Chapter 9.1 – Overview of the Excretory System
advertisement

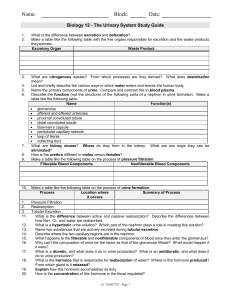
Chapter 9 – Excretion and the interactions of systems Pages 306 - 310 Structures of the Excretory System Structure 1. renal artery Function carries blood into the kidney from the aorta 2. renal vein carries blood away from the kidney into the inferior vena cava carries blood away from the heart toward the lower torso and legs carries blood from the lower torso and legs to the heart removes wastes from the blood, thus producing urine carries urine from a kidney to the urinary bladder temporarily stores urine 3. aorta 4. inferior vena cava 5. kidney 6. ureter 7. bladder 8. urethra carries urine from the urinary bladder to the exterior of the body The Problem of Waste in a Human Body A functioning system that produces waste uses different methods to release waste from the system, waste in the human body include excess water, chloride and sodium ions, carbon dioxide, etc. The excretory system is used to eliminate these waste from the fluids already in use, or are yet to be used, by cells to function. The main organ of the excretory for separating useful fluids and waste in the body is the kidney. The Function of a Nephron in the Kidney • The function of Nephrons in the kidney can be compared to the function of the pulmonary valve in the human heart • Nephrons are millions of microscopic structures that filter away waste from the blood and transforming it into urine • The Nephrons are organized into 3 main regions, a filter, a tube and a duct which can be viewed in the image below Pages 311 - 315 Urine Formation Four processes used for urine to be created: Glomerular filtration - moves filtrate (water and solutes) from blood into nephron. Tubular reabsorption – removes useful solutes from filtrate back into blood for reuse by body systems. Tubular secretion – moves additional wastes and substances from blood into filtrate. Water reabsorption – returns water from the filtrate back to blood for reuse. Glomerular Filtration Start of urine formation, glomerular filtration: Water and dissolved substances are forced from the blood in the glomerulus into the Bowman’s capsule Capillaries of the glomerulus are very porous and allow water and dissolved solutes to easily pass through Pores are small enough that blood cells and proteins cannot cross High pressure in the glomerulus (4x higher than elsewhere), aides filtration Tubular Reabsorption Tubular reabsorption – the recovery process Occurs in the loop of Henle 65% of filtrate is reabsorbed to the body Reabsorption occurs via active and passive transport Nutrients like sodium, glucose and other solutes are actively transported back into blood from filtrate. Negatively charged ions are passively absorbed by electrical attraction Water is absorbed by osmosis Tubular Secretion Occurs in distal tubule and collecting duct Excess hydrogen ions (H+) are secreted into the distal tubule to maintain the pH of the blood Other substances not normally in the blood, such as medication, are secreted into the distal tubule filtrate Reabsorption and secretion in the distal tubule are under the control of hormones Water Reabsorption Water reabsorption occurs in the collecting duct Filtrate still contains a lot of water The reabsorption of water in the collecting duct causes the filtrate to become 4x as concentrated by the time it exits the duct. The end product is approx. 1% of the volume of the original filtrate and is now called urine Summary Part of the Nephron Function Glomerulus and bowman’s capsule Filtration - blood pressure forces water and dissolved substances from the blood plasma through the pores of the glomerular wall. Bowman’s capsule receives filtrate. Reabsorption – passive and active reabsorption of water and ions from the filtrate back to blood Secretion – foreign components of blood are secreted from blood into the filtrate Loop of Henle Distal tubule Collecting duct Reabsorption – water is reabsorbed back into blood. Final product is called urine. Pages 316 - 325 Water Balance The solute concentration of blood remains constant despite variations in the amount of water we consume: If water intake is too high the kidneys allow more water to pass into the urine If water is scare, the kidneys conserve water by producing concentrated urine Osmotic Pressure Osmotic pressure is the force generated by water as it moves via osmosis The greater the concentration gradient the higher the osmotic pressure Osmotic pressure affects many cellular activities, especially the exchange of matter between cells and blood. Blood volume influences blood pressure, affecting the health of your cardiovascular system Regulating the Reabsorption of Water The hypothalamus regulates mechanisms maintain homeostasis: •Hunger •Thirst •Blood pressure •Body temperature •Fluid balance •Salt balance Osmoreceptors in the hypothalamus measure osmotic pressure When you are dehydrated, blood concentration increases and osmotic pressure increases Osmotic receptors send a signal to the pituitary gland to release ADH (antidiuretic hormone) ADH travels through the blood to the kidneys and increases the permeability of the distal tubule and collecting duct, allowing more water to be reabsorbed If blood plasma is too dilute, osmotic pressure is low Osmoreceptors stop or prevent the release of ADH The distal tubules and collecting duct become less permeable to water; more water is excreted in the urine. Reabsorption of Salts A drop in blood Na+ concentration triggers a release of the hormone aldosterone Aldosterone stimulates the distal tubules and collecting ducts to reabsorb Na+ Urine Analysis Analyzing the physical and chemical composition of urine enables physicians to make inferences about an individual’s health Disorders of the Excretory System Common excretory system disorders: Urinary tract infection (UTI) – due to bacterial or viral infection Can affect the bladder or urethra Characterized by urge to urinate, even when no urine is formed Painful urination Brown or bloody urine Kidney Stones – due to crystalline formations in the kidney Maybe caused by: recurrent UTIs, insufficient water consumption, low activity levels Treatment may include ultrasound shock waves to break down stones to be passed via urethra; large stones may require surgery Problems with Kidney Function Nephrons can regenerate and restore kidney function after short-term injuries. A person can survive on as little as 1/3 of one kidney. If 75% or more of the nephrons are destroyed, urine output is inadequate to maintain homeostasis Kidney function may be replaced by kidney transplant or through dialysis Dialysis Two types of dialysis: Hemodialysis – artificial membrane in an external device acts as an artificial kidney Peritoneal dialysis – utilizes the peritoneum (intestinal membrane) as the dialysis membrane. Hemodialysis Peritoneal Dialysis Kidney Transplant Dialysis is not intended to be a long-term treatment for kidney failure Kidney transplant organs can come from cadaveric donors or from living donors Individuals can function normally with one kidney The success rate of kidney transplant is 9095% with the aide of anti-rejection drugs