Neuro_Anatomy_2012
advertisement

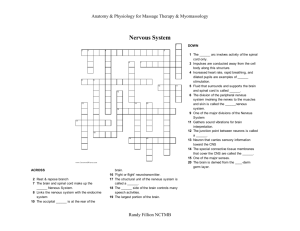
Neurosurgery Outline • • • • • • • • A&P Pathology Diagnostics/Pre-operative Testing Medications/Anesthesia Positioning/Prepping/Draping Supplies/Instrumentation/Equipment Dressings/Drains/Post-op Care Procedures: Carpal Tunnel Release, Craniotomy, Cervical Discectomy, Lumbar Discectomy, Ventroperitoneal Shunt Nervous System • • • • Functions: Senses changes in environment Interprets changes Stimulates movement to respond to these changes Organization of the Nervous System • Two systems: 1. CNS Central Nervous System • Two major parts: Brain and Spinal Cord 2. PNS Peripheral Nervous System • Everything else Peripheral Nervous System • Two major parts: • Afferent Nervous System • Sensory neurons take info from PNS to CNS • Efferent Nervous System • Motor neurons take info from CNS to PNS Efferent Nervous System • • 1. • • 2. • • • • • Motor nervous system 2 parts: Somatic Nervous System Skeletal muscle control Conscious control Autonomic Nervous System Cardiac muscle, smooth muscle, and glands Unconscious control Has 2 divisions: Sympathetic Division Parasympathetic Division Autonomic Nervous System • Sympathetic vs. Parasympathetic • Controlled by hypothalamus and medulla oblongata • Both are different nerves going to the same effector or target • Are antagonistic • Parasympathetic = decreased skeletal blood flow, increased organ blood flow (quietly eating) • Sympathetic = increased skeletal blood flow, decreased organ blood flow (eatus interruptus by a bear!) Also called fight or flight; prepares body for emergencies Spinal Cord • Functions: • Info to and from the brain • Integration of reflexes • Location: • Begins at foramen magnum and extends to 2nd lumbar • About 16-18” in length Spinal Cord Support Structures • • • • • • • Vertebra 33 total 7 cervical 12 thoracic 5 lumbar Sacrum formed by 5 fused bones Coccyx formed by 4 fused bones Intervertebral Disks • Separate vertebrae • Outer layer is tough and called the annulus fibrosis • Inner core is soft and called the nucleus pulposus • Bear stress incurred with body weight and when lifting Spinal Cord Support Structures • • • 1. • 2. • 3. • Meninges Between vertebra & spinal cord Epidural space between vertebra and dura mater Dura Mater outermost layer extends to S-2 Subdural space between dura mater and arachnoid Arachnoid extends to S-2 Subarachnoid space contains CSF Pia Mater adheres directly to spinal cord and extends to L-2 Meninges also cover brain/continuous layer/difference epidural space not present Spinal Nerves • 31 pair • Names and numbers depend on where enter and exit • Each has a ventral and dorsal root • Ventral root = motor • Dorsal root = sensory • 8 cervical • 12 thoracic • 5 lumbar • 5 sacral • 1 coccygeal Brain • Protected by the cranium or skull Brain • • • • • 4 major parts: Brain stem Diencephalon Cerebellum Cerebrum Weight about 3 lbs. Support Structures of the Brain 1. Meninges • Continuous layer with spinal cord • NO epidural space Support Structures of the Brain 2. Cerebrospinal fluid (CSF) • About 800ml produced each day by the choroid plexus, a specialized set of capillaries • Circulates inside subarachnoid space through central canal of spinal cord and the ventricles of the brain • Reabsorbed in arachnoid villus found in the parietal lobe • Functions as a shock absorber and circulates nutrients Support Structures of the Brain 3. Blood Brain Barrier • Specialized set of capillaries exclusive to the central nervous system • Less permeable than any other capillaries in the body • Advantage = keeps out unwanted chemicals • Disadvantage = difficult to diffuse materials out, hence difficulty in treating conditions such as encephalitis Brain Stem • • • • 3 parts: Medulla oblongata Pons Midbrain Medulla oblongata • Contains: • 5 of 12 cranial nerves • Pyramids: function only with motor neurons/a crossing of the spinal nerve impulses • Reflex centers: hiccupping, sneezing, coughing • Vital reflex centers: • Cardiac center – heart rate • Vasoconstrictor center-BP via blood vessel diameter control • Respiratory center - breathing Pons • Above medulla • Switching point for motor neurons • Respiratory center Midbrain or Mesencephalon • Above pons • Involuntary eye and head movement in response to auditory stimuli Diencephalon • 2 parts: • Thalmus • Hypothalmus Thalmus • Relay center for sensory information • Interprets stimuli for example pain from changes in temperature (hot stove) • 1st level of reasoning occurs here • Recognizes crude touch NOT localized touch Hypothalmus • Controls large number of subconscious functions • Controls most of Autonomic nervous system • Where endocrine and nervous systems interface • Homeostasis regulation of the body • Controls: body temp, thirst, hunger, sleep and waking habits, psychosomatic disorders, rage and aggression Cerebellum • • • • 2nd largest part of the brain Primarily a motor area Controls skeletal muscles, subconsciously Receives sensory input from eyes, muscles, joints, and inner ear • Posture, balance, coordination, equilibrium • Muscle sense tells body where other parts are Cerebrum • Largest part of brain • Motor/sensory/association area • 4 Lobes: frontal, parietal, occipital, temporal • Each controls a specific function be it motor or sensory • Limbic system: controls emotion/functions in cerebral cortex and diencephalon • See page 970 Figure 24-4 in Price Cerebrum Lobes’ Function • Frontal • Memory, abstract thinking, ethics, judgement, emotion, expressive speech, motor • Parietal • Sensory, receptive speech, written word • • • • • Temporal Auditory, olfactory Occipital Visual cortex Visual association Cranial Nerves • All originate in the brain stem EXCEPT the 1st and 2nd • Classified as sensory or mixed (sensory and motor) nerves • Directly off of brain • Do not go through the spine • Identified by Roman numerals and names Cranial Nerves I. II. III. IV. V. VI. Olfactory - sense of smell Optic – sense of sight/vision Occulomotor – eyeball, eyelid movement (medial, inferior, superior rectus, inferior oblique), pupil constriction, lens accommodation Muscle sense for eyeball Trochlear – eyeball movement (superior oblique) Muscle sense for eyeball Trigeminal – masseter muscle control Sensory part has 3 branches: ophthalmic (forehead to corner of eye), maxillary (corner of eye to upper lip/teeth), and mandibular (lower lip/teeth/tongue) All three convey sense of touch, pain and temp changes Abducens - same as IV eyeball movement (lateral rectus) and eyeball muscle sense FYI: EOM formula LR6(SO4)3 Cranial Nerves VII. Facial- facial muscles, lacrimal and salivary glands anterior 2/3 of tongue (taste) VIII. Vestibulocochlear -last of totally sensory nerves; has 2 branches: vestibular conveys balance and cochlear which conveys sense of hearing IX. Glossopharyngeal -salivary gland secretion and posterior 1/3 of tongue X. Vagus – internal organ control motor and sensory; originates in medulla and goes down through neck into chest and abdomen XI. Accessory – controls head and neck movement, speech, and muscle sense for the head XII. Hypoglossal – tongue muscles: swallowing, speech, muscle sense for tongue Neuro Pathology Cervical Spine Pathology • Very serious • Can have severe consequences related to all of the spinal cords’ nerve pathways • Spondylosis is osteophyte or bone spur formation in the spinal canal • Cervical disk extrusion acute or chronic • Treatment errs on the side of caution due to potential extreme consequences of surgical intervention Thoracic Pathology • Spondylosis • Extrusion of disk Lumbar Pathology • • • • Spondylosis Stenosis Spondylolithesis Disk extrusion Neoplasms/Tumors • Two types: • Primary • Originate in nervous tissue or meninges • Secondary • Are metastasized from other parts of the body • May be classified as benign or malignant Tumors • Benign tumors: • “Craniopharyngiomas, epidermoids, hemangiomas, menigiomas, acoustic neuromas, and pituitary microadenomas” • Malignant tumors: • “Astrocytes or gliomas” Price, 2004 Price, 2004 • Benign usually excisable via craniotomy • Malignant normally cannot be completely removed but efforts are made to remove most Head Trauma • Includes; • Scalp lacerations, fractures, hematomas (epidural or subdural), and brain injuries Spinal Cord Trauma • • • • Vertebral Fracture Vertebral Dislocation Herniated disk into spinal canal Laceration from GSW or MVA Cerebrovascular Disease • #3 cause of death in US • Symptoms reflect ischemia (TIAs) or hemorrhage • Intracranial aneurysm • Arteriovenous malformations • Brain hemorrhage • Stroke or cerebrovascular accident (CVA) Congenital Pathology • Craniosynotosis “premature closure of the cranial sutures” • Hydrocephalus result of obstructed CSF flow • Spina bifida Price, 2004 Infection • Abscess • Subdural empyema • Post-op infection Spinal Cord Tumors • Intramedullary in the spinal cord • Intradural in dura, outside spinal cord • Extradural outside spinal cord Price, 2004 Peripheral Nerve Pathology • Carpal tunnel syndrome - compression of the median nerve • Ulnar nerve compression – compression of ulnar nerve by the ligament of Osborne Price, 2004 Diagnosis • History and physical • Symptoms usually specific to area of pathology • Electroencephalogram (EEG) • X-ray • Myelogram • CAT Scan • MRI • Cerebral arteriograms Medications • Lidocaine 1% with epinephrine • Topical hemostatic agents: gelfoam, avitene, surgicel, bone wax • Antibiotic irrigants • Topical papaverine for prevention of spasm during intracranial artery surgery • Methyl methacrylate with cranioplasty • Heparin saline irrigation again with intracranial artery surgery • Contrast solutions with cerebral arteriography • Gliadel wafers (tumor bed of glioblastoma) Anesthesia • General • Could be local with MAC for minor laceration suturing Positioning • Cranial Surgery • Supine primarily, with a specialty headrest and or fixation devices • Can be lateral or semilateral • Sitting • Prone • Varies with location of access • Spinal surgery • Anterior procedures require supine • Posterior procedures require prone Preps • Will require shave especially on head • Varies with surgeon preference: betadine, alcohol, chlorohexidine • Care taken NOT to get in patient’s eyes or facial orifices Draping • Toweled out • Adhesive type drape • Specialty drapes: laparotomy, thyroid, craniotomy, lumbar • Stockinette for peripheral procedures Supplies • • • • • • • • • • • • • • Marking pen Disposable bi-polar cord Monopolar pencil/bovie Cottonoids/patties Raney clips Hemostatic clips Shunt catheters, tubing, connectors Cotton balls Hemovac drain Nerve stimulator Telfa Microscope drape C-Arm drape Ultrasound wand drape Instruments • Minor tray if laminectomy and craniotomy trays do not have basic instrumentation • Laminectomy tray • Craniotomy tray • Basic ortho tray • Plates and screws • Specialty self-retaining retractor trays: Greenburg Miscellaneous Instrumentation • See pages 987-990 in PRice Equipment • • • • • • • • • • • • • • microscope Video tower YAG or CO2 laser Positioning equipment: Mayfield headrest, Gardner-Wells Operative Ultrasound machine Stereotaxis system CUSA Cavitron ultrasonic aspirator Bipolar and monopolar ECU Nitrogen source for power equipment (saws/drills) Mayfield overbed table Headlight and light source C-Arm and monitor Cell saver Fluid warming and temperature regulating equipment Dressings/Drains/Postop Care • Dressings surgeon preference • Drains surgeon preference • Post-op care: keep field sterile until patient has left the OR • Careful with moving patient to avoid patient injury and hemorrhage Post-operative Complications • • • • • • Infection Hemorrhage Nerve damage CSF leakage Meningitis Neurological deficits