Board Review
advertisement

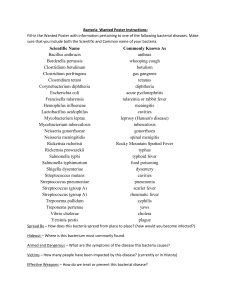
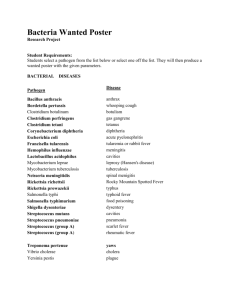
Board Review Paul O’Keefe April 16, 2003 Skin/Soft Tissue Infections • Impetigo • Cellulitis • Fasciitis Impetigo – Group A streptococcus, Staphylococcus arueus – Superficial blistershoney colored crusts on erythematous base – No systemic signs – Mainly in children – May be associated with glomerulonephritis – Treat with penicillin/antistaphylococcal penicillin Cellulitis • Deeper infection usually involving skin and subcutaneous tissue • Erythema, pain and swelling often with distinct border (erysipelas) • Fever and lymphangitis or adenitis common • Gp A streptococcus, Staphylococcus aureus most common • Treat with antistaphylococcal penicillin unless culture positive Necrotizing Fasciitis • Streptococcal gangrene (Gp A strept) • Deeper infection involving fascia and often muscle • Extreme toxicity and rapid spread (“flesheating virus”) • May have associated toxic shock • Treatment – surgical removal of necrotic tissue and antibiotics – Penicillin and clinidamycin A three year old boy presents with an itchy rash that is spreading. Afebrile with numerous cursted lesions in erythematous base involving left shoulder and upper chest and back with few lesions in the right thigh. Culture growing gram positive coccus, beta hemolytic on SBA, catalase negative, inhibited by bacitracin disc. The isolated agent is • • • • • Staphylococcus aureus Coagulase negative staphylococcus Streptococcus pyogenes Sterptococcus pneumoniae Enterococcus faecalis A 13 year old develops high fever and a severely painful red rash on the right arm beginning at the site of a minor laceration. He has high fever, hypotension and extreme toxicity. The arm is red, very swollen, firm and there are areas of black discoloration of the skin. The remainder of the skin has a red sunburned appearance. The extreme toxicity is thought to be caused by A. B. C. D. E. Streptolysin O Hyaluronidase M Protein Pyrogenic exotoxin Peptidoglycan Upper Respiratory Tract Infection • Pharyngitis • Sinusitis • Otitis media Pharyngitis • • • • Viral Group A streptococcus (S. pyogenes) Corynebacterium diphtheriae Infectious mononucleosis Characteristics of Pharyngitis Agent Exudate Lymph nodes Treatment Penicillin Gp A strept + Submandibular Viral - + C. Diphtheriae Membrane Infectious mononucleosis + None “Bull neck” Antitixon Erythromycin, Penicillin Diffuse None Pharyngitis and Fatigue A 15 year old presents with fever, sore throat and extreme fatigue. Temperature is 103.2 and there is a yellowish exudate covering both enlarged tonsils. Submandibular, anterior cervical, and posterior cervical lymph nodes are enlarged on both sides. Which of the following is most characteristic of infectious mononucleosis? • • • • • Atypical lymphocytosis Positive culture for Group A streptococcus Neutrophilia with left shift Low serum globulin Hematuria Sinusitis A 15 yo woman presents with fever, facial pain and severe nasal congestion. She has been suffering with hay fever. CT showed opacification of the R maxillary sinus and an airfluid level in the left. Gram stain of material obtained by antral puncture disclosed gram negative coccobacilli. Which of the following characterizes the organism most likely responsible for the infection? • • • • • Requires neither X nor V factor for growth Requires X factor but not V factor Requires V factor but not X factor Requires both X and V factors Exuberant growth on sheep blood agar Otitis Media A 9 month old child with fever and congestion is diagnosed with right otitis media. Common causes of this infection are? • Gp A streptococcus and Gp B streptococcus • Neisseria meningitidis and Streptococcus pneumoniae • Streptococcus pneumoniae and Haemophilus influenzae • Haemophilus parainfluenzae and Gp A streptococcus • Staphylococcus aureus and Gp A streptococcus Community Acquired Pneumonia • • • • • • Streptococcus pneumoniae Mycoplasma pneumoniae Legionella pneumophila Haemophilus influenzae Chlamydia pneumoniae Tuberculosis Community acquired pneumonia A 33 year old male presents with fever and cough 3 weeks after his 7 year old son was treated for pneumonia. X-ray shows a patchy bronchopneumonia involving the right middle and lower lung field. Cold agglutinin test is positive What is the likely cause? Features of Community Acquired pneumonia S. pneumoniae Mycoplasma Legionella pneumophila Onset Sudden Gradual Less sudden X-ray Lobar Bronchopneumonia Can be lobar Other features Rusty sputum, +blood cultures Cold agglutinins Diarrhea, negative culture Treatment Penicillin, ceftriaxone, vancomycin Macrolides, tetracycline Macrolides, quinolones Communinty Acquired Pneumonia A 26 year old woman complained of fever, night sweats and cough for 2 months. She had occasional hemoptysis and 15 pound weight loss. Chest x-ray showed fibronodular infiltrates with a cavity in the posterior segment of the right upper lobe. Please answer the following: What type of isolation would you order? What diagnostic tests would you order? Sputum smear returned positive for AFB. What treatment would you order? Why are multiple drugs necessary for treatment of tuberculosis? Food Poisoning Agent Mechanism Incubation Clinical S. Aureus Enterotoxin 1-8 h Nausea, vomiting, diarrhea B. Cereus Toxin 4h Diarrhea Clostridium perfirngens Sporulation toxin 8-16 h Diarrhea 12-48 h Fever, pain and diarrhea Salmonella Infectious Diarrhea Fever Fecal WBC Inoculum Other E. Coli - - ? Lactose + V. cholerae - - 107 Comma, TCBS Salmonella + + 105 Non lactose Shigella + + 102 Non lactose C. jejuni + + 104 Seagull E. coli O157:H7 + - ? Meat, HUS + 108 Pets, adenitis Enterotoxin Invasive Y. + Enterocolitic a Cause of diarrhea 4 hours after eating fried rice • • • • • • • B. cereus S. aureus Salmonella Shigella C. jejuni Yersinia enterocolitica Vibrio parahemolyticus Contaminated poultry is the most likely source of • • • • • Salmonella Vibrio cholerae Shigella dysenteriae Campylobacter jejuni S. aureus An important virulence factor of the organism found on biopsy of the stomach in patients with chornic epigastric pain is • • • • • Enterotoxin Polysaccharide capsule Endotoxin Urease Beta-lactamase Urinary Tract Infection A 23 year old woman presents with acute dysuria one day after intercourse. Urinalysis discloses 15-20 WBC’s /HPF. Gram stain discloses gram negative rods. What is the recommended treatment? • • • • • Penicillin V Erythromycin Trimethoprim/sulfamethosoxazole Gentamicin Clindamycin Which of the following strongly favors the diagnosis of pyelonephritis? • • • • • Burning on urination Hematuria Suprapubic tenderness Fever WBC casts on urinalysis Causes of Meningitis by Age Neonate E. coli, Gp B streptococcus, Child – 3 months-5 years Haemophilus infulenzae (no longer), S. pneumoniae Adolescents, Young adults (age 5-40) Neisseria meningitidis, Streptococcus pneumoniae Older adults Streptococcus pneumoniae, Listeria Listeria Meningitis A 6 year old boy presents with fever and lethargy. He has nuchal rigidity on examination. Lumbar puncture discloses many PMN’s and Gram positive cocci in pairs. Which of the following characterizes this organism? • • • • • Beta hemolytic on sheep’s blood agar Inhibited by bacitracin dise Inhibited by optichin disc Beta-lactamase positive Growth on MacConkey agar Vaccines are available to prevent meningitis caused by which organisms ? • • • • • E. coli and Streptococcus pneumoniae Haemophilus influenzae and Listeria monocytogenes Group B streptococcus and E. coli Neisseria meningitidis and Haemophilus influenzae Streptococcus pneumoniae and Group B streptococcus Bone and Joint Infections A 22 year-old woman with sickle cell disease presents with fever and pain in the left upper arm. X-ray of the humerus shows a lytic lesion. Biopsy is growing gram negative Bacilli. Which of the following best describes the organism? • • • • • Comma-shaped with single polar flagellum Motile and oxidase positive Nonmotile facultative anaerobe Motile and does not ferment lactose Coccobacilli that require X and V factors Sexually Transmitted Diseases A 16 year old man presents with burning on urination and a scant urethral discharge 3 days after intercourse with a new partner. Gram stain of discharge discloses many PMN’s but no bacteria. The organism most likely responsible for the infection is • Gram positive coccus, catalase positive • Gram positive coccus, catalase negarive, betahemolytic • Has infectious elementary body and intracellular reticulate body • Gram negarive coccus, oxidase positive • Gram negarive rod, ixidase negarive lactose fermenting Arthritis A 29 yo female presents with fever, rash and arthritis 5 days after onset of menses. She has a new sex partner. Exam discloses about 25 papular lesions on distal extremities and inflamed tendon sheaths of the wrists and ankles with painful motion but no fluid in the joints. Cultures of blood and endocervix are growing • Catalase positive, gram positive coccus • Gram negative coccus that ferments glucose but not maltose • Gram negative coccus that ferments glucose and maltose • Gram negative coccus that requries X and V factors for growth • Gram negative bacillus that ferments lactose Neisseria gonorrhoeae undergoes antigenic variation by altering • Antigenic structure of pilus or expression of outer membrane protein II • Antigenic structure of OMP II or expression of OMP I • Expression of polysaccharide capsule • Antigenic structure of pilus and expression of OMP I • Expression of cytochrome c (Oxidase) Lesion A 32 yo homosexual man presents with a painless lesion on the penis of one week’s duration. It developed 3 weeks after unprotected sex with an anonymous partner. The cause of the infection is identified from a specimen obtained from the lesion which shows. • • • • • Gram negative coccobacilli Gram positive cocci in clusters Gram negative diplococci Gram negative bacilli Motile corkscrew-shaped organisms on darkfield microscopy Response to Treatment A 20 yo asymptomatic woman in the 6th week of pregnancy has a positive RPR of 1:16. FTA Abs is positive. She is treated with 3 doses of benzathine penicillin. Follow up testing after treatment should demonstrate • Progressive rise in RPR and reversion of FTA Abs to negative • No fall in RPR and reversion of FTA to negative • Progressive fall in RPR and reversion of FTA to negative • Progressive fall in RPR while FTA remains positive • No change in RPR while FTA remains positive Discharge A 33 yo sexually active woman complains of vaginal discharge. Examination of the greenish frothy discharge discloses pH of 5.5 with numerous WBC’s and organisms with a jerking motion on saline wet mount. Treatment is best accomplished with • • • • • Doxycycline for 5 days Metronidazole – single dose Ciprofloxacin – single dose Ceftriaxone intramuscular – one dose Benzathine penicillin G IM – one dose Fever and Abdominal Pain An 18 yo woman presents with fever and lower abdominal pain. She has recently had intercourse with a new partner. Pelvic examination discloses vaginal discharge, pain on motion of the cervix and bilateral adnexal fullness. Causes of these symptoms include? • • • • • Neisseria gonorrhoeae Treponema pallidum Chlamydia trachomatis E. coli, Prevotella bivia, enterococcus Herpes simplex Vaginitis A 35 year old woman complains of scant vaginal discharge and itching. Exam discloses erythema of the vaginal mucosa with patches of white discharge. The pH is 4.3. What is appropriate treatment for this condition? • • • • • Metronidazole for 5 days Ciprofloxacin – one dose Doxycycline for 5 days Topical acetic acid Topical miconazole Zoonoses Plague – Yersinia pestis • Highly virulent, encapsulated, small gram negative rod • Endemic in wild rodents Europe and Western N. America • Transmitted by flea • Virulence: endotoxin, exotoxin, proteins • Spreads to nodes – Buboes, severe sepsis • Pneumonic plague – droplet spread • Diagnosis – aspirate bubo, blood (careful in lab) • Treatment – Gentamicin, Streptomycin, tetracycline Pastuerella multocida • Short, gram-negative rod • Cellulitis or osteomyelitis following cat bite or dog bite • Treatment penicillin Anthrax – Bacillus anthracis • Gram positive, spore-forming rod with capsule “Box cars”. Spores in soil, on animal productrs • Enter through skin, alimentary, respiratory tracts • Toxin: Protective antigen, edema factor (cyclase), lethal factor • Painless ulcer with marked local edema • Pneumonia (mediastinitis) meningitis • Necrotizing enteritismeningitis • Diagnosis-culture • Treatment: ciprofloxacin+clindamycin+rifampin, penicillin if susceptible Gram Stain - CSF Tularemia • Francisella tularensis – small gram negative rod, enzootic in wild animals (rabbit) • Transmission – ticks or contact with dead animal • Clinical – Ulceroglandular – ulcer with swollen regional lymph nodes – Typhoidal – fever, adenopathy – Pulmonary • Diagnosis – Culture dangerous in lab; serology and direct fluorescence • Treatment – Gentamicin or tobramycin Brucellosis • Small, slow growing gram negative rod • B. melitensis (goats, sheep), B. abortus (cattle), B. suis (swine) • Transmission – Occupation, milk • Small granulomas in lymph nodes, spleen, marrow • Fever, weakness, fatigue • Diagnosis – cluture blood and tissue, serology • Treatment – tetracycline, gentamicin Rocky Mountain Spotted Fever • Tick borne rash illness caused by Rickettsia rickettsii, a small gram negative rod. Obligate intracellular parasite. Eastern and Midwestern US • Vasculitis – organism in endothelium • Fever, headache, weakness followed by rash, DiC and shock • Diagnosis: Clinical, serology, ElISA, Weil Felix (Culture dangerous) • Treatment – Doxycycline Q Fever • Coxiella burnetti • Transmission – contact with infectious aerosol from cattle, sheep, goats. Parturient cats • Fever, headache, cough; frequent hepatitis, endocarditis • Diagnosis – serology • Treatment – Doxycycline Lyme Disease • Borrelia burgdorferi – spirochete transmitted by Ixodes ticks – Reservoir – field mice and deer • • • • Erythema migrans, meningitis, encephalitis Heart disease, arthritis Diagnosis – Serology ELISA and Western blot Treatment – Doxycycline, amoxicillin, ceftriaxone Fungi Histoplasmosis • Dimorphic fungus – mold in soil, yeast in tissue • Ohio and Mississippi river valleys, disturbed soil with bird droppings, bat caves • Small oval yeast in macrophages • Clinical – Pulmonary – acute pneumonia, chronic like tuberculosis – Disseminated in immunocompromised – esp AIDS • Diagnosis – Culture, Serology, Antigen in urine • Treatment – Self limited, Itraconazole, Amphotericin b Blastomycosis • Dimorphic fungus – large refractile yeast with broad based budding • Ohio, Mississippi, St. Lawrence river valleys, Great Lakes. Soil with decaying organic material • Clinical – Pulmonary, pneumonia (refractory) – Dissemination to skin common • Diagnosis – culture, histology • Treatment – Itraconazole, Amphotericin b Coccidioidomycosis • Dimorphic fungus – mold in soil, spherule in tissue • Southwestern US (CA, AZ, NM, TX), Mexico. Arthrospores carried by wind • Clinical – Valley fever – flu, pneumonitis, erythema nodosum – Chronic pulmonary – thin-walled cavity, nodule – Disseminated – Filipinos, African Americans, Immunosuppressed, pregnant • Skin, bone, joint. CNS common – chronic meningitis • Diagnosis – Sperules in tissue, culture (DANGER), serology • Treatment – Amphotericin b, fluconazole, itraconazole Candida • Oval yeast with single bud. ‘Pseudohyphae’ in tissue. Many species. Germ tube distinguish C. albicans from others • Impaired defenses: – Mucosal disease – mouth, esophagus, vagina, skin (warm, moist areas) – Greater immune compromise – dissemination to many organs • Diagnosis – seen on KOH, Culture • Treatment – Topical – nystatin, azoles – Systemic – fluconazole, amphotericin b, caspofungin Cryptococcus neoformans • • • • Oval, budding yeast with polysaccharide capsule Ubiquitous in soil containing bird droppings. Inhaled Compromised: AIDS, diabetes, malignancy, transplant Lung infection – Aymptomatic nodule – Pneumonia • Meningitis common • Diagnosis – India ink on CSF, Culture, antigen in CSF and serum (follow titer during treatment) • Treatment – Amphotericin b + flucytosine, Fluconazole Aspergillus • Mold (no yeast form), ubiquitous, several species (A. fumigatus most common), Airborne conidia • Manifestations – Hypersensitivity – sinusitis, asthma-like illness (ABPA) – Mycetoma – fungus ball in pre-existing lung cavity – Invasive – Severely immunocompromised. sinus and lung • Causes thrombosis and infarction • Disseminated especially to CNS • Diagnosis – culture and histology • Treatment – Amphotericin b, Voriconazole, itraconazole Zygomycosis • Mucor, Rhizopus, Absidia – saprophytic molds • Invade blood vessels in paranasal sinuses or lung – Progressive destruction across tissue planes • Diagnosis – culture, histology • Treatment – Surgical debridement – Amphotericin b, newer azoles Fever in Returning Traveler • Malaria if exposed – Africa – falciparum – India – vivix • Blood smear • Chloroquine plus primaquine, Quinine plus doxycycline • Typhoid fever. Fever, rash, splenomegaly • Dengue – fever and headache Scenarios • Returned from Philippines and passed a worm? • Young Mexican immigrant with headache and new seizure. CT Cysts in brain • Sepsis and severe diarrhea in WWII veteran who has just finished chemotherapy for NHL. Eosinophilia and microscopic worm in sputum