An Intraoperative Small Dose of Ketamine Prevents Remifentanil
advertisement

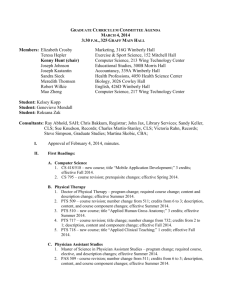
AN INTRAOPERATIVE SMALL DOSE OF KETAMINE PREVENTS REMIFENTANIL-INDUCED POSTANESTHETIC SHIVERING Hilary Wagner RN, BSN, SRNA Oakland University-Beaumont/MSNAnesthesia Class of 2013 Nakusuji, M., Nakamura, M., Imanaka, N., Tanaka, M., Nomura, M., & Suh, S. H. (2011). An intraoperative small dose of ketamine prevents remifentanilinduced postanesthetic shivering. Anesthesia & Analgesia, 113 (3). INTRODUCTION Published in the September 2011 edition of Anesthesia & Analgesia The study was approved by the Human Ethics Review Committee of Kansai Denryoku Hospital in Japan STUDY OBJECTIVES/PURPOSE Postanesthetic shivering (PAS) is frequently encountered in patients after discontinuation of remifentanil infusion Remifentanil is more likely to cause PAS than other opioids However, the exact cause of remifentanilinduced PAS remains undetermined at this time STUDY OBJECTIVES/PURPOSE To investigate whether or not a ketamine infusion while using remifentanil during gynecological laparotomy cases reduces the incidence of PAS STUDY Patients were enrolled in this study from August 2009 to October 2010 Randomized controlled trial Prospective study Dependent variable = Postanesthetic shivering Independent variable = Ketamine infusion INCLUSION CRITERIA ASA status of I or II Under age 60 Surgical time less than 3.5 hours (surgical times longer than 3.5 hours are correlated with PAS) Patients were automatically excluded if they were: undergoing emergency surgery scheduled for radical hysterectomy METHODS Signed written consent form was obtained from each subject 64 patients meeting inclusion criteria were randomly assigned to receive either 0.5 mg/kg ketamine at induction followed by an infusion of 0.3 mg/kg/hr for the duration of surgery (n=32) or a similar volume of saline (n=32). The patients were randomly assigned via envelope randomization METHODS (CONT.) In both groups, all patients received: Midazolam IM (2.5-5 mg) 15 minutes before OR arrival An epidural catheter at the T12-L1 interspace Epidural ropivacaine titrated intraoperatively to maintain systolic arterial blood pressure within 20% or less of preoperative blood pressure General anesthesia induced with propofol at 1.5-2 mg/kg IV and a remifentanil infusion at 0.25-0.5 mcg/kg/min (for analgesia) Vecuronium bromide for tracheal intubation at 0.1 mg/kg IV METHODS (CONT.) Total IV anesthesia with propofol titrated to maintain a target Bispectral Index (BIS) value between 30-50 FiO2 at 0.40 (a mix of oxygen and air, no nitrous oxide was used) 100 mcg of fentanyl via the epidural catheter after closure of the peritoneum 1.25 mg of droperidol at the end of the case to prevent postoperative nausea and vomiting Forced air blanket to lower extremities at 32C which was discontinued when rectal temperature reached 37C Lactated ringer’s solution infused at ambient temperature of 25-27C METHODS (CONT.) The OR staff were unaware as to which patients were part of the experimental and control groups The staff monitored the patients for PAS while in the OR and for 30 minutes post-emergence OUTCOME MEASURES(CONT.) Measured shivering with a 5-point rating scale 0: no shivering 1: peripheral vasoconstriction with no visible muscular activity 2: visible muscular activity confined to only 1 muscle group 3: visible muscular activity in more than 1 muscle group 4: gross muscular activity involving the whole body A score between 3 and 4 indicated PAS METHODS (CONT.) The anesthesia provider remained absent during the PAS evaluation so as not to allow bias related to anesthetic regimen knowledge Postoperative pain was also evaluated using the visual analog scale from 0 (no pain) to 10 (worst pain) PAS was then treated using a warm blanket If PAS persisted longer than 15 minutes, 50 mg of flurbiprofen axetil was administered (COX inhibitor) A flow diagram of inclusion and exclusion criteria applied in this study, based on the CONSORT (Consolidated Standards of Reporting Trials) statement. Nakasuji M et al. Anesth Analg 2011;113:484-487 STATISTICAL ANALYSIS Student t test and the Mann-Whitney U test were used for statistical comparisons Differences between the groups were considered statistically significant when the P value was <0.05 Normality and equal variance tests were applied to all data (expressed as mean ± SD) RESULTS No significant difference in temperature throughout anesthesia between both groups All patients were found to be pain free for 30 minutes post emergence from anesthesia using the visual analog scale RESULTS (CONT.) Incidence of PAS in ketamine group n=2, 6% Incidence of PAS in control (saline) group n=12, 38%, P=0.005 DISCUSSION The study showed that the incidence of remifentanil-induced PAS during the early recovery period was markedly reduced when ketamine was also administered intraoperatively Exact mechanism of this remains to be discovered Other factors which may have influenced the incidence of PAS were well controlled in this study (such as postoperative pain and hypothermia) STRENGTHS Another study demonstrated decreased incidence of PAS when using intraoperative magnesium sulfate (a noncompetitive NMDA receptor antagonist) in patients receiving propofol/remifentanil based anesthesia This suggests that the stimulation of NMDA receptors may be the underlying mechanism of remifentanil-induced PAS LIMITATIONS Small sample size (n=64) Short duration of observation Patients were only observed for 30 minutes after emergence They may have developed PAS after transfer to the GYN floor Cannot entirely exclude the possibility of residual sedative and analgesic effects being the cause of the differences observed CONCLUSION While the mechanism of the reduced incidence of PAS is still not fully understood, ketamine should be considered when using high dose remifentanil during surgery