Routine Care Of Healthy Patient, 'common Symptoms'
advertisement

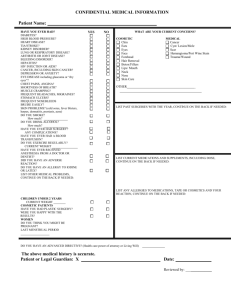
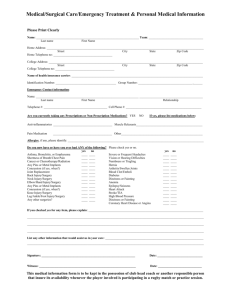
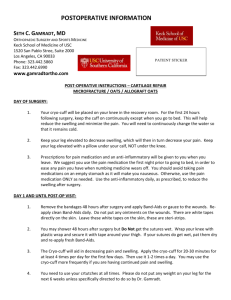
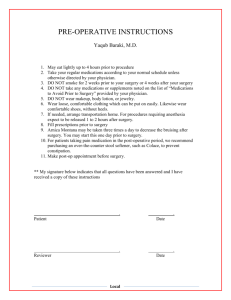
Gen Med Board Review – Part I Screening/Vaccines, Common Symptoms, Musculoskeletal complaints, Red Eye, Perioperative Medicine April 18, 2013 A 62-year-old woman is evaluated during a follow-up visit for hypertension. She has no complaints and is monogamous with her husband of 35 years. Her only current medication is hydrochlorothiazide. On physical examination, blood pressure is 136/72 mm Hg and weight is 62 kg (136 lb). Physical examination is normal. Total cholesterol is 188 mg/dL and HDL cholesterol is 54 mg/dL.. She received an influenza vaccination 3 months ago and a herpes zoster vaccination 1 year ago. Her last Pap smear was 14 months ago and it was normal, as were the previous three annual Pap smears. Which of the following is the most appropriate health maintenance option for this patient? Abdominal ultrasonography Dual-energy x-ray absorptiometry Pap smear Pneumococcal vaccine A 57-year-old man is evaluated during a routine examination. He has hypertension, which is well controlled on hydrochlorothiazide. He asks if he should get a prostate-specific antigen (PSA) test. Medical history is otherwise unremarkable. There is no family history of cancer. Blood pressure is 132/86 mm Hg, and results of the physical examination are unremarkable. Which of the following is the best prostate cancer screening option for this patient? 1. 2. 3. 4. Discuss the risks/benefits of screening for prostate CA Order PSA testing Order PSA testing and perform DRE Perform DRE Screening Recommendations • Blood Pressure: – • DM2: – – • abdominal ultrasound once in men >65 and smoking hx Colon CA: – – • DXA at 65yo then q2y or <65 if RF (wt <70, FHx, smoking, EtOH, steroids/RA, previous fx) q5y AAA: – • Male >35 or anyone >20 with RFs Then every 5 years for low risk people Osteoporosis: – – • Start >45y or <45 with RFs Screen yearly if RFs or q3y if no RFs Hyperlipidemia: – – • Every 2 yrs if wnl; yearly if pre-HTN Start age 50, unless AA then start at 45 Colonoscopy q10y, FOBT q1y, or flex sig q5 + FOBT q3 Routine screening for the following: – – – EtOH/tobacco dependence Depression Obesity USPSTF vs ACS Cervical Cancer Age 21-29: screen with cytology q3 years Age 30-65: cytology q3y or cytology + HPV q5y Stop screening at age 65 if adequate prior screenings and not high risk Breast Cancer Biannual mammograms age 50-74 No clinical breast exams (CBEs) Mammograms yearly starting age 40 CBEs q3 yrs starting age 20, then yearly at age 40 Prostate Cancer Does not recommend PSA testing Men should make informed decision with their doctor about whether to check PSA A 68-year-old woman is evaluated during a routine examination. She states that last year she had a painful rash on the right side of her back that was self-limited. She does not recall a history of childhood chickenpox. She takes no medications and has no allergies. Vital signs are normal and the physical examination is unremarkable. Complete blood count, liver enzymes, and serum chemistry studies are all normal. She is scheduled to receive her annual influenza vaccination today. Which of the following is the most appropriate vaccine administration strategy to prevent herpes zoster in this patient? 1. 2. 3. 4. 5. Zoster vaccination if negative for varicella antibodies Zoster vaccination if positive for varicella antibodies Zoster vaccination now Zoster vaccination now and in 6 months Zoster vaccination not indicated Live Vaccine Dead Vaccine Immunizations Hepatitis A Hepatitis B • MSM, illicit drug users, chronic liver disease, food handlers, travelers • 2 doses • all patients – esp those in HepA group, healthcare workers, HIV, CKD, inmates • 3 doses MMR • • all patients 2 doses HPV Influenza - IM • Females 11-26 • Males 11-21 (unless MSM, HIV, immunocomp, then until age 26) • 3 doses Pneumococcal Meningococcal • All pts 65 and older • younger if: Alaskan, SNF residents, immunocomp, chronic disease, asplenic • one time booster if 1st vaccine >5yr ago and given before age 65 • young adults in closed quarters, asplenia, complement deficiency, travelers • MCV4 – one dose (ages 11-55) • MPSV4 – 2 doses (ages <11 or >55) Tetanus and Wounds: • all adults – esp if >50yo, health care workers, chronic disease • contraind: GBS, egg allergy Intranasal Tetanus • Td – all patients • 3 doses, then booster every 10 yr • sub one booster for Tdap (age 19-64) – or can give 2y after last Td Zoster • 60 or older regardless of shinges hx (most benefit 60-69) • Vaccine Status Unknown or <3 total doses: Vaccinate now • Clean minor wound and 3+ known vaccines – Revaccinate if last was >10yr ago • Other wounds and 3+ known vaccines – Revaccinate if last vaccine 5+ yr ago A 52-year-old woman is evaluated at a routine appointment and seeks advice on smoking cessation. She smokes one and one half packs of cigarettes daily and wants help to stop. She has tried to stop smoking on three previous occasions, each time using nicotine replacement therapy, and she would like to try something different. She has a seizure disorder that is well controlled on valproate. In addition to brief smoking cessation counseling, which of the following is the most appropriate pharmacologic therapy to offer? 1. 2. 3. 4. Bupriopion Nortriptyline Sertraline Varenicline Smoking Cessation Agent Success SEs, contraind Pregnancy Nicotine replacement (gum, patch, spray, inhaler, lozenge) Increases cessation 1.5x over control Avoid in recent MI, arrhythmia, unstable angina Safety unclear Bupropion Increases cessation 2x over control Avoid in seizure disorder and eating disorder; associated with HTN Safety unclear Varenicline (Chantix) Increases cessation 3.5x control and 2x over bupropion Associated with drowsiness, fatigue, sleep disturbance, depressed mood, suicidal thoughts, constipation Safety unclear A 52-year-old man is evaluated for a daily cough for the past 6 months. It occurs throughout the day and occasionally at night, but he does not notice any specific triggers. There is occasional production of small amounts of white sputum but no hemoptysis. He does not have any known allergies, has no new pets or exposures, and does not smoke. He does have nasal discharge. He has not noticed any wheezing and has no history of asthma. He has no symptoms of heartburn. He has had no fever, weight loss, or foreign travel, and takes no medications. Vital signs are normal. There is no cobblestone appearance of the oropharyngeal mucosa. Lungs are clear to auscultation. A chest radiograph is normal. Which of the following is the most appropriate management for this patient? 1. 2. 3. 4. 5. Antihistamine/decongestant combination CT scan of chest Inhaled fluticasone Proton-pump inhibitor Pulmonary function testing Chronic cough • • • • 3-8 weeks = subacute >8 weeks = chronic Etiologies (often multifactorial): 1. Upper Airway Cough Syndrome (post-nasal drip) • Exam may show “cobblestoning” or mucous down oropharynx • Tx: 1st generation antihistamine + decongestant (if not due to sinusitis) • If allergic rhinitis, add daily nasal steroid 2. Asthma (cough-variant) • May present with cough associated with exercise or exposure to cold • If dx uncertain, do methacholine challenge 3. GERD • Consider trial of PPI 4. Other: • Nonasthmatic Eosinophilic bronchitis – Normal CXR, spirometry, and negative methacholine challenge – Dx: Bronch – Tx: avoid occupational exposure; Inhaled steroids • Chronic bronchitis • Bronchiectasis – voluminous purulent sputum production • Smoking • Meds (ACEI, NSAIDs, bblockers, macrobid, cellcept) Approach to workup: – History to try and identify cause – Medication review – CXR (99% due to UACS, Asthma, or GERD in nonsmokers with normal CXR and not on ACEI) An 89-year-old woman is evaluated for dizziness that she has had for the past year, mainly while standing and ambulating. The dizziness is described as a sense of unsteadiness. The symptoms can last for minutes to hours, and she has at least 4 to 5 episodes per day. There are no reproducible activities that cause the dizziness. She does not describe hearing loss, headache, diplopia, or other motor or sensory symptoms. Medical history includes type 2 diabetes mellitus, hypertension, hyperlipidemia, osteoporosis, and mild dementia. Current medications are hydrochlorothiazide, ramipril, simvastatin, metformin, insulin glargine, low-dose aspirin, and donepezil. Exam reveals no orthostasis. Cardiopulmonary exam is normal. The patient has a positive Romberg sign and is unsteady on tandem gait. Rapid alternating movements are slowed. The patient has a corrected visual acuity of 20/50 in the right eye and 20/70 in the left eye. Vibratory sense and light touch are diminished in a stocking pattern in the lower extremities, and ankle jerk reflexes are 1+. She has no motor abnormalities and no cranial nerve abnormalities. A DixHallpike maneuver does not elicit vertigo or nystagmus. Labs are wnl. Which of the following management options is the best choice for this patient? 1. 2. 3. 4. Brain MRI Meclizine Physical therapy Replace aspirin with aspirin/extended-release dipyridamole A 79-year-old man is evaluated in the emergency department for vertigo that began suddenly about 1 hour ago, associated with severe nausea and vomiting. He noticed that he could not seem to sit up straight and could not walk without assistance. The patient denies confusion, motor weakness, hearing loss, dysarthria, diplopia, fever, or paresthesias. Medical history is remarkable for hypertension, hyperlipidemia, and type 2 diabetes mellitus. Current medications are lisinopril, atorvastatin, low-dose aspirin, insulin glargine, metformin, and atenolol. There are no allergies. The patient demonstrates unsteadiness on finger-to-nose testing in the right upper extremity and is unable to walk more than a few steps or stand without assistance. Motor strength and reflexes are normal. Visual acuity and visual fields are normal. Otoscopic and hearing exams normal. Cardiopulmonary examination is normal. Which of the following in the most appropriate management option for this patient? 1. Admit for telemetry 2. Brain MRI 3. Intravenous methylprednisolone 4. Oral meclizine A 61-year-old man is evaluated for dizziness that started about 2 days ago while he was looking over his shoulder. He describes the symptoms as “room spinning” dizziness and mild nausea. The symptoms resolved within several minutes when he lay back on the couch and was perfectly still. They recurred several hours later while turning in bed and the next day while backing out of his driveway. He denies diplopia, slurred speech, confusion, motor weakness, paresthesias, tinnitus, antecedent infection, or hearing loss. He has no other medical problems and takes no medications. Vital signs are normal. The cardiopulmonary examination is normal. Peripheral nystagmus and reproduction of symptoms on the Dix-Hallpike maneuver when the head is turned right are demonstrated. There are no focal neurologic defects. Visual acuity and hearing are normal. Which of the following management options is the beset choice for this patient? 1. Audiometry 2. Brain MRI with magnetic resonance angiography 3. Cardiac event monitor recording 4. Epley canalith repositioning maneuver 5. Methylprednisolone Vertigo 1. VERTIGO – “room spinning” 2. PRESYNCOPE – nearly losing consciousness 3. DISEQUILIBRIUM – unsteady while Nonspecific DIZZINESS Disequilibrium Presyncope walking • Usually multifactorial/in elderly • DDx: deconditioning, peripheral neuropathy, poor hearing or eyesight, polypharmacy 4. NONSPECIFIC – none of the above • DDx: hypoglycemia, medications, thyroid dz, anemia, stress, psychiatric Vertigo – “room is spinning” 1. Nystagmus – vertical vs horizontal 2. Episodic or Persistent 3. How long does it last? 4. Associated with hearing loss? Tinnitus? Nausea? – Central Cause: • Nystagmus vertical or changes direction with different head positions; no latent period; longer duration; non-fatiguing • Etiologies: – Tumors (<1%) – Acoustic Neuromas » Unilateral hearing loss/tinnitus – Posterior circulation CVA » Persistent vertigo; other symptoms (neurologic, nausea/vomiting) – Migraine headaches – Peripheral (vestibular) Cause: • Nystagmus horizontal or rotary; delayed onset; lasts seconds; fatigues with repetition • Vertigo symptoms more pronounced than central causes • Often associated with recent URI, hearing loss, tinnitus, or head trauma • 3 major etiologies: – BPPV – Vestibular Neuronitis – Meniere Disease Vestibular Vertigo Cause Nature Duration Hearing loss? Tinnitus? Nausea? Treatment BPPV Otolith debris in semicircular canals Episodic Minutes No No No Eply maneuver +/- vestibular suppressants Vestibular Neuronitis Post-viral inflammation of vestibular portion of CN VIII Persistent Days No No Yes Can add steroids; meclizine if it persists Meniere’s Endolymphatic hydrops (too much fluid in canals) Episodic Yes (unilateral) Yes (typically unilateral) Yes Avoid triggers (salt, caffeine, EtOH), rehab, vestibular suppressants Minuteshours Vestibular suppressants: anticholinergics, antihistamines, benzos A 36-year-old woman is evaluated in the emergency department after collapsing suddenly while waiting in line at a county fair on a hot summer day. The patient states she felt nauseated and became diaphoretic and lightheaded. She sat on the ground and then lost consciousness. According to her son, she was unconscious for less than a minute, exhibited some twitching movements when she first lost consciousness, but had no incontinence or symptoms of confusion upon awakening. She had no further symptoms upon regaining consciousness. She has a history of hypertension and hyperlipidemia. On exam, temperature is normal, blood pressure is 142/80 mm Hg (supine) and 138/78 mm Hg (standing), pulse rate is 84/min (supine) and 92/min (standing). Cardiac and neurologic examinations are normal. An ECG is normal. Which of the following is the most appropriate management option for this patient? 1. 2. 3. 4. 5. Echocardiogram Electroencephalogram Exercise stress test Tilt-table testing No further testing 20% 1 20% 20% 2 3 20% 4 20% 5 Syncope Cardiac Neurogenic Outflow obstruction Neurocardiogenic (Vasovagal) Seizure Ischemia (rare) Severe AS CVA (very rare) HOCM PE Orthostasis Arrhythmias Meds Non-neurogenic Neurogenic MS Venous pooling ALS • Vasovagal: • • • Volume depletion Polyneuropathy Adrenal insufficiency Specific trigger leads to increased parasympathetic (vagal) tone (decreased HR and increased BP) Prodrome of nausea, lightheadeness, dizziness, diaphoresis Dx: clinical or tilt-table test Tx: trigger avoidance; supine with legs up when it occurs; compression stockings, tilt training, bblockers if frequent episodes A 42-year-old man is seen in the office for low back pain that began after lifting a box 5 days ago. The pain is moderately severe, and almost any movement makes it worse. He tried lying down and experienced some, but not complete, relief. He reports that he has had no trouble urinating. He has no other symptoms and is otherwise healthy. Physical examination reveals tenderness over the L4 paravertebral musculature bilaterally. His gait is slow owing to the pain. Results of a straight-leg-raising test are normal. There are no signs of motor weakness or sensory loss, including perineal sensation. Deep tendon reflexes are normal bilaterally. Which of the following is the best initial management option? 1. 2. 3. 4. 5. Acetaminophen Epidural corticosteroid injection MRI of lumbar spine Plain radiographs of the lumbar spine Strict bed rest 20% 1 20% 20% 2 3 20% 4 20% 5 Acute Back Pain • Decide which type: 1. Nonspecific (90%) • • • 2. Associated with radiculopathy/spinal stenosis (6%) • • 3. • Will resolve on their own Tx conservatively with Tylenol or NSAIDs No imaging needed Radiating pain down leg(s), + straight leg raise If pain >1 month, then get MRI Due to spinal pathology – need further imaging Red flags = need further imaging – Cancer – Hx of malignancy and new onset low back pain; unexplained weight loss – MRI – Infection – Hx of IVDU, fever, recent infxn – MRI – Cord Compression – Hx of malignancy, new neuro deficits – MRI of all spinal levels – Cauda Equina Syndrome (L1-S5 nerve roots) – Urinary retention, fecal incont, saddle anesth, motor deficits at multiple levels - MRI – Compression Fx – Hx of osteoporosis or steroid use + fall – plain xray A 47-year-old man is evaluated in the office for right lateral shoulder pain. He has been pitching during batting practice for his son’s baseball team for the past 2 months. He has shoulder pain when lifting his right arm overhead and also when lying on the shoulder while sleeping. Acetaminophen does not relieve the pain. On physical examination, he has no shoulder deformities or swelling. Range of motion is normal. He has subacromial tenderness to palpation, with shoulder pain elicited at 60 degrees of passive abduction. He also has pain with resisted mid-arc abduction but no pain with resisted elbow flexion or forearm supination. He is able to lower his right arm smoothly from a fully abducted position, and his arm strength for abduction and external rotation against resistance is normal. Which of the following is the most likely diagnosis 1. 2. 3. 4. 5. 20% 20% 20% 2 3 20% 20% Adhesive capsulitis Bicipital tendinitis Glenohumeral arthritis Rotator cuff tear (complete) Rotator cuff tendinitis 1 4 5 Shoulder • Rotator Cuff Tendonitis – most common shoulder complaint – Subacromial pain on exam and impingement when reaching overhead – No need to image – Treatment: • first 2 weeks – subacromial injection, NSAIDs, ROM exercises • >2 weeks - add PT • Rotator Cuff Tear – Weakness, loss of function, + drop arm test • Bicipital tendonitis – Pain with forced supination of hand when elbow flexed 90 degrees • Adhesive Capsulitis (Frozen Shoulder) – Progressive decreased ROM (due to stiffness and not so much limited from pain) – loss of rotation and abduction • GH osteoarthritis – Gradual anterior pain and stiffness – Crepitus and anterior joint line tenderness on exam A 72-year-old woman is evaluated for a 8-month history of aching in her left wrist that keeps her awake at night. She is in a knitting group and has found it increasingly difficult to perform fine hand movements. Using the Katz hand diagram, the patient indicates the presence of sensory changes in the first through third digits. She also reports wrist pain with sparing of the palm and some pain into the forearm. Her only medication is acetaminophen. On physical examination, there is weakness of thumb abduction, hypalgesia in a median nerve distribution, and thenar atrophy. Vascular assessment in the hand is normal. A nerve conduction study and electromyogram demonstrate medial neuropathy. Which of the following is the most appropriate management option for this patient? 1. 2. 3. 4. 5. Corticosteroid injection NSAIDs Surgery Ultrasound treatment Wrist splint 20% 1 20% 20% 2 3 20% 4 20% 5 Carpal Tunnel • Predisposing Factors: – Pregnancy, RA, OA, Hypothyroidism, Obesity, carpal fracture • Treatment: – Conservative measures (none has been proven superior or first line) • Splinting, NSAIDs, US, PT • Short-term prednisone vs steroid injections – Surgery – first line if evidence of severe neuromuscular compromise A 48-year-old overweight woman is evaluated for buttock pain. She began jogging 1 week ago to lose weight. Over the last 2 days, pain has developed deep in the left gluteal area. The pain is an ache that she first noticed while lying in bed on her left side. It was somewhat relieved by lying on her right side. The pain has become severe enough that she avoids putting weight her left leg while climbing stairs. The pain does not radiate. Ibuprofen has helped the pain somewhat. She is on no other medications. On physical examination, there is tenderness elicited over the left sciatic notch when pressure is applied with the thumb. When lying on the right side, abduction of the leg is painful. The hip joint has no pain with full range of motion. There is no tenderness in the groin or over the lateral thigh, and FABER (Flexion, ABduction, and External Rotation of the hip) test results are normal. Reflexes and the straight-leg-raising test are normal. 25% 25% 25% 2 3 25% Which of the following is the most likely diagnosis? 1. 2. 3. 4. Left hip osteoarthritis Left trochanteric bursitis L4-L5 disk herniation (Sciatica) Piriformis syndrome 1 4 Hip • • • • • Osteoarthritis = true hip pain (groin, worse with weight bearing) Trochanteric Bursitis = bursal pain (lateral, worse with lying on that side) Piriformis Syndrome = compression of sciatic nerve by piriformis muscle – Seen in prolonged sitting or carrying large wallet in back pocket – Tx: Stretching/NSAIDs Osteonecrosis – RFs: steroids, sickle cell disease – Dx: MRI (if early disease); xray (if late disease) Meralgia Paresthetica = entrapment of lateral cutaneous nerve under inguinal ligament – Decreased sensation over lateral thigh – clues: obesity, belt, tight clothes A 35-year-old woman is evaluated in the office for a 5-day history of acute right knee pain that began when she hopped down from the bed of a truck, twisting her knee. She experienced a popping sensation and a gradual onset of knee joint swelling over the next several hours. Since then, she has continued to have moderate pain, particularly when walking up or down stairs. She reports no locking or giving way of the knee or any previous knee injury. On physical examination, the right knee has a minimal effusion with full range of motion. The medial aspect of the joint line is tender to palpation. Maximally flexing the hip and knee and applying abduction (valgus) force to the knee while externally rotating the foot and passively extending the knee (McMurray test) result in a palpable snap but no crepitus. Which of the following is the most likely diagnosis? 1. 2. 3. 4. 25% 25% 25% 2 3 25% Anserine bursitis Anterior cruciate ligament tear Meniscal tear Patellofemoral pain syndrome 1 4 Knee • Acute Trauma – “popping”, effusion – ACL – sudden twist + hyperextension • Anterior drawer or Lachman test – PCL – trauma to flexed knee – LCL/MCL – medial/lateral force without twisting – Meniscus – McMurray test = 97% specific • Patellofemoral Syndrome – Females <45yo – Reproducing the pain by firmly moving the patella along the femur confirms the diagnosis • Iliotibial Band Syndrome = inflammation of distal part of iliotibial ligament – “Knife-like” lateral pain that occurs with repetitive flexion/extension • Bursitis – Pes anserine, prepatellar, suprapatellar A 25-year-old woman presents for evaluation of recurrent, bilateral eye pain and redness. Symptoms began several months ago without a specific inciting event. With each episode, she has deep or boring pain that is constant and has awakened her from sleep. She has had photophobia, tearing, and decreased vision during the episodes. Vital signs are normal. Visual acuity is 20/40 bilaterally. There is photophobia. The pupils are equal, round, and reactive to light. Extraocular movements are intact but painful. The corneas appear clear. On the lateral aspect of both eyes, there is a localized area of raised erythema, with superficial blood vessels coursing over top of erythema but no white sclera visible between the blood vessels. There is no discharge or crusting of the lids. Which of the following is the most likely diagnosis regarding her eyes? 20% 1. 2. 3. 4. 5. 20% 20% 2 3 20% 20% Episcleritis Scleritis Subconjunctival hematoma Uveitis Viral conjunctivitis 1 4 5 • Red eye Conjunctivitis = most common cause – Allergic • Recurrent, seasonal • Itchy eyes with watery discharge; diffuse redness (bilateral) • Tx: topical antihistamine, cool compress, topical NSAIDs (3 days) – Viral • Typically starts in one eye along with URI, then moves to the other side • Tearing, foreign body sensation, can have LAD • Very contagious; Adenovirus = most common • Tx: supportive, cold compress PRN – Bacterial • Diffuse unilateral redness with AM mucopurulent discharge • Pneumococcus = most common (followed by Staph, Hemophilus) – Tx: topical Abx • If suspect GC or Chlamydia as cause, need referral to ophtho + Abx Red Eye • Urgent call to Ophtho if: – • Scleritis – – – – • Pain, Decreased vision, seeing “halos”, photophobia **urgent ophtho referral Iritis (or Iridocyclitis or Uveitis) – – • Spontaneous, PAINLESS; associated with recent straining/coughing Self-limiting in 2 weeks Keratitis = Corneal inflammation – – • Still able to see white sclera between prominent vascular markings Self-limited; not associated with underlying disease Subconjunctival Hemorrhage – – • Cannot see white sclera between prominent vascular markings Severe constant ocular pain worse with EOM, photophobia **associated with CVD and rheum disease **urgent referral as can lead to orbital rupture!! Episcleritis – – • Vision changes, Photophobia, Pupillary changes, pain, trauma, anytime cornea involved (“kerato”) Intense pain, photophobia, ciliary injection, irregularly shaped pupil May indicate infection or underlying CVD/Rheum disease Acute Angle-Closure Glaucoma – Pain, seeing “halos”, HA, n/v, dilated pupil 68-year-old woman is evaluated in the emergency department for difficulty seeing out of her left eye. The symptoms were first present upon awakening 45 minutes earlier. She describes her vision as “looking through a dark veil.” Her right eye is unaffected. There is no associated pain, head-ache, muscle aching, or difficulty chewing, and no trauma or history of a similar episode. She has hypertension, hypercholesterolemia, and chronic open-angle glaucoma. Current medications are ramipril, hydrochlorothiazide, atorvastatin, aspirin, and timolol ophthalmic solution. 20% 20% 20% 2 3 20% 20% Vital signs are normal. Visual acuity in the right eye is 20/30, corrected for glasses; in the left eye, visual acuity is restricted to finger counting. Both globes are nontender to palpation. There is no conjunctival injection. Ophthalmoscopic examination of the right eye is normal. Findings in the left eye are shown. Venous pulsations are noted. Pupils are equal. The right pupil reacts to direct and consensual light stimulus. The left pupil has sluggish response to direct light, but normal consensual response. Cardiac and neurologic examinations and electrocardiogram are normal. Which of the following is the most likely diagnosis? 1. Acute angle-closure glaucoma 2. Acute occipital stroke 3. Central retinal artery occlusion 4. Central retinal vein occlusion 5. Retinal detachment 1 4 5 Eye Emergencies • • • • • • Acute Angle Closure Glaucoma Central Retinal Artery Occlusion – Due to embolus or thrombus – Unilateral/painless, “looking through a dark veil” – Pale retina on exam with “cherry red spot” near fovea – Tx: emergent surgery; optic massage x15 min Central Retinal Vein Occlusion – Presents similarly to CRAO but retina with “cotton wool spots” or “blood & thunder” Giant Cell Arteritis – Abrupt vision loss due to thrombosis of posterior ciliary or ophthalmic artery – Associated with PMR – Tx: emergent steroids Retinal Detachment – Seeing “flashes of light”, multiple floaters, decreased vision and metamorphopsia (wavy vision) Cellulitis (Preseptal vs Septal) – CT to assess depth of infection – Preseptal (not involving orbit): Usually due to contiguous spread of skin or sinus infection – Septal (involving orbit): usually from dental, soft tissue infection • Can be complicated by meningitis or cavernous sinus thrombosis A 64-year-old woman is evaluated during a health maintenance examination. She has hypertension and hypercholesterolemia. She has no symptoms to report. She is a current smoker, with a 20 pack-year history. Current medications are atenolol and hydrochlorothiazide. Vital signs are normal. BMI is 28. Funduscopic examination reveals bright, yellow, refractile deposits scattered in the retina of the right eye, with approximately five deposits seen on direct ophthalmoscopy. The left fundus appears normal. On visual acuity testing, near vision is 20/20 with reading glasses, and distance vision is 20/25 for both eyes. The remainder of the physical examination is normal. A lipid panel obtained prior to today’s visit reveals a total cholesterol of 190 mg/dL ; LDL cholesterol of 120 mg/dL; HDL cholesterol of 40 mg/dL; and triglycerides of 150 mg/dL. 25% 25% 25% 25% Which of the following is the most effective management option for this patient’s ocular findings? 1. 2. 3. 4. Antioxidant supplements Atorvastatin Lower blood pressure to below 130/85 mm Hg Smoking cessation 1 2 3 4 A 78-year-old woman is evaluated because of concerns about her ability to drive. She has trouble seeing on bright, sunny days and also at night because of the glare from headlights of oncoming cars. The patient has type 2 diabetes mellitus and a 55-pack-year smoking history. Her current medications include metformin and glipizide. This patient’s history is most suggestive of which of the following ophthalmologic disorders? 1. 2. 3. 4. 5. Age-related macular degeneration Cataracts Presbyopia Primary open-angle glaucoma Proliferative diabetic retinopathy 20% 1 20% 20% 2 3 20% 4 20% 5 Macular Degeneration/Glaucoma/Cataracts • Macular Degeneration = central vision loss – “Dry” – 80% - gradual vision loss • “Drusen” (amorphous deposits) form behind retina – “Wet” – 20% - more rapid and profound • Neovascularization near macula – RFs: age, smoking – Tx: stop smoking! • • For “wet”, can try photodynamic tx or laser photocoagulation Primary Open Angle Glaucoma = peripheral vision loss – Due to obstruction in outflow of aqueous humor from anterior chamber – Initially asymptomatic with loss of periph vision, but can lead to progressive optic neuropathy and elevated IOP – Increased cup:disc ratio (>0.5) – Treatment (often with systemic side effects) • • • • Bblockers (timolol) -> decrease inflow A2-agonists (brimonidine) -> decrease inflow and increase outflow PG analogues (latanoprost) -> increase outflow Cataracts = contrast/glare issues – – – – Due to opacification of lens Symptoms: glare, reduced vision, loss of contrast, decreased illumination RFs: age, smoking, UV light, DM, steroids Tx: surgery Macular Degeneration Glaucoma Cataracts A 60-year-old woman is evaluated before undergoing a lumpectomy for breast cancer tomorrow. Medical history is significant for hypertension, type 2 diabetes mellitus, chronic kidney disease, a myocardial infarction 2 years ago, and a stroke 1 year ago with residual right-sided hemiparesis. The patient does not have chest pain or shortness of breath and is otherwise asymptomatic. She uses a walker to ambulate. Current medications are metoprolol, simvastatin, furosemide, losartan, nifedipine, insulin glargine, insulin aspart, and aspirin. On physical examination, temperature is 36.8 °C, BP 160/90 mm Hg, HR 66/min, and RR is 25% and 25% 25%pedal edema. 25% 14/min. Examination is normal except for right-sided hemiparesis mild bilateral Pertinent laboratory results: blood urea nitrogen, 35 mg/dL; creatinine, 2.2 mg/dL; random glucose, 180 mg/dL; hemoglobin A1c, 8.1%. An ECG shows normal sinus rhythm, left ventricular hypertrophy, first-degree atrioventricular block, and nonspecific ST-T wave changes. Which of the following is the most appropriate preoperative management? 1. Postpone surgery until blood pressure is below 140/90 mm Hg 2. Postpone surgery until dobutamine stress echocardiography is obtained 3. Postpone surgery until fasting glucose is below 110 mg/dL (6.11 mmol/L) 4. Proceed with surgery 1 2 3 4 A 65-year-old man with a 2-year history of severe osteoarthritis of the right knee is evaluated before undergoing total knee replacement surgery. Until 1 month ago, the patient was able to walk four or more blocks and four flights of stairs but now can only walk one block because of severe knee pain. He has a 3-year history of occasional chest pain that occurs less than once each month and develops only after walking too quickly. There has been no change in the severity or frequency of the chest pain and no dyspnea. Medical history is significant for a myocardial infarction 4 years ago, type 2 diabetes mellitus, and hypertension. Current medications are metoprolol, fosinopril, atorvastatin, insulin glargine, metformin, and aspirin. 20% 20% 20% 20% 20% Blood pressure is 140/80 mm Hg, pulse rate is 60/min. BMI is 30. There is no jugular venous distention. The lungs are clear. There are no murmurs or gallops. Serum creatinine is 1.5 mg/dL (132.6 µmol/L). An electrocardiogram shows normal sinus rhythm with Q waves in leads II, III, and aVF; nonspecific ST-T wave changes; and left ventricular hypertrophy. A chest radiograph is normal. Which of the following is the most appropriate preoperative cardiac testing? 1. 2. 3. 4. 5. Coronary angiography Dobutamine stress echocardiography Exercise (treadmill) thallium imaging Resting two-dimensional echocardiography No additional testing is indicated 1 2 3 4 5 A 70-year-old man with severe disability due to claudication in his right leg and a 2-month history of increasingly frequent chest pain undergoes preoperative cardiovascular evaluation prior to elective right femoropopliteal bypass graft surgery. The patient can only walk one block because of claudication and chest pain despite adequate medical treatment. Medical history is significant for coronary artery disease, a myocardial infarction 4 years ago, hypertension, and type 2 diabetes mellitus. The patient underwent left femoropopliteal bypass graft surgery 2 years ago under general anesthesia without complications. He has a 55 pack-year smoking history but stopped smoking 2 years ago. Current medications are20% metoprolol, 20%atorvastatin, 20% amlodipine, 20% 20% fosinopril, isosorbide mononitrate, insulin glargine, insulin aspart, and aspirin. Vital signs are normal. There is no jugular venous distention. Cardiopulmonary examination is normal. Pulses in the right calf are decreased. There is no calf tenderness and no peripheral edema. An electrocardiogram shows Q waves in the inferior leads. Which of the following is the best preoperative management? 1. 2. 3. 4. 5. Coronary angiography Dipyridamole nuclear imaging stress testing Dobutamine stress echocardiography Two-dimensional echocardiography No testing needed 1 2 3 4 5 Perioperative Guidelines Emergent? Yes Proceed with surgery and optimize meds if time No Active cardiac conditions? Yes No Delay surgery for further eval/tx Low risk surgery? Yes No Adequate functional capacity (4 METs) without symptoms? Proceed with surgery Yes Proceed with surgery Clinical RFs 0 Proceed 1-2 proceed; consider periop heart rate control and/or noninvasive testing Intermediate risk Proceed; consider periop HR control and/or noninvasive testing >3 Type of surgery? Vascular Noninvasive testing Perioperative Guidelines - Definitions • Active Cardiac Conditions: – MI <30d, UA or severe angina, decompensated CHF, arrhythmias, severe valve disease • Low Risk Surgery: – Endoscopic, superficial, breast, ambulatory, cataract • 4 METs: – Flight of stairs, walk up a hill, walk 4 mi/hr • Clinical RFs: – Hx of heart disease, Hx of CHF, hx of stroke, DM2, renal insufficiency • Intermediate Risk Surgery – Intraperitoneal, intrathoracic, endovascular aortic aneurysm, CEA, head/neck, orthopedic, prostate • Vascular Surgery – Peripheral vascular, major valve surgery