View slides - AMSUS Continuing Education

TRAINING THE FORWARD DEPLOYED SURGEON:
IS ACS FELLOWSHIP THE ANSWER?
William Scott, DO
General Surgery Resident (PGY 4)
Nellis AFB, Las Vegas, NV
Disclosures
• The presenter has no financial relationships to disclose.
• This continuing education activity is managed and accredited by Professional
Education Services Group in cooperation with AMSUS.
• Neither PESG,AMSUS, nor any accrediting organization support or endorse any product or service mentioned in this activity.
• PESG and AMSUS staff has no financial interest to disclose.
• Commercial support was not received for this activity.
• The views and opinions herein are the author’s own private views and are not to be construed as official or reflecting the views of the US Air Force,
Department of Defense, or the United States Government.
Learning Objectives:
At the conclusion of this activity, the participant will be able to:
1. List the skill sets needed by a forward deployed surgeon.
2. Identify the role of the Acute Care Surgery (ACS) Fellowship curriculum in training the deployed surgeon.
3. Discuss the strengths of the fellowship curriculum is preparing the forward deployed surgeon.
4. Recognize the opportunity for comparable training of general surgeons unable to complete an ACS fellowship prior to deployment.
Personal Background
• 4 th year surgical resident at Nellis AFB, Las Vegas, NV.
• After an internship, spent 4 years as a General Medical Officer at Nellis AFB in the Family Medicine clinic
• 2 tours
• Afghanistan 2009
• Liberia 2011
• Returned to residency in 2012
Background
• Varied skills are required at the first echelon of surgical care
• These operations are the first stage of complex surgical care
• Staffing at forward surgical units is not uniform
• The general surgeon must perform a range of surgical specialty operations
• The typical military general surgeon does not possess the diverse skill set needed
• Would training in an acute care surgery (ACS) fellowship fill this knowledge gap?
Methods
• Joint Trauma Theater Registry was queried for procedures performed at forward surgical units from 2002-2012
• These procedures were then organized by type
• Procedures were compared to the revised 2014 ACS fellowship case requirements
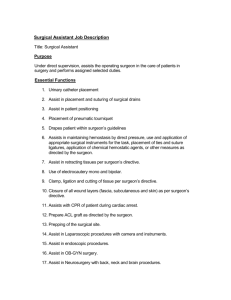
ROLE I - TIC
Battalion
Aid Station
ROLE II - FOB
Forward
Surgical
Team
ROLE III – BAF/KAF
Combat
Support
Hospital
ROLE IV - LRMC
Definitive
Care
REVISED 2014 ACS FELLOWSHIP CASE REQUIREMENTS:
Head and Neck
Organ Management
ICP – 5
Nasal Packing – 2
Trachostomy – 10
Crichothyroidotomy – 2
Thoracic
Thoractomy – 10 pleura – 5
Throacoscopy – 10
Sternotomy – 10
Pericardiotomy – 5
Organ Management
Lung – 35
Operative evacuation of the
Parenchymal procedures – 10
Broncoscopy – 20
Diaphgram – 5
Cardiac – 5
Esphagus – 2
Intrathoracic great vessel injury – 3
Case Requirements
Abdominal
Endoscopy – 20
Enteral Access – 10
Laparotomy – 10
Diagnostic laparoscopy – 5
Hepatic Mobilization – 2
Damage control technique – 10
Complex laparoscopy – 10
Organ Management
Liver – 5
Spleen – 2
Kidney – 3
Pancreas – 5
Stomach – 5
Duodenum – 2
Small Intestine – 10
Colon/Rectum – 10
Appendix – 15
Anus – 5
Biliary System – 3
Bladder – 3
Ureter – 1
Case Requirements
Vascular
LMVR – 2
RMVR – 5
Infrarenal aorto-pelvic exposure – 3
Brachial exposure – 3
Femoral – 5
Popliteal – 2
Retrograde balloon occlusion of the aorta –
Ultrasound
FAST – 25
Thoracic ultrasound for function – 15
Thoracic ultrasound for drainage – 5
Ultrasound guided central line insertion – 5
5
Organ Management
Arterial injury – 10
Amputation – 3
Fasciotomy – 5
Results
• Over a 10 year period (2002-2012)
• 34,411 procedures performed on 9,363 patients
• Mean age 25.9 years
• 80.6% injuries were battle related
Results
• Dominant injuries demographics:
• Explosive: 59.2% were penetrating and 38.1% were blunt
• 48.3% were injured during OIF
• 51.6% were injured during OEF
• Mean ISS of these patients was 12.4 (IQR 5-17).
ISS Example
Trauma.org
Results
• The 34,411 procedures were grouped into categories
• 27,439 operative procedures
• 6,972 non-operative but critical procedures
• 2,279 FAST exams
• 1,735 splint/casting
• 1,040 tube thoracostomies
• 1,918 ICU patients managed
• 2,157of the operative cases were primarily orthopedic
• 758 amputations
• 501 definitive internal fixation
Operative Cases
Soft Tissue (26%)
Vascular (19%)
Ex Fix (13%)
Alimentry Tract (12%)
Laparotomy (including
Diaphram) (11%)
Fasciotomy (9%)
Other (8%)
Thoracic (4%)
Critical Non-operative Procedures
FAST (33%)
Splint/Cast (25%)
Tube Thoracostomy
(15%)
ICU Management
(28%)
Results
• 99.7% of these procedures are part of the ACS fellowship curriculum
• 27 operative cases were not included in the fellowship curriculum
• 3 gynecologic operations and 24 burns/grafting
Take Home Thought #1
• The ACS curriculum replicates the operative and non-operative skill sets needed by forward deployed surgeons
Why don’t we do this with everyone?
• Cost of training
• Budgeting costs for additional trainees
• Lost man hours during training
• Lag time until trainees enter deployment pool
• Accrual of commitment by trainees
• Duty station limitations after training to maintain skill set
• Limited locations
• Current combat injury survival implies forward surgical care is adequate
• Survivability scores
Cost of Training
• Budgeting for more ACS fellowship trained physicians
• Rank pay over 2 year period
• Change in Bonus pay from general surgeon to trauma surgeon
• Lost work during training
• 2 years missing a general surgeon at current duty station
• 2 years that you
Cost of Training
• Lag time until trainees enter deployment pool
• 2 years missing a general surgeon who can deploy
• Accruing further commitment time
• 2 years of commitment for fellowship (4 years total of opportunity cost)
• 2 years of payback will likely increase deployment exposure
Limited Duty Stations
• Duty stations that allow maintenance of this skill set are limited
• Larger Military Treatment Facilities (MTFs)
• Civilian training agreements
• Decreases the available general surgeons who are needed to staff non-acute care locations
Current Efficiency
• Combat injured who reached role III had a > 90% survivability over this period
• Nessen et al showed that FSTs could provide comparable care to other locations in the deployed setting
• No data on what level of training and/or experience of the individual surgeon’s had at role II facilities and whether complications/mortality differed
Take Home Thought #2
• While the ACS curriculum is clearly the best training model and correlates with the training regime best suited for the forward deployed surgeon, the opportunity cost limits the number of available spots that can be set aside each year
What’s the alternative?
• If we can’t send everyone to ACS fellowship, what can we do to prepare them for the front line surgical experience?
The current training model
• General Surgery residency
• Orthopedic residency
• Pre-deployment Training
• Center for the Sustainment of Trauma and Readiness Skills (C-STARS)
• Sustained Medical And Readiness Training (SMART)
• Emergency War Surgery (EWS)
• Advanced Surgical Skills for Exposure in Trauma (ASSET)
CSTARS
• St. Louis, Baltimore, Cincinnati
• 21-day course that offers:
Trauma lectures
Human Simulator Sessions
Human Cadaver Lab
Baltimore City Ambulance Rotation
Trauma Resuscitations in the STC Trauma Resuscitation Unit (TRU), ICU, ER and John’s Hopkins Regional burn ICU
Equipment Skills Stations
Maryland State Trooper Helicopter rotation (as available)
Trauma/Critical Care case studies
Clinical duties as determined by specialty
SMART
• Las Vegas
• 14 day experience with focus on direct patient care
• Tailored to rotator’s identified needs / weaknesses
• Includes traumatically injured as well as emergency general surgery cases
• Includes an emphasis on ICU concepts and care
• Additional informal discussions of current literature and practices with embedded faculty
• Has flexibility to include other surgical specialties as desired
EWS
• San Antonio
• Developed in 1991
• 3 day refresher/review course
• 20 hours of trauma lecture
• 6.5 hours of human cadaver lab
• Reviews war wounds, shock and resuscitation, damage control, injury patterns, etc.
ASSET
• Multiple locations nationwide
• 1 day course
• Reviews anatomy for trauma surgery exposure
• Cadaver lab with practice dissections
Waving Goodbye
• Courses often waived because of small spin up time prior to deployment
• Many surgeons “get out” of this training and “slip through the cracks”
Take Home Thought #3
• General Surgery Residency alone is not sufficient training
• Ideal training simulates the ACS fellowship experience
• Current options that mirror this curriculum are limited to
C-STARS, EWS and the SMART programs
Thank you for your time
Questions?
Obtaining CME/CE Credit
If you would like to receive continuing education credit for this activity, please visit: http://amsus.cds.pesgce.com