Monmouth Ocean Hospital Consortium (MONOC)
advertisement

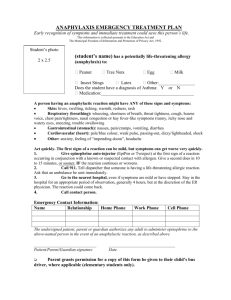
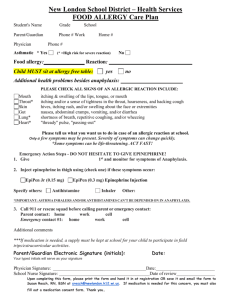
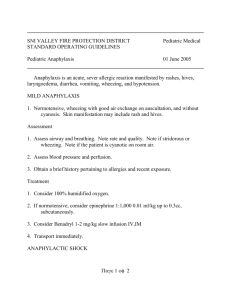
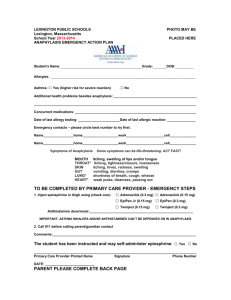
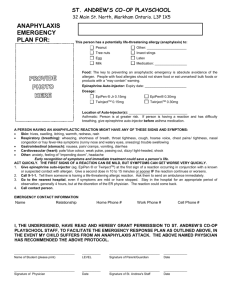
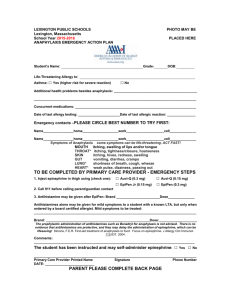
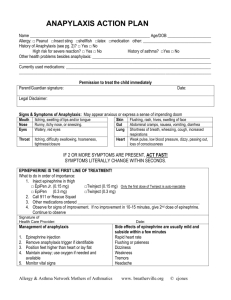
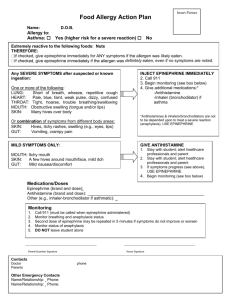
New Jersey’s Hospital Service Corporation Epinephrine Auto Injector A Lifesaving Tool Now In the Hands of the EMT-B EMS EDUCATION © MONOC 2007 Epinephrine Auto Injector A Lifesaving Tool Now In the Hands of the EMT-B Immediate Treatment = Saved Lives OBJECTIVES At the conclusion of this program the EMT-B will have the cognitive, psychomotor, and affective skills that are needed to properly administer an Epinephrine Auto Injector to a prehospital patient who is having an Anaphylactic reaction in accordance with the NJ OEMS Policy OBJECTIVES • Describe the scope of the problem • Define Anaphylaxis • Explain the Epinephrine Auto Injector Policy • Define role and responsibility of the Medical Director, the First Aid Squad, the individual EMT-B, OEMS and MONOC in this program • Explain the importance of FAST care OBJECTIVES • Describe progressive pathophysiology of Anaphylactic Reactions • Describe the Signs and Symptoms that an Anaphylaxis patient presents with • List the common “triggers” that lead to an Anaphylactic Reaction • List conditions that mimic Anaphylaxis OBJECTIVES • Describe the actions, side effects, route, and injection site for Epinephrine Auto Injector • State when to use the pediatric dose of Epi and how to estimate patient weight and age • Describe the procedure to follow to check for device expiration and drug clarity • State how to safely and properly dispose of an Epinephrine Auto Injector OBJECTIVES • Describe proper patient assessment by an EMT-B for a Anaphylaxis patient • Explain the Procedure for an EMT-B to follow to administer an Epinephrine Auto Injector • Describe common errors in Auto Injector use • Describe proper Documentation after use OBJECTIVES • Describe the proper method to deliver Ventilations to patients of all ages • Explain the proper procedure for use of Basic Airway Adjuncts by EMT-B • Describe how to deliver Quality CPR • Explain how the EMT-B can assist ALS • State where to find more information DEFINITION WHAT IS • Anaphylaxis ? Systemic allergic reaction Affects body as a whole Multiple organ systems may be involved • Onset generally acute • Manifestations vary from mild to fatal Now let us take a look at New Jersey’s Epinephrine Auto Injector Policy Definitions & OEMS Policy The Medical Director Responsibilities of the Squad Responsibilities of each EMT-B DEFINITIONS • National EMT-B Curriculum allows EMTs to ASSIST a patient with EpiPen • The OEMS Policy allows EMTs to ADMINISTER an EpiPen to the patient ASSIST • The medication must be prescribed to the patient • The patient carries the medication with him ADMINISTER • The medication will be prescribed to the squad • The medication is carried on the ambulance In either case the extent to which the patient or EMT-B participate with the use of the EpiPen can vary significantly. The EMT-B may just watch patient use the EpiPen or the EMT-B may actually perform the “stick”. NJ Epinephrine Auto Injector Policy The National Standard Curriculum for EMT-B provides that EMT-Basic’s are trained to recognize clinical signs and symptoms of anaphylactic shock and establishes that it is within the scope of practice of the EMT-Basic to assist a patient in the self-administration of a patient's Epinephrine Auto Injector NJ Epinephrine Auto Injector Policy • PL 2003, c,1., N.J.S.A. 26:2K-47.1, presently authorizes OEMS to certify the NJ EMT-B to administer the epinephrine auto injector to patients suffering from anaphylactic shock • NJ OEMS recognizes that the expeditious implementation of this law would have an immediate benefit to the general public • Accordingly, OEMS shall now authorize the NJ certified EMT-B to administer the epinephrine auto injector to patients in accordance with the following policies and protocols NJ Epinephrine Auto Injector Policy • The EMT-B is allowed to administer an • • • Epinephrine Auto Injector to prehospital patients only before an ALS Unit arrives Once the ALS Unit arrives the Paramedics will administer Epinephrine from their stock NJ Paramedics can administer Epinephrine immediately under Standing Orders The Paramedics Medical Control Physician will provide on line medical control after the Paramedics complete the Standing Orders NJ Epinephrine Auto Injector Policy • Only EMT-Basics meeting the following • • requirements are authorized by OEMS to carry on their ambulance and administer epinephrine auto injectors to patients Only EMT-Basics acting with the general authority of a physician medical director, will be allowed to administer epinephrine auto injectors to prehospital patients BLS agencies must complete an approved training program prior to obtaining or using epinephrine auto injectors NJ Epinephrine Auto Injector Policy • Only EMT -Basics who are members of BLS agencies that are registered with NJ OEMS may possess or administer the Epinephrine Auto Injector to patients • OEMS will monitor the EMT-B use of epinephrine auto injectors according to these policies and will take corrective action as is deemed necessary for the safe implementation of this policy Medical Director DR. MICHAEL MARCHETTI • Provides Off-line Medical Control • Will provide the prescriptions for the Epinephrine Auto Injectors • Responsible for all clinical aspects of the MONOC EpiPen Program • Training and Quality Assurance The First Aid Squad • • • • Register with OEMS Contract with MONOC Initial training at FAS location Fill Medical Director’s prescription for the Epinephrine Auto Injector • Stock the squad’s ambulances with the Epinephrine Auto Injector and a sharps disposal container The First Aid Squad • Send new EMT-B certified members to the regional Initial MONOC training programs • Epinephrine Auto Injector administered by EMT-Bs certified as per OEMS Policy only • Proper disposal and replacement of used or expired Epinephrine Auto Injectors • Send required reports to MONOC and OEMS upon using an Epinephrine Auto Injector NJ OEMS BLS Agency Application The EMT-B • Attend Initial and Renewal classes • Sign the MONOC contract to administer the Epinephrine Auto Injector • Maintain Current EMT-B and CPR certs • Adhere to all MONOC & OEMS Policies • Submit required reports to MONOC and OEMS on use Epinephrine Auto Injector NJ Epinephrine Auto Injector Law Immunity From Civil Liability An EMT-B certified to administer epinephrine auto injector pursuant to this law… or officers and members of any first aid, ambulance or rescue squad shall not be liable for any civil damages as the result of any act or the any omission of an act committed while in training to administer, or in the administration of, the epinephrine auto injector in good faith and in accordance with the provisions of this law Now let us take a look at Pathogenesis of Anaphylaxis Progression of Allergic Reaction Myths & Reality Anaphylaxis Fatalities Common Causes of Anaphylaxis Myth: Anaphylaxis Is Rare The Reality! • Anaphylaxis is underreported • Incidence seems to be increasing • Anaphylaxis leads to 200 deaths a year • Up to 41 million Americans at risk • 63,000 new cases per year • 5% of adults have history of anaphylaxis DEFINITION WHAT IS • Anaphylaxis ? Systemic allergic reaction Affects body as a whole Multiple organ systems may be involved • Onset generally acute • Manifestations vary from mild to fatal Myth: Anaphylaxis is Easy to Avoid If You Know What You are Allergic To REALITY: Most cases of Anaphylaxis are Accidental Exposures Immediate Treatment = Saved Lives Pathogenesis of Anaphylaxis • Hypersensitivity • Sensitization Stage • End result is an anaphylactic response – The clock is ticking Immediate Treatment = Saved Lives Pathogenesis of Anaphylaxis Antigen (allergen) exposure • Antigen Antigen: A substance that is capable of causing the production of an antibody • Antigens may or may not lead to an allergic reaction • Allergens: Antigens that cause an allergic reaction and the production of a substance called IgE Pathogenesis of Anaphylaxis Antigen (allergen) exposure Antigen Allergic Reactions Don’t Occur at First Exposure to Allergen • First Exposure • Immune system sees substance as allergic trigger or ALLERGEN and attempts to protect the body from that specific allergen by creating specific chemicals called ANTIBODIES Later Exposure with that same Allergen On subsequent exposures to same allergen, the antibodies attack & engage the invading allergens to produce the allergic response Pathogenesis of Anaphylaxis Plasma cells produce IgE antibodies against the allergen Plasma Cell • Immunoglobulin: A protein produced by plasma cells • IgE: A class of immunoglobulins (Ig) that includes the antibodies elicited by an allergic substance (allergen) • A person who has an allergy usually has elevated blood levels of IgE antibodies that will attack and engage the invading army of allergens Pathogenesis of Anaphylaxis IgE antibodies attach to mast cells and basophils Mast cell with fixed IgE antibodies Granules that contain histamine • Mast cell: A connective tissue cell whose normal function is unknown but which is frequently injured in allergic reactions, releasing chemicals including histamine that are very irritating and cause itching, swelling, and fluid leakage from cells • Basophil: A type of white blood cell with coarse bluish-black granules of uniform size within the cytoplasm. Basophils are so named because their cytoplasmic granules stain with basic dyes. Basophils contain and can release histamine Pathogenesis of Anaphylaxis IgE antibodies attach to mast cells and basophils Mast cell with fixed IgE antibodies Granules that contain histamine • Basophils contain and can release histamine • Histamine: A substance that plays a major role in many allergic reactions. Histamine dilates blood vessels and makes the vessel walls abnormally permeable. This will result in systemic swelling. HISTAMINES • Symptoms progress FAST! • These actions cause fluid loss – Swelling – Hypotension VASODILATION ↑ PERMEABILITY Anaphylactic Reaction • A Systemic allergic reaction - Affects body as a whole IMMEDIATE TREATMENT = SAVED LIVES Antigen More of same allergen invades body Allergen combines with IgE attached to mast cells and basophils, which will trigger degranulation and release of histamine and other chemical mediators . • • • • •• • • • • • • • • •• • • • • • • • • • • • • • • • • •• • • • • • • •• • • • •••• • • • • • •• • • • • • •• • • • • •• • • • •• • •• • • •• • •• • • • • • • •• • • • • • •• • • •• • • • • • • • • •• • • •• • • •• • • • •• •• • • • • • • •• •• •• • • • • • • • •• •• • • • • • •• • • • • • • • • • • • •• • • • •• • • • • • • ••• • • • • • •• • • • • • • • • • •• •• • • •• • • • • • • • •• • • • • •• • • • • • •• • • • • • • • • • • • • • • • •• • •• •• • • • • •• •• •• •• • • • • • • • • • • •• • • • • • • • • Mast cell granules releases contents after the antigen binds with IgE antibodies Histamine and other mediators Anaphylaxis Fatalities • Estimated 200 deaths annually • Symptoms progress FAST! • Risk factors: – Rapid IV allergen – Failure to administer epinephrine immediately Immediate Treatment = Saved Lives Common Causes of Anaphylaxis Common Causes of Anaphylaxis • Foods • Insect venoms • Latex • Medications • Immunotherapy – Insect venom – Inhalant allergens Now let us take a look at Clinical Presentation Anaphylaxis Signs & Symptoms of Anaphylaxis Myths & Reality Food - Venom – Latex Other Conditions Mimic Anaphylaxis Clinical Presentation of Anaphylaxis Immediate Treatment = Saved Lives Severe Allergic Reaction HIVES are also known medically as URTICARIA Immediate Treatment = Saved Lives Myth: Anaphylaxis Always Presents with Hives REALITY: • Approximately 10%-20% of all anaphylaxis cases will not present with any hives or other cutaneous manifestations • 80% of food-induced, fatal anaphylaxis cases were not associated with any cutaneous signs or symptoms Myth: The Cause of Anaphylaxis is Always Obvious REALITY: Idiopathic anaphylaxis is common • Triggers may be hidden – Foods – Latex • Patient may not recall details of exposure Clinical Presentation of Anaphylaxis • Cardiovascular System: – Tachycardia or Bradycardia – Hypotension – Arrhythmias – Chest Pain (Only 6% of the time) Immediate Treatment = Saved Lives Clinical Presentation of Anaphylaxis • Respiratory System: – Shortness of Breath – Throat Tightness – Tongue Swelling – Wheezing or Stridor Immediate Treatment = Saved Lives Clinical Presentation of Anaphylaxis Signs & Symptoms Incidence (%) Urticaria and swelling Upper airway edema Dyspnea and wheezing Flushed skin Dizziness, syncope, and hypotension Gastrointestinal symptoms Rhinitis Headache Substernal chest pain Itch without rash Seizure 88 56 47 46 33 30 16 15 6 4.5 1.5 Clinical Presentation of Anaphylaxis Hives 88% of the time Swelling of the Tongue 56% of the time These Sx RARELY present with any other conditions Conditions That Can Mimic Anaphylaxis • • • • • • Foreign Body Airway Obstruction Wheezing or Stridor from Other Etiology Other Respiratory Impairments Acute MI CHF Asthma Conditions That Can Mimic Anaphylaxis Foreign Body Airway Obstruction ANAPHYLAXIS FBAO Hives >88 % of the time NO HIVES Tongue Swollen >50 % of the time NOT PRESENT Prior Episodes May Have Had Hx Usually NONE Progression Symptoms progress increased SOB Reflexes relax & often lead to reduced Sx WITHOUT ANY INTERVENTION Breath Sounds 47% Bilateral Wheeze 65% Unilateral ↓ BS History - Events Leading Up to Episode? Conditions That Can Mimic Anaphylaxis Wheezing or Stridor Other Etiology ANAPHYLAXIS Wheeze - Stridor Hives >88 % of the time NO HIVES Tongue Swollen >50 % of the time NOT PRESENT Prior Episodes May Have Had Hx What is prior Hx? Progression Symptoms progress increased SOB Inhaler or Humidity often will reduce Sx Breath Sounds >47 % will wheeze History - Events Leading Up to Episode? Conditions That Can Mimic Anaphylaxis Other Respiratory Impairments ANAPHYLAXIS Other Resp Prob Hives >88 % of the time NO HIVES Tongue Swollen >50 % of the time NOT PRESENT Prior Episodes May Have Had Hx What is prior Hx? Progression Symptoms progress increased SOB OXYGEN often will reduce Sx Breath Sounds >47 % will wheeze Rales or Rhonchi? Look at the patient’s Meds & Prior History Conditions That Can Mimic Anaphylaxis Acute MI ANAPHYLAXIS Other Resp Prob Hives >88 % of the time NO HIVES Tongue Swollen >50 % of the time NOT PRESENT Substernal Chest Pain Only 6% of the time >70 % of the time Pain Radiates NO OFTEN Arrythmias RARE OFTEN Look at the patient’s Meds & Prior History Conditions That Can Mimic Anaphylaxis Acute MI Chest Pain in >70% of MIs – Only 6% of Anaphylaxis Conditions That Can Mimic Anaphylaxis CHF ANAPHYLAXIS Other Resp Prob Hives >88 % of the time NO HIVES Tongue Swollen >50 % of the time NOT PRESENT Breath Sounds >47 % will wheeze Rales (Wheeze early) Blood Pressure 33 % with ↓ BP Very High (Drops late) Pedal edema - + JVD – Frothy Pink Sputum NO OFTEN History – Orthopnia – Sleeping Position (# of Pillows?) Conditions That Can Mimic Anaphylaxis CHF CHF Occurs Primarily in the Geriatric Population Conditions That Can Mimic Anaphylaxis ASTHMA ANAPHYLAXIS ASTHMA Hives >88 % of the time NO HIVES Tongue Swollen >50 % of the time NOT PRESENT Breath Sounds 50% will not wheeze Wheeze (Absent Late) Progression Only Epi Reduces Sx ! Inhaler or Humidity often will reduce Sx Area Effected Upper Airway Lower Airway Many Patients will also have History of Both Anaphylaxis and Asthma ASTHMA This drawing shows a By contrast, this drawing shows tightened airway and inflamed normal, relaxed airway air sacs in the lungs and air sacs in the lungs Myth: Prior Episodes Predict Future Reactions REALITY: • No predictable pattern • Severity depends on: –Sensitivity of the individual –Dose of the allergen Anaphylaxis: Food Induced • Food allergies are usually due to the protein component of the offending food • For some reason some of the food protein is absorbed from the intestine intact, instead of being digested as most proteins are • Once the intact protein is in the blood stream, it is recognized as a foreign protein to the body, or in other words as an ANTIGEN Anaphylaxis: Food Induced • 35%–55% of anaphylaxis is caused by food allergy • 6%–8% of children have food allergy • 1%–2% of adults have food allergy • Incidence is increasing • Accidental exposures are common and unpredictable Immediate Treatment = Saved Lives Food Induced Anaphylaxis: Common Triggers Food-induced Anaphylaxis: Common Symptoms • Oropharynx: Swelling of lips and tongue, throat tightening, slurred speech • GI: Cramps, diarrhea, nausea, vomiting • Cutaneous: Urticaria, angioedema • Respiratory: Shortness of breath, cough, wheezing or stridor Anaphylaxis: Venom-induced Common Culprits (Triggers) 13 million Americans are sensitive to insect venoms Culprit – Bees – Wasps – Hornets – Yellow jackets Geographical Culprit – Fire ants – Marine life – Spiders – Honeybees and yellow jackets most common in East, Midwest, and West regions of US – Wasps, fire ants common in Southwest & Gulf Coast Venom-induced Reactions: Common Symptoms • Normal: Local pain, Redness, Mild swelling • Large local: Extended swelling, Redness • Anaphylaxis: Usual onset within 15–20 minutes – Cutaneous: Urticaria, Flushing, Edema – Respiratory: Dyspnea, Wheeze or Stridor – Cardiovascular: Dizziness, Loss of Consciousness, Tachycardia or Bradycardia (late), Hypotension, 30%–60% of patients have a systemic reaction with multiple stings Anaphylaxis: Latex Latex Gloves • 1%–6% of Americans (> 16 million) affected • 8%–17% incidence with health care workers • Repeated exposure leads to a higher risk • Incidence has increased since mid 1980s • Proteins in natural rubber latex • Component of ~40,000 commonly used items Anaphylaxis: Latex Latex Gloves • The sudden, large-scale increase in latex glove use by healthcare workers since the 1980s lies at the heart of the growing problem of latex allergy • As health care workers protect themselves from AIDS and other bloodborne diseases, latex glove use became virtually universal in hospitals • Healthcare workers, were exposed to more latex than ever - many have become sensitized to it Anaphylaxis: Latex Latex Gloves • Irritant contact dermatitis – Dry, itchy, irritated hands • Allergic contact dermatitis – Delayed hypersensitivity • Latex allergy – Immediate hypersensitivity – Sx: hives, itching, sneezing, rhinitis, cough, wheezing or stridor, shortness of breath – Greatest risk with mucosal contact Latex Anaphylaxis: Prevention AVOIDANCE • Use latex-free products • Alert employer/health care providers, schools about • • need for latex-free products and equipment Wear MedicAlert bracelet Awareness of cross-sensitivity with foods: – Banana – Avocado – Chestnuts – Kiwi – Stone fruit – Others Other Causes of Anaphylactic Reactions • Antibiotics • Chemotherapeutic agents • Aspirin • Biologicals (vaccines) • Radiocontrast media (IV Dye) Now let us take a look at The Treatment of Anaphylaxis Epinephrine Epinephrine Auto Injector Maintaining the Auto Injector EPI Auto Injector Administration Treatment of Anaphylaxis Immediate Treatment with Epinephrine Imperative – No contraindications in Anaphylaxis – Failure or delay = Fatalities – Must be available at all times Immediate Treatment = Saved Lives Epinephrine Auto Injector A Lifesaving Tool Now In the Hands of the EMT-B Immediate Treatment = Saved Lives What Is Epinephrine ? EPINEPHRINE = ADRENALINE • Adrenaline is a natural hormone released in response to stress • It is a natural "antidote" to the chemicals released with severe allergic reactions triggered by a drug, food, or insect allergy • It is destroyed by enzymes in the stomach, so must be injected • When injected, it rapidly reverses the effects of a severe allergic reaction CLINICAL PHARMACOLOGY EPINEPHRINE = ADRENALINE • Strong vasoconstrictor action – Acts quickly to counteract both vasodilation and increased vascular permeability which can lead to loss of volume and hypotension Anaphylaxis • Epinephrine causes smooth muscle relaxation of the bronchial walls in the airway – ↑ air flow alleviates wheezing & dyspnea • Epinephrine is a sympathomimetic drug – Heart beats stronger and faster = more effective Side Effects ? EPINEPHRINE = ADRENALINE • Side effects of epinephrine may include palpitations, tachycardia, apprehension, sweating, nausea and vomiting, pallor, respiratory difficulty, tremor, headache, dizziness, weakness, and nervousness • Cardiac arrhythmias may occur after the administration of epinephrine Myth: Epinephrine is Dangerous The Reality! • Risks of anaphylaxis far outweigh risks of epinephrine administration • Minimal cardiovascular effects in children (Simons et al, 1998) • Use caution when administering epinephrine in elderly patients or those with known cardiac disease THE AUTO INJECTOR Preloaded Unit Dose Spring Loaded Trigger AUTO INJECTORS ONLY THE EMT-B IS NOT PERMITTED TO USE A SYRINGE X TWINJECT CANNOT BE USED BY THE EMT-B X AUTO INJECTORS ONLY CANNOT BE USED BYTHE EMT-B IS NOT THE EMT-B PERMITTED TO USE A SYRINGE The First Dose is an AUTO INJECTOR Second Dose is a SYRINGE The EpiPen® Dismantled EpiPen® The Spring The Needle The Syringe How Does It Work ? Expiration Dates MONITOR THE EXPIRATION DATES Check the expiration date when you get the prescription - You should be able to obtain an expiration date 12 - 14 months out Return expired Auto Injectors to Pharmacy Expiration Date and Lot Number Expiration Dates Join the Free EpiPen®Center for Anaphylactic Support™! www.epipen.com/epipen_reminder Expiration Dates EpiPen®Center for Anaphylactic Support™ • There is a free expiration reminder program • Register every time you purchase EpiPen® • You get reminders before the expiration date Expiration Date and Lot Number Storage of EpiPen® X • Clear Window CHECK FOR CLARITY X Improper storage of the Auto Injector can cause the Epinephrine to oxidize & go bad • Check the Epinephrine periodically through the viewing window - be sure the solution is clear and colorless • Replace Auto Injector immediately if solution is found to be clouded Storage of EpiPen® X • Clear Window CHECK FOR CLARITY X Epi stable at room temp until expiration date • Epinephrine should not be refrigerated refrigeration may cause unit to malfunction • Epi should not be exposed to high heat • Do not expose the EpiPen® to direct sunlight for prolonged periods of time How is Epinepherine Given? Intramuscular (IM) Injection • A shot where the needle goes into the muscle • to deliver a certain amount of medicine The drug is absorbed in the muscle and the bloodstream then carries it through the body • IM injections are made into the striated muscle fibers under the subcutaneous layer of the skin Where Do I Give Epinepherine? VASTUS LATERALIS MUSCLE • Forms part of quadriceps muscle group • Located on anteriolateral aspect of thigh • Used as the site for IM injections as it is generally thick and well formed in patients of all ages and is not located close to any major arteries or nerves • This site is readily accessed • Middle third of muscle is the injection site QUADRICEPS Where is Epinepherine Given? ANTERIOLATERAL MID THIGH AREA • Same site is used for both Adult and Pediatric • The EpiPen should simply be pushed against the fleshy outer (lateral) portion of the thigh • There is no need for more precise placement • Do not attempt an injection into a vein or the buttocks .3 mg .15 mg OEMS Policy Use the EpiPen® Jr For Patients Under 4 Years Old EpiPen® .3 mg .15 mg EpiPen® • Epinephrine dosing is based on body weight • The EpiPen® Auto Injector (0.3 mg) is for individuals weighing 66 lbs. or more • The EpiPen® Jr Auto Injector (0.15 mg) is for those individuals weighing between 33 and 66 lbs • The OEMS Epinephrine Auto Injector Policy states to use a EpiPen® Jr Auto Injector (0.15 mg) for patients Under 4 years of age Determining Weight & Age Don’t Forget the Obvious ASK THE PARENT ! PEDI - WHEEL BROSELOW SYSTEM Now let us take a look at Using the Epinephrine Auto Injector The Patient Assessment Using the Auto Injector Common Errors Post Use Epinephrine Auto Injector How Do I Use It ? AUTO INJECTORS ONLY X THE EMT-B IS NOT PERMITTED TO USE A SYRINGE Epinephrine Auto Injector EMT CHECKLIST My BLS Agency is registered with and has been approved by OEMS I have completed the mandated training program for Epinephrine Auto Injectors I am a current NJ EMT-B I have a current CPR card The patient does not have his own ALS has not yet arrived on location Remember Safety First Look Around! Be Alert! The Scene Size-Up STOP LOOK • Remember crew safety and BSI! • You already have Off Line Medical Control • Check environment for source of the reaction—insects, foods, medications • Call ALS immediately • How many patients? • Do you need additional resources? Initial Assessment • As you approach develop a General Impression • Assess mental status • Assess Airway • Assess the adequacy of Breathing • Assess Circulation • Identify patient priority Initial Assessment Identify the patient priority • If unresponsive, then immediately evaluate and treat life threats • ABCs • Provide 100% oxygen Provide 100% OXYGEN Provide 100% oxygen via NRB, but be ready to assist ventilations if necessary with a BVM High Con O2 BVM for Ventilations • Nonrebreather mask • For inadequate tidal @ 10-15 liters per min 10-15 lpm volume or resp rate Set @ 15 lpm General Impression & Chief Complaint Consider the need for an Epinephrine Auto Injector if any of the following are present: – – – – – – Generalized urticaria (Present >80% of the time) Swelling of the face, tongue, or lips Chief Complaint of respiratory distress or arrest A tightness in the chest and or throat Wheezing or Stridor Altered mental status • Restlessness, Anxiety, Confusion • Seizure, Unresponsiveness Initial Assessment • Look for indications of any circulatory distress • Indications of Hypoperfusion – Rapid heart rate – Cool, moist skin – Delayed capillary refill times • If unable to palpate a pulse, then begin CPR and AED resuscitation immediately Focused History and Physical Exam • Obtain Baseline Vital Signs • Look for Medical Alert Tags • Check environment for source of the ALLERGY reaction—insects, foods, medications • Where is the ALS Unit ?? • Responsive patients - SAMPLE HISTORY • Unresponsive patients need to receive a Rapid Physical Exam Immediate Treatment = Saved Lives SHOCK ?? Consider an Epinephrine Auto Injector if any signs or symptoms of shock are present: CHILD 1 TO 12 years old Heart Rate > 140 AND/OR BP < 70 Systolic ADULT OLDER THAN 12 Heart Rate > 120 AND/OR BP < 80 Systolic INFANT UNDER 12 months Heart Rate > 180 AND/OR BP < 60 Systolic Fast pulses and hypotension are ominous signs SAMPLE •S — Signs and Symptoms What signs & symptoms occurred at onset? • A — Allergies Is patient allergic to meds, foods, or other? • M — Medications What medications is the patient taking? • P — Pertinent Past History Does the patient have any medical history? • L — Last Oral Intake When & What did patient last eat or drink? • E — Events Leading Up To What events led to this incident? ASK LISTEN STAY GO Transport Decision TRANSPORT Transport Promptly • Take patient medications and the Epinephrine Auto Injector with you • Treat respiratory distress and shock, then transport immediately Auscultate Breath Sounds WHEEZING STRIDOR RALES (CRACKLES) RHONCHI LISTEN Focused History and Detailed Physical Exam • Consider if: – Complaint or history is confusing – There is extended transport time – You need to clarify findings • In severe Anaphylaxis reactions the Focused & Detailed Physical exams may be omitted Immediate Treatment = Saved Lives HIS MINE Do I Use the Patient’s or Mine ? WHAT IF THE PATIENT HAS HIS OWN EpiPen® ? If the patient has a prescribed Epinephrine Auto Injector then ASSIST the patient with theirs EpiPen/EpiPen Jr: Directions for Use Remove the Auto Injector from the Storage Tube Check the Expiration Date & Color of the Epi Storage Tube EpiPen/EpiPen Jr: Directions for Use Remove the Safety Cap The device is now LOADED X AFTER THE SAFETY CAP IS REMOVED KEEP YOUR FINGERS AWAY FROM THE END EpiPen/EpiPen Jr: Directions for Use Insert in the Lateral Mid Thigh • Place auto injector firmly against lateral portion of the thigh, midway between the waist and the knee • Firm pressure activates spring mechanism in the auto injector and forces the needle into the thigh muscles EpiPen/EpiPen Jr: Directions for Use Hold For 10 Seconds and Remove • • • Hold in place for 10-15 seconds while the epi is injected in muscle Remove auto injector from the thigh - careful the needle will now be projecting Massage the injection site – this will enhance absorption of the epi COMMON ERRORS MISTAKE NUMBER 1 • The black tip contains • the needle and needs to be placed against the mid-thigh. Holding the wrong end and injecting the thumb (blue line) is painful and not very effective ... COMMON ERRORS MISTAKE NUMBER 2 • Unless the safety cap is removed (blue line), the EpiPen will NOT work, no matter how hard you push ... COMMON ERRORS MISTAKE NUMBER 3 • This photograph is more subtle. The patient is pressing the white end very hard (blue line), assuming there is a "button" at the white end. There is not! EpiPen/EpiPen Jr: Directions for Use Needle is Exposed – BE CAREFUL ! • • Clear Window Place the used Auto Injector in a sharps container for Safety Note: Most of the liquid (about 90%) stays in the auto-injector and cannot be reused - The correct epinephrine dose was given if the RED FLAG appears in clear window TRANSPORT The Ongoing Assessment • You should have already initiated your patient TRANSPORT to the hospital – DO NOT DELAY • Take the Epinephrine Auto Injector with you • Where is ALS ? Consider meeting the ALS unit Line of Sight en route to the hospital • Notify Receiving Hospital (If NO ALS) Immediate Treatment = Saved Lives TRANSPORT The Ongoing Assessment • Monitor with Vigilance Level of Distress, Level of Consciousness, Blood Pressure, Respirations, Pulse, Breath Sounds • Repeat a second Epinephrine dose if the signs and symptoms still persist after 10-15 minutes • Maintain Normal Body Temp • Where is the ALS unit? Immediate Treatment = Saved Lives TRANSPORT Biphasic Reactions • Biphasic reactions - Sx occur again after the initial • • • anaphylaxis Sx have completely resolved Biphasic reactions can occur several hours after the initial Anaphylactic episode Biphasic reactions happen in up to 20% of cases Biphasic reactions are treacherous – more difficult to treat than initial episode – Patients often require intubation Immediate Treatment = Saved Lives DOCUMENTATION REQUIRED ON PCR • Location of the Injection Site • Medication Name and Dose • Time Epi was Administered • Vital Signs Pre and Post Epi • Any changes in the patient’s condition Immediate Treatment = Saved Lives DOCUMENTATION REQUIRED FINISH THE PAPERWORK! • Leave a copy of the Patient Care Report (PCR) at the hospital • Complete the MONOC QA Form • Send a copy of the PCR to – MONOC within 7 days after the call – OEMS within 45 days after the call Immediate Treatment = Saved Lives Medical Director DR. MICHAEL MARCHETTI • You administered the Auto Injector under his Off-line Medical Control • Responsible for all clinical aspects of the MONOC EpiPen Program • Will review documentation provided for Quality Assurance purposes Now let us take a look at AHA 2010 Guidelines for CPR and Emergency Cardiac Care Assessing Ventilations C-A-B Sequence Quality CPR Interfacing With ALS Check Responsiveness • Tap the patient’s shoulder – ask “are you all right?” • Check for movement / chest rise and fall . • Check for breathing / adequate breathing. AGONAL Breathing Assess For Effective Breathing Occasional gasps = agonal breathing Will soon lead to cardiac arrest Called “Guppie Breathing” This is NOT effective breathing Pulse Check • Check the carotid artery for at least 5 seconds and no longer than 10 seconds to determine presence of a pulse. • If no pulse, perform 5 cycles of compressions and breaths (ratio 30:2) beginning with chest compressions. Chest Compressions Compress HARD & FAST • Compress at a rate of at least 100/min. • Ratio of compressions to breaths same for 1 rescuer or 2 rescuers – 30:2 • Each set of 30 compressions should take 18 seconds or less. Ventilations This is much too FAST Avoid the Urge To Ventilate TOO FAST or TOO HARD! • Ventilations delivered TOO FAST or with TOO MUCH VOLUME are NOT beneficial and may even be HARMFUL • Deliver just enough volume to make the chest rise • Each breath should be delivered over one second Each time you ventilate intrathoracic pressure increases and the flow of blood through the heart and the blood vessels in chest decreases Rate of Ventilations This is much too FAST Adult patient in respiratory arrest with a pulse: – Deliver about 10 - 12 breaths per minute – Give just enough volume to allow the chest to rise – Resist the urge to ventilate faster or harder! Child or Infant in respiratory arrest with a pulse: – Deliver 12 - 20 effective breaths per minute – Resist the urge to ventilate faster or harder! Each rescue breath should be delivered over one second A Word About Advanced Airways 211 MICU When ALS arrives on scene the paramedics will secure the airway with an Endotracheal Tube Once the ET is in place ventilate at: 8 times per minute Once every 7 seconds • DO NOT PAUSE your cardiac compressions to give breaths • This will optimize blood flow Delivery of Ventilations AGE GROUP Breaths Per Min ADULT 10 per min CHILD 15 per min INFANT 20 per min ADULT with ET 8 per min Each rescue breath should be delivered over one second AIRWAY EQUIPMENT Provide 100% oxygen via NRB, but be ready to assist ventilations if necessary with a BVM High Con O2 BVM for Ventilations • Nonrebreather mask • For inadequate tidal @ 10-15 liters per min 10-15 lpm volume or resp rate Set @ 15 lpm Best Use of the BVM 2 Rescuer Bag Valve Mask Technique is Preferred • Minimizes the chance of the 2 • Note the PADDING Note the E – C Clamp • most common BVM errors - Poor Seal – Loss of Volume - Squeezing bag inadequately One rescuer seals the mask and opens the airway with an E – C clamp The second rescuer squeezes the BVM with both hands - for good tidal volume (chest rise) Best Use of the BVM 2 Rescuer Bag Valve Mask Technique is Preferred • Sellick Maneuver is done by a • Note the PADDING Note the E – C Clamp • third rescuer with ventilations of an unprotected airway BLS can provide the Sellick Maneuver early & continually until a ET tube is inserted by the Paramedics Note the padding under the head for this adult patient – What if this were a child or infant? The Sellick Maneuver The routine use of the Sellick Maneuver is no longer recommended for use American Heart Association The Sellick Maneuver BLS Providers can help with the Sellick Maneuver • Used to help line up the airway structures in ET intubation – will help to visualize the vocal cords • Also will help to prevent gastric distension and vomiting as you ventilate an unprotected airway The Sellick Maneuver BLS Providers can help with the Sellick Maneuver • Performed by applying gentle pressure to the anterior neck at the Cricoid Cartilage • BLS can provide this maneuver early and continually until an ET tube is inserted PEDI AIRWAY EQUIPMENT All BLS Ambulances must have airway adjuncts of all types available for all age groups of patients Variety of Sizes •OPA •BVM BROSELOW SYSTEM SUCTION EQUIPMENT • BLS Ambulances must have SUCTION available for all patients – Suction should be set up READY FOR USE Suction Equip • READY TO USE • Rigid tip catheter • 15 seconds On Board Equip • Oxygen • Suction Coronary Perfusion Pressure (CPP) 2010 Guidelines Focus on Maintaining CPP • Maximizing delivery of quality compressions • Minimizing the delivery of ventilations and other “hands off time” HIGH QUALITY CPR SAVES LIVES The Need for Quality CPR PUSH HARD PUSH FAST • Maintain compression rate at - least • This Per Minute rate is same in all AHA age groups - for both one and multiple rescuers MAKE EVERY COMPRESSION COUNT! Every compression done improperly decreases CPP A Major Change All rescuers acting alone should deliver Compressions to Ventilations for all victims except newborns • Adequate blood flow is needed to provide delivery of oxygen to the vital organs • Scientific studies measured blood flow to the heart muscle in the coronary arteries – Coronary Perfusion Pressure (CPP) Coronary Perfusion Pressure and the CPR Cycle Scientific data shows that CPP builds up to the maximum with the first 5 - 10 compressions of the CPR cycle CPP will be maintained by well delivered uninterrupted cardiac compressions When cardiac compressions are interrupted CPP falls to almost zero immediately It will then take the next several compressions to build the CPP back up to the optimal level again MINIMIZE INTERRUPTIONS Coronary Perfusion Pressure Over a CPR Cycle Coronary Perfusion Pressure (CPP) Over CPR Cycle 30 Compressions to 2 Breaths Coronary Perfusion Pressure (CPP) Over CPR Cycle 30 Compressions to 2 Breaths A Cycle of 30 Cardiac Compessions Delivered at a rate of 100 per minute PUSH HARD - PUSH FAST 1 10 20 A Cycle of 30 Cardiac Compessions Delivered at a rate of 100 per minute PUSH HARD - PUSH FAST 30 PUSH HARD 2 Breaths CPP = 0 2 Breaths CPP = 0 Maximum CPP Maintained 2 Breaths CPP = 0 2 Breaths CPP = 0 Maximum CPP Maintained 1 Per Minute 10 20 30 PUSH FAST Compressions to Ventilations One Lone Rescuer Multiple Rescuers ADULT 30 : 2 30 : 2 CHILD 30 : 2 15 : 2 INFANT 30 : 2 15 : 2 MINIMIZE INTERRUPTIONS Hand Position AGE GROUP Place Your Hands ADULT Center of chest between nipples 2 hands - Heel of hand on chest – other on top CHILD Center of chest between nipples 1 hand - Heel of one hand on chest INFANT One Rescuer INFANT Multiple Rescuers Just below nipple line 1 Rescuer – 2 Fingers Just below nipple line 2 Rescuers – 2 Thumbs NO LANDMARKING “Eyeball” the correct spot and place your hands Minimize Hands Off Time Two Thumb Compression Technique For Multiple Rescuer Infant CPR • Encircle the infant’s chest with both hands • Spread your 4 fingers across the thorax and place your 2 thumbs together on the lower half of the sternum Note the PADDING Two Thumb Compression Technique For Multiple Rescuer Infant CPR • Squeeze the thorax with your 4 fingers as you compress over sternum with your 2 thumbs • Second rescuer provides ventilations (15:2 Ratio) • This technique has been proven to achieve higher CPP in studies Note the PADDING SUMMARY NJ Epinephrine Auto Injector Policy – Allows NJ EMT-B to carry the Epinephrine Auto Injector in the ambulance & administer under off-line medical control Anaphylaxis – Anaphylaxis is a condition that progresses through several phases very rapidly – Anaphylaxis can be triggered by several things – Food, Stings, Latex most common – Other conditions can mimic Anaphylaxis SUMMARY The EpiPen – The EpiPen is a safe easy device that can rapidly reverse the effects of Anaphylaxis – EMT-B should understand the actions, the side effects, dose, and site to use for EpiPen Using the Epi-Pen – The EMT-B needs to perform an accurate rapid patient assessment – Proper documentation required per policy – Transport should not be delayed SUMMARY Airway and CPR Skills – It is essential the EMT-B delivers proper ventilations and compressions to all ages – The EMT-B must be proficient in AHA 2010 – Quality CPR is an essential skill Conclusion – The Epinephrine Auto Injector is a new lifesaving tool now in the hands of the EMT – IMMEDIATE TREATMENT = SAVED LIVES Additional Information For Anaphylaxis -- WEB SITES FOR INFORMATION -- EpiPen Auto Injector A Lifesaving Tool Now In the Hands of the EMT-B Immediate Treatment = Saved Lives Thank You For Your Participation For More CEUs www.MONOC.ORG