CHAPTER 6
advertisement

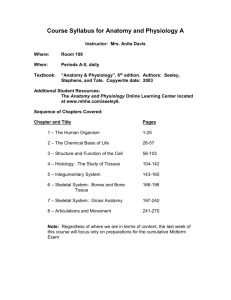
CHAPTER 6 HEAD TRAUMA OBJECTIVES A. Understand basic intracranial anatomy & physiology B. Evaluate a patient with a head injury C. Perform the necessary stabilization procedures D. Determine the appropriate disposition of the patient Introduction 10 % of head injury die prior to reaching a hospital Head injury can be divided: – mild ( 80 % ) – moderate (10 % ) – severe (10 % ) avoid secondary brain damage ( support vital signs, avoid & treat IICP ) Obtaining a CT Scan should not delay patient transfer ( transfer patient early ) Neurosurgical consult essential Neurosurgen need know 1. Age of patient & the mechanism and time of injury 2. Vital signs ( particular the blood pressure ) 3. Results of minineurologic examination ( GCS score; particular the motor response, and pupillary reaction ) 4. Associated injury 5. Results of the diagnostic studies ( CT scan ) Anatomy & Physiology SCALP – S: Skin – C: Connective tissue – A: Aponeurosis / galea aponeurotica – L: Loose areolar tissue – P: Pericranium – Pitfalls Bleeding from Scalp laceration will result in shock ( especialling in children ) Anatomy & Physiology Brain – Cerebrum 1. Frontal: emotion, motor function & expression of speech ( motor speech areas ) 2. Parietal: sensory & spatial orientation 3. Temperal: memory function, responsible for speech 4. Occipital: vision – Brain Stem 1. Midbrain: reticular activating system 2. Pons: reticular activating system 3. Medulla: cardiorespiratory center 4. Cerebellum: coordiration & balance Anatomy & Physiology Tentorium – Supratentorial compartment ( anterior & middle cranial fossa ) » – Uncal herniation ( Supratentorial pressure ): ipsilateral pupillary dilation & contralateral hemiplegia Infratentorial compartment ( posterior fossa ) Anatomy & Physiology Intracranial Kicp Pressure: Hemostasis VCSF + VBl + VBr Pitfalls: A normal intracranial pressure dose not necessarily exclude a mass lesion ( compensation stage ) Intracranial Pressure Pressure / Volume Curve ICP Herniation 10 point of decompensation volume of mass keep the patient’s pressure & volume in the flat portion of the curve, rather than to treat the patient at the point of decompensation Increased Intracranial Pressure( IICP ) Result in – Decreased cerebral perfusion pressure ( CPP ) » CPP : Mean Arterial Blood PressureICP – Altered level of consciousness Anatomy & Physiology Autoregulation of Cerebral blood flow ( CBF ) Noninjured person: CBF is consiant between mean blood pressure of 50 and 160 mm Hg Head-injured patient: autoregulation is often disturbed, so he vulnerable to secondary brain injury due to ischemia from hypotensive episode ( keep vital signs is very important ) Classification of Head Injury Mechanism Severity of injury of injury Morphology of injury ( base on CT scan ) Classification of Head Injury Mechanism of injury – Blunt: automobile collision, fall & assault – Penetrating: gunshot wounds, other penetrating injuries Classification of Head Injury Severity – Coma: GCS sore =< 8 – Mild: GCS score 14 ~ 15 – Moderate: GCS score 9 ~13 – Severe: GCS score 3 ~ 8 Classification of Head Injury Morphology of Injury – Skull fractures – Intracranial lesions Skull fractures Vault: linear / stellate, depressed / nondepressed, open / close Basilar (diagnosed by CT bone window): raccoon eyes, Battle’s signs (retroauricular ecchymosis), CSF leakage and 7th nerve palsy Intracranial Lesions Focal lesions Diffuse lesions Intracranial Lesions Focal lesions: Epidural hematoma: – most due to tearing of the middle meningeal artery – prognosis is usually excellent ( underlying brain injury is limited ) – CT: biconvex or lenticular in shape – Pitfalls: classical lucid interval and ‘talk and die’ Intracranial Lesions Focal lesions Subdural hematoma: – brain damage much more & prognosis is much worse than EDH – tearing of a bridging vein Intracranial Lesions Focal lesions Contusions and intracerebral hematomas: – most occur in the frontal & temporal lobes – always seen in association with SDH Intracranial Lesions Diffuse injuries – Mild concussion: temporary neurologic dysfunction, confusion & disorientation without or with amnesia – Classic cerebral concussion: 1.Transient & reversible loss of consciousness, returns to full consciousness by 6 hrs. 2.No sequelae other than amnesia for the events 3.post-concussion syndrome: memory difficulties, dizziness, nausea, anosmia & depression Intracranial Lesions Diffuse injuries: – Diffuse axonal injury ( DAI ) 1.prolonged postraumatic coma that is not due to a mass lesion or ischemic insults 2.usually having decortication or decerebation posture 3.autonomic dysfunction: hypertension, hyperhidrosis & hyperpyrexia Assessment of Head injury History Mechanism of injury Pre and post injury status Document / communicate Reassess Assessment Vital Signs Identifies neurologic & systemic status Presume hypotension due to hypovolemia, not head injury Minineurologic Exam Purpose Determine severity of brain injury Detect deterioration Categories injuries Minineurologic Exam Level of consciousness - GCS – eye opening – verbal – motor Pupil Motor lateralization ( mass lesion ) Minineurologic Exam Pupils Equality Briskness of response Anormal: >1 mm difference in size Minineurologic Exam Extremity Movement Equality Pain response Lateralized weakness - mass lesion Minineurologic Exam Repeat & compare Detect deterioration initiate treatment Neurosurgical Consultation Minineurologic Exam Don’t presume altered status due to alcohol / drugs ingestion Diagnostic Procedure CT: – be obtained in all head -injury patients ( ideally ), especially there is a history of more than a momentary loss of consciousness, amnesia or severe headaches C-Spine Alcohol level & urine toxic screen Skull X-ray: – penetrating head injury or when CT scan is not immediately available Head injury Management Management Goals Establish diagnosis Assure brain metabolism & prevent secondary brain injury Consult Neurosurgen early or early transfer Head injury Management Management of Mild head injury Normal CT : 1. Brought back to ER if need ( Headinjury warning discharge instructions ) 2. No companion ==> Admission or observe at ER Abnormal CT : Admission Head-injury Warning discharge Instruction Drowsiness or increasing difficulty in awaking patient ( Awaken patient every 2 hrs ) Nausea or Vomiting Convulsion or fits Bleeding or Watery discharge from the nose or ear Severe headache Weakness or loss of feeling in the arm or leg Confusion or strange behavior One pupil larger than the other, double vision or visual disturbance Very slow or very rapid pulse, or an unusual breathing pattern Head injury Management Management of Moderate Head Injury GCS 9 ~ 13 All need brain CT All need to be admitted, even if CT scan is normal Head injury Management Management of Severe Head Injury GCS 3 ~ 8 Prompt diagnosis & treatment is of utmost import ( wait and see = disastrous ) Primary survey : Cardiopulmonary stabilization be achieved rapidly Secondary survey : >= 50 % had additional major systemic injury Minineurologic Examination : reliable minineurologic examination prior to sedating or paralying the patient Medical Therapies for Head Injury Goal: To prevent secondary damage to an already injuried brain Medical Therapies for Head Injury Intravenous Fluid: – 1. Keep euvolemic status, dehydration is more harmful ( vital signs stable ) – 2. Not to use hypotonic or glucosecontaining fluids Hyperventilation: – 1. Keep PaCO2 at 25~30 mmHg when the presence of raised ICP – 2. PaCO2 < 25 mmHg is avoided ( vasoconstriction ==> CBF ) Medical Therapies for Head Injury Mannitol: Indication: – 1. Comatous patient who initially has normal, reactive pupils, but the develops pupillary dilatation with or without hemiparesis – 2. Patient with bilaterally dilated and nonreactive pupils who are not hypotensive Dose ( bolus ) : 1 g/Kg Lasix : Be used in consultation with a neurosurgeon Medical Therapies for Head Injury Steroid : – Not demonstrated any beneficial effect Anticonvulsants – High incidence of Late epilepsy: 1. Early seizure occurring within the first week 2. An intracranial hematoma 3. Depressed skull fracture – phenytoin reduce the incidence of seizure in the first week of injury but not thereafter Restlessness Identify etiology: – Pain – Hypoxia or shock Correct cause: – Analgesics / Sedatives – Ventilation / Treat shock Summary In a comatose patient, secure & maintain airway ( endotracheal intubation ) Moderately hyperventilation, keep PaCO2 at 25~35 mmHg Treat shock aggressively Resuscitate with normal saline or Ringer’s lactate ( avoid hypotonic or glucose-containing fluid ) keep euvolemic status Summary Avoid the use of long-acting paralytic agents Perform a minineurologic examination after stabilizing the blood pressure and before paralying the patient Exclude cervical spine injury Contact a neurosurgeon as early as possible Frequently reassess the patient’s neurologic status