Diagnosis in the DSM-5
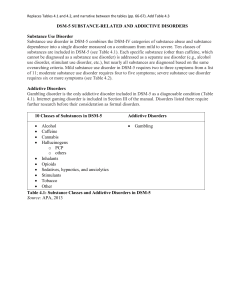
advertisement
Diagnosis in the DSM-5 CHRISTOPHER J. HOPWOOD, PHD MICHIGAN STATE UNIVERSITY Disclaimers This workshop is not affiliated with or endorsed by the American Psychiatric Association There will be additional editorial and content changes to the DSM-5 prior to its publication in May, 2013 Outline The Past: Competing models of psychopathology The Present: Specific changes in the DSM-5 The Edge: DSM-5 personality disorders The Future: DSM-5.1 and beyond Note about slides and handouts Initial Questions What do you use the DSM for? Initial Questions What do you use the DSM for? How do you conduct clinical assessment? Do you use psychometric instruments? What instruments? Initial Questions What do you use the DSM for? How do you conduct clinical assessment? How useful is the DSM for your treatment decisions and clinical predictions? Initial Questions What do you use the DSM for? How do you conduct clinical assessment? Not very, but I need to list something to get reimbursed What instruments? I would rearrange things slightly, but it more or less What theoretical perspective? covers psychopathology, which is one part of How useful is the DSM for your treatment decisions assessment and clinical predictions? It covers psychopathology well, and this is the single most important among domains of assessment It provides most of what you need to know for assessment The Example of Diabetes Diagnosis and treatment in ancient civilizations The Intersection of medical practice and basic research in 18th Century France Contemporary diagnosis and treatment Mechanisms, structure, and function A Clinical Example: MMPI profile 120 110 100 90 80 70 60 50 40 30 L F K HS D HY PD MF PA PT SC MA SI A Clinical Example: Clinical features 32 year old Caucasian Male Born unwanted to an introverted lab-scientist father and fragile factory working mother in a midwestern, predominately Lutheran community Mother often unavailable due to depression and substance use, father often unavailable due to workaholism Had a number of medical complications in early childhood, one of which involved a threat to remove his penis; parents reflected how these experiences drew him “inward” A Clinical Example: Clinical features Developed an interest in anatomy, would frequently kill and dissect animals As a teen, began masturbating to fantasies involving animal parts and male peers Daydreamed about killing and having sex with a jogger who past his home Efforts to be part of social groups routinely failed; began using substances and developed a reputation as a clown for approval Parents relationship deteriorated during his high school, separated when he was 18; was sent to live with relatives Mother kidnapped child, left him alone in house, and instructed him not to report their whereabouts A Clinical Example: Clinical features Went to college briefly but failed and was unable to develop a social network; described as “awkward loner” Began using alcohol to fit in and self-medicate Had difficulties holding a job, fired for absenteeism Began having sex with men in bathhouses Convicted of public exposure; then molesting a 13 year old whom he had given soporiphic before taking nude pictures Court was convinced by remorse, he got 5 years probation A Clinical Example: Clinical features (Nichols, 2007) Killed 17 people in a typical pattern Go to gay bar, invite a man to his home Behave oddly and sometimes have intercourse Develop fears of abandonment when the man motioned to leave Administer soporiphic, play with anatomy Murder the man, play more with anatomy, including canibalism Jeffrey Dahmer A Clinical Example: Clinical features http://www.youtube.com/watch?v=ErB0R4wlB64 A Clinical Example Psychiatric Diagnosis? Traits? Functional Formulation? Implicit Dynamics? Nomothetic Idiographic Outline The Past: Competing models of psychopathology The Present: Specific changes in the DSM-5 The Edge: DSM-5 personality disorders The Future: DSM-5.1 and beyond Theoretical Models of Psychopathology Descriptive Psychiatry Quantitative Psychology The Past: Competing Models of Psychopathology Medical Model The Past: Competing Models of Psychopathology Assumptions of the Medical Model Psychiatric disorders are like any other medical disorder Abnormal and normal behavior are qualitatively different Disorders are qualitatively different from one another Biology is a privileged level of analysis The research goal of taxonomy is to describe symptoms reliably to work backwards to underlying biological cause The Past: Competing Models of Psychopathology Kraepelin 1856-1926 German psychiatrist notable for developing psychiatric taxonomy rooted in biological hypotheses Trained with Wundt, unlike contemporaries in psychiatry advocated detailed behavioral analysis Chapter organization was based on his textbook approach The Past: Competing Models of Psychopathology Adolf Meyer 1866-1950 Swiss psychiatrist who emigrated to US, early APA president Introduced Freud and Kraepelin to US psychiatry Emphasized phenomenology and subjective experience Focused on importance of detailed case history The Past: Competing Models of Psychopathology Anti-Classification Movement Rosenhan study Szasz Laing Humanism Anti-pharmacology The Past: Competing Models of Psychopathology Neo-Kraepelinian Propositions (Klerman, 1978) Psychiatry is a branch of medicine based on science Psychiatry treats people with illness, who are different than people who are not sick There are discrete mental illnesses which are biological in origin Classification should be based on reliable description and hypotheses about underlying biology Feigner, Robins, Guze, and neo-Kraepelinianism Feigner criteria (1972) Clinical description Laboratory studies (biological or psychometric evidence) Delimitation from other disorders Follow-up research (to rule out other explanations) Family study (i.e., behavior genetic research) The Invisible College and reactionary psychiatry (Blashfield, 1984) The Past: Competing Models of Psychopathology The Invisible College and DSM-III (Blashfield, 1984) The Past: Competing Models of Psychopathology The Invisible College and DSM-III (Blashfield, 1984) Robins, Guze, and Washington School The Past: Competing Models of Psychopathology The Invisible College and DSM-III (Blashfield, 1984) Spitzer, Endicott, Fleiss, and NYSPI The Past: Competing Models of Psychopathology Feigner, Robins, Guze, and neo-Kraepelinianism Feigner criteria (1972) Clinical description Laboratory studies (biological or psychometric evidence) Delimitation from other disorders Follow-up research (to rule out other explanations) Family study (i.e., behavior genetic research) The Invisible College and reactionary psychiatry (Blashfield, 1984) DSM-III The Past: Competing Models of Psychopathology Feigner et al. (1972) depression criteria Dysphoric mood 5 of 9 criteria (appetite, sleep, energy, lethargy, anhedonia, guilt, concentration, suicidality) At least one month No other psychiatric or medical explanation The Past: Competing Models of Psychopathology Limitations of the Medical Model Where are the causes and effective treatments? How much is diagnosis influenced by pharma and insurance? Is psychopathology fully reducible to signs and symptoms? What about those complications that Meyer emphasized and his notion of a detailed case history? Did the Washington school ever intend the diagnostic formulation to be complete? Or did external forces reduce clinical assessment to DSM checklists? Psychiatric exclusivity The problem of reviewing for psychiatry journals as microcosmic for the problem of the diagnostic manual being written by a single profession The Past: Competing Models of Psychopathology Limitations of the Medical Model Many aspects of the model are demonstrably wrong With rare exceptions normal behavior is not qualitatively different than abnormal behavior Current psychiatric phenotypes have predictable patterns of comorbidity A number of factors affect functioning and outcomes for persons with psychopathology that are not in the manual The Past: Competing Models of Psychopathology Question Have you ever recorded patient information for purposes not directly to treatment delivery? The Past: Competing Models of Psychopathology What is important about the medical model? Clinical experience Reliable description Biology Pragmatic, categorical worldview Treatment matching The Past: Competing Models of Psychopathology Quantitative Trait Psychology The Past: Competing Models of Psychopathology Assumptions of Quantitative Trait Psychology The nature of psychopathology is a testable question Although multi-method evidence is ideal, people can generally self-report their difficulties Signs reflect real entities plus error (circles and squares) The best way to develop an effective taxonomy and identify treatments is to carve nature at its joints The Past: Competing Models of Psychopathology Two streams Structure of traits – implications for psychiatry Structure of psychopathology – implications for integration with personality The Past: Competing Models of Psychopathology Two streams Structure of traits – implications for psychiatry Structure of psychopathology – implications for integration with personality The Past: Competing Models of Psychopathology Allport 1897-1967 First Personality textbook Trait psychologist who emphasized how everyone is unique Lexical hypothesis Allport & Odbert (1936) The Past: Competing Models of Psychopathology Cattell 1905-1998 Built psychometric models from agriculture and intellectual assessment Spearman, Thurstone, Guilford, Burt Developed the notion of using factor analysis for test development that currently dominates basic personality research Proposed 16 primary traits The Past: Competing Models of Psychopathology The Big Five Digman, Goldberg, Costa, McCrae and others ‘settled’ on the Big Five Neuroticism Extroversion Openness to Experience/Intellect Agreeableness Conscientiousness Wiggins, Widiger, Costa, and many others demonstrated the importance of big five traits to clinical psychology The Past: Competing Models of Psychopathology Two streams Structure of traits – implications for psychiatry Structure of psychopathology – implications for integration with personality The Past: Competing Models of Psychopathology Eysenck Interested in understanding the structure of psychopathology Used factor analysis and experimental research with multiple methods and samples Identified similar factors Neuroticism Extroversion Psychoticism The Past: Competing Models of Psychopathology Achenbach Seminal study in 1966 applying factor analysis to childhood psychopathology Two broad factors Internalizing Externalizing The Past: Competing Models of Psychopathology Krueger Structure of comorbidity (Krueger, 1999) The Past: Competing Models of Psychopathology Trait Hierarchy The Past: Competing Models of Psychopathology Evidence for Traits Cross-cultural validity (Terraciano et al., 2010) Heritability (Hopwood et al., 2011) Links to Biological Structure (De Young et al., 2009) Course (Roberts et al., 2006) Cross-instrument validity (McCrae et al., 2011) Prediction of psychopathology (Kotov et al., 2010; Samuel & Widiger, 2008) The Past: Competing Models of Psychopathology How “personality” are PDs? Samuel & Widiger (2008) Meta-Analysis (16 Independent samples) N E O A C Paranoid 0.40 -0.21 -0.04 -0.34 -0.11 Schizoid 0.22 -0.46 -0.11 -0.16 -0.10 Schizotypal 0.38 -0.28 0.09 -0.17 -0.14 Antisocial 0.18 0.04 0.08 -0.36 -0.33 Borderline 0.54 -0.12 0.10 -0.24 -0.29 Histrionic 0.10 0.33 0.15 -0.11 -0.11 Narcissistic 0.11 0.09 0.07 -0.37 -0.10 Avoidant 0.52 -0.49 -0.08 -0.07 -0.16 Dependent 0.44 -0.15 -0.03 0.08 -0.20 Obsessive Mean Median 0.18 0.31 0.30 -0.12 -0.14 -0.14 -0.04 0.02 0.02 -0.05 -0.18 -0.17 0.24 -0.13 -0.13 Kotov et al. (2010) “Axis I” meta-analysis N E O A C PDs 0.31 -0.14 0.02 -0.18 -0.13 Axis I 0.39 -0.24 -0.09 -0.02 -0.30 Advantages of a quantitative perspective Provides quantitative model for understanding individual differences in psychopathology The Past: Competing Models of Psychopathology Meehl Taxometrics Quantitative procedures to tell if a construct is distributed continuously or not Current evidence – discontinuities are rare (Haslam, 2011) Actuarial prediction All measures are potentially useful – this is a falsifiable question Clinicians are good at picking variables Clinicians are bad at combining variables The Past: Competing Models of Psychopathology Advantages of a quantitative perspective Provides quantitative model for understanding individual differences in psychopathology Provides a model for developing assessment methods The Past: Competing Models of Psychopathology (Cronbach, Meehl and) Loevinger Construct Validation Theory = Content Validity Structure = Structural Validity, Reliability Nomological Network Convergent, Discriminant, Criterion Validity Trait realism Psychological Disorders as hypothetical constructs The Past: Competing Models of Psychopathology Advantages of a quantitative perspective Provides quantitative model for understanding individual differences in psychopathology Provides a model for developing assessment methods Provides a coherent framework within which to understand Comorbidity Heterogeneity The Past: Competing Models of Psychopathology Applying the hierarchy (Hopwood et al., in press) DSM-5 Traits Negative Affect, Detachment, Antagonism, Disinhibition, Psychoticism 25 facets PAI Psychopathology Suicide, Aggression, Treatment Motivation, Social Support, Stress Exploratory Structural Equation Model with target rotation The Past: Competing Models of Psychopathology Applying the hierarchy: Structure (Hopwood et al., in press) Negative Affectivity Submissiveness Separation Insecurity Anxiousness Emotional Lability Suspiciousness Detachment Restricted Affectivity Depressivity Withdrawal Intimacy Avoidance Anhedonia Antagonism Manipulativeness Deceitfulness Hostility Callousness Attention Seeking Grandiosity Disinhibition Irresponsibility Impulsivity Distractability Perseveration Rigid Perfectionism Risk Taking Psychoticism Eccentricity Perceptual Dysregulation Unusual Beliefs Negative Affectivity Detachment Antagonism Disinhibition Psychoticism .27 .48 .70 .59 .32 .01 .04 .20 .11 .28 -.23 .01 -.07 .12 .26 .03 .21 .15 .25 .20 .11 .18 .13 .16 .29 -.34 .15 -.01 -.21 .06 .38 .40 .71 .27 .62 .15 -.07 .09 .05 -.05 .11 .36 .05 .01 .30 .13 .40 .20 .39 .23 .07 .07 .36 -.12 .23 .05 .01 .17 .39 .31 -.32 .03 .52 .41 .58 .54 .39 .52 .18 .28 .32 .14 .16 -.10 .05 .19 -.10 .30 .13 .20 -.06 -.05 .16 .35 .45 -.31 .16 -.10 .08 .20 .20 -.33 .21 .26 -.10 .09 .28 .30 .30 .56 .44 .17 -.34 .56 .45 .19 .25 .32 .18 -.09 .15 .13 .08 .12 .13 .10 .16 .18 .28 .27 .17 -.06 .31 .58 .61 The Past: Competing Models of Psychopathology Applying the hierarchy: “Comorbidity“ (Hopwood et al., in press) Anxiety Disorders Obsessive Compulsive Phobias Traumatic Stress Borderline Features Affective Instability Identity Problems Negative Relationships Self Harm Negative Affectivity Detachment Antagonism Disinhibition Psychoticism .44 .17 .34 -.38 .22 .50 .25 -.04 -.04 .42 .44 .09 .07 .23 .44 .43 .35 .32 .39 .20 .48 .13 -.04 .42 .25 .43 .23 .26 .32 .16 .04 -.06 .30 .47 .32 The Past: Competing Models of Psychopathology Applying the hierarchy: Heterogeneity (Hopwood et al., in press) Negative Affectivity Detachment Antagonism Disinhibition Psychoticism Mania Activity Level Grandiosity .25 -.12 .33 .08 .46 .03 -.29 .46 -.22 .20 Irritability .48 .14 .53 .08 .10 The Past: Competing Models of Psychopathology Applying the hierarchy: Levels of analysis (Hopwood et al., in press) The Past: Competing Models of Psychopathology Applying the hierarchy: How much breadth do you need? (Hopwood et al., in press) Anxiety Insecurity Lability Anger Perfectionism Sleep Problems (.19) .13 .07 .11 Suicidal Ideation (.58) .35 .09 .32 .29 Interpersonal Problems (.63) .39 .23 .18 .39 .07 The Past: Competing Models of Psychopathology Advantages of a quantitative perspective Provides quantitative model for understanding individual differences in psychopathology Provides a model for developing assessment methods Provides a coherent framework within which to understand Comorbidity Heterogeneity Provides a connection between basic science and clinical application The Past: Competing Models of Psychopathology Links to Dynamics Wiggins: Structure of interpersonal behavior commensurate with Agreeableness (warmth) and Extraversion (dominance) Watson: Structure of affect commensurate with Neuroticism (negative affectivity), Extraversion (positive affectivity) The Past: Competing Models of Psychopathology Limitations of a quantitative perspective Primarily studied in normal psychological literature with questionnaires Paradox of broad topics and small concerns Types vs. traits Number of types or traits Best way to rotate factors Best fit indicators Limited efforts to connect to clinical practice in a tangible way Mistrust among clinicians who see the quantitative perspective as “cold” and among psychiatry as “numbery” The Past: Competing Models of Psychopathology Summary There is a clinical need to describe disorders, ideally including underlying biology However, it is important to recognize that to the degree that motives, perceptions, and social contexts affect behavior, psychopathology can not be fully reduced to biological processes without losing important meaning Behaviors are structured by hierarchical personality and cognitive architectures In other words, psychiatric taxonomy needs quantitative clinical psychology The Past: Competing Models of Psychopathology Outline The Past: Competing models of psychopathology The Present: Specific changes in the DSM-5 The Edge: DSM-5 personality disorders The Future: DSM-5.1 and beyond In the beginning Regier et al., 2009: Indictment of Feigner Criteria Comorbidity Non-specific treatment response “combined influence of syndromes…more significant than any of their individual effects” “unlikely to find single gene underpinnings” The Present: DSM-5 In the beginning Regier et al., 2009: Hierarchies “the presence of any disorder would cause the manifestations of disorders lower in the hierarchy” Implicit in Kraepelin, Explicit in Jaspers Lost in DSM-III-R Dimensions “We have decided that one, if not the major, difference between DSM-IV and DSM-V will be the more prominent use of dimensional measures.” The Present: DSM-5 Process 1999 – Goals and White Papers Basic definition Dimensional criteria Development, gender, and culture Neuroscientific research Meetings APA, WHO, NIMH, NIDA, NIAAA Leadership selected by APA: Kupfer, Regier Study Groups Diagnostic Cluster Work Groups Literature Reviews Re-analysis Initial Proposals Comments The Present: DSM-5 Process Field Trials Description Comorbidity Issues with reliability The Present: DSM-5 Description of DSM-5 Field Trials (Clarke et al., 2013) 279 clinicians 2246 patients 86% seen for 2 interviews Diverse in age, ethnicity, geography Certain phenotypes oversampled to ensure adequate base rates The Present: DSM-5 Comorbidity in Field Trials Trimorbid MDD, PTSD, AUD? The Present: DSM-5 DSM-5 Field Trials Reliability Spitzer et al., 2013 Fleiss Standard of kappas in DSM-III, IV .40 = minimum, .70 = good Kappas for DSM-5 field trials dip into .30s, which is a cause for concern Kraemer et al., 2013 “The methodology and understanding of kappa have advanced over the last 30 years” The Present: DSM-5 DSM-5 Field Trials Reliability DSM-III DSM-5 patients selected by clinicians patients referred to clinicians blinding between clinicians taken on trust blinding ensured by design very small samples for low adequate (over) sampling base rate disorders leading to large confidence intervals The Present: DSM-5 DSM-5 Field Trials Reliability Kraemer et al., 2013 Inter-clinician kappas for most areas of medicine tend to be around .40 “It is important that our expectations of DSM-5 diagnoses be viewed in the context of what is known about the reliability and validity of diagnoses throughout medicine and not be unrealistically high” The Present: DSM-5 Rolling out the Manual Work Groups developed revised proposals Comments invited Final proposals passed to committees Scientific Review Clinical Public Health DSM-5 Task Force led by Kupfer and Regier advises APA Board of Trustees APA Board of Trustees makes final decisions Available for purchase currently, available in May 2013 The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 DSM-5, not DSM-V Use of Arabic numerals is meant to reflect a paradigm shift towards greater responsivity Practically: more revisions 5.1, 5.2, 5.3…. Challenge: how to be responsive to research without driving clinicians and mental health systems nuts! Conflict of interest? DSM-5: $200 ICD-10: Public Domain The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 Medicine More dimensional ratings of cross-cutting constructs Developmental organization of disorders Dropped multi-axial format The Present: DSM-5 Multi-Axial Diagnosis Distinctions between “Axis II” and other disorders have been falsified No other medical profession uses a multi-axial model Axis III gets equal status (albeit possibly in a different manual) Cultural/Social issues and Functioning will be incorporated into symptom descriptions or assessed as cross-cutting dimensions The Present: DSM-5 Biology Behavior Genetics GWAS Imaging Psychophysiology The Present: DSM-5 Behavior Genetics Everything is ~50% heritable…and the rest is mostly error However Developmental patterns Eating Disorders Antisocial Behavior: Rule Breaking and Aggression Epigentics GxE GrE The Present: DSM-5 GWAS (Lancet, 2013) Findings from family and twin studies suggest that genetic contributions to psychiatric disorders do not in all cases map to present diagnostic categories. We aimed to identify specific variants underlying genetic effects shared between the five disorders in the Psychiatric Genomics Consortium: autism spectrum disorder, attention deficit-hyperactivity disorder, bipolar disorder, major depressive disorder, and schizophrenia. 33 332 cases and 27 888 controls Our findings show that specific SNPs are associated with a range of psychiatric disorders of childhood onset or adult onset. In particular, variation in calcium-channel activity genes seems to have pleiotropic effects on psychopathology. Overall very few findings highly inconsistent very small effects effects that exist are pleiotropic or can be organized around higher order dimensions The Present: DSM-5 Imaging (DeYoung et al., 2010) The Present: DSM-5 Psychophysiology P300 In general, less deflection is associated with more impulsive, poorer decision making Traditionally examined with alcohol disorders The Present: DSM-5 Psychophysiology (Patrick et al., 2006) Evaluated P300 relation to alcohol, drug, nicotine dependence as well as conduct disorder and antisocial personality Correlation with externalizing pathology = .25 With this correlation covaried, no correlations with specific disorders was significant The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 ICD Current version: ICD-10 ICD-11 scheduled for 2015 DSM-5 connection to ICD reviewed for all symptom criteria Chapter organization designed to bring DSM in line with ICD Developmental Organization across and within chapters The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 Chapter Organization Kraepelinian organization was arbitrary There are non-arbitary ways to arrange disorders Covariance (Krueger, 1999) Development Brings DSM-5 structure in line with ICD as well as other areas of medicine The Present: DSM-5 Chapter Organization: DSM-5 approach Include all mental disorders in Section II List domains of disorder and disorders within domains developmentally Keep classical distinctions (e.g., mood and anxiety) New domains (e.g., obsessive and traumatic) Encourage clinical use and research on content of Section III The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Neurodevelopmental Disorders Intellectual Disabilities Intellectual Disability (Intellectual Developmental Disorder) Global Developmental Delay Unspecified Intellectual Disability Communication Disorders Language Disorder Speech Sound Disorder (previously Phonological Disorder) Childhood Onset Fluency Disorder (Stuttering) Social (Pragmatic) Communication Disorder Unspecified Communication Disorder Autism Spectrum Disorder Autism Spectrum Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Neurodevelopmental Disorders Attention-Deficit/Hyperactivity Disorder Attention-Deficit/Hyperactivity Disorder Other Specified Attention-Deficit/Hyperactivity Disorder Unspecified Attention-Deficit/Hyperactivity Disorder Specific Learning Disorder Specific Learning Disorder Motor Disorders Developmental Coordination Disorder Stereotypic Movement Disorder Tourette’s Disorder Persistent (Chronic) Motor or Vocal Tic Disorder Provisional Tic Disorder Other Specified Tic Disorder Unspecified Tic Disorder Other Neurodevelopmental Disorders Other Specified Neurodevelopmental Disorder Unspecified Neurodevelopmental Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Schizophrenia Spectrum and Other Psychotic Disorders Schizotypal Personality Disorder Delusional Disorder Brief Psychotic Disorder Schizophreniform Disorder Schizophrenia Schizoaffective Disorder Substance/Medication-Induced Psychotic Disorder Psychotic Disorder Due to Another Medical Condition Catatonia Associated With Another Mental Disorder (Catatonia Specifier) Catatonic Disorder Due to Another Medical Condition Unspecified Catatonia Other Specified Schizophrenia Spectrum and Other Psychotic Disorder Unspecified Schizophrenia Spectrum and Other Psychotic Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Bipolar and Related Disorders Bipolar I Disorder Bipolar II Disorder Cyclothymic Disorder Substance/Medication-Induced Bipolar and Related Disorder Bipolar and Related Disorder Due to Another Medical Condition Other Specified Bipolar and Related Disorder Unspecified Bipolar and Related Disorder Depressive Disorders Disruptive Mood Dysregulation Disorder Major Depressive Disorder, Single and Recurrent Episodes Persistent Depressive Disorder (Dysthymia) Premenstrual Dysphoric Disorder Substance/Medication-Induced Depressive Disorder Depressive Disorder Due to Another Medical Condition Other Specified Depressive Disorder Unspecified Depressive Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Anxiety Disorders Separation Anxiety Disorder Selective Mutism Specific Phobia Social Anxiety Disorder (Social Phobia) Panic Disorder Panic Attack Agoraphobia Generalized Anxiety Disorder Substance/Medication-Induced Anxiety Disorder Anxiety Disorder Due to Another Medical Condition Other Specified Anxiety Disorder Unspecified Anxiety Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Obsessive-Compulsive and Related Disorders Obsessive-Compulsive Disorder Body Dysmorphic Disorder Hoarding Disorder Trichotillomania (Hair-Pulling Disorder) Excoriation (Skin-Picking) Disorder Substance/Medication-Induced Obsessive-Compulsive and Related Disorder Obsessive-Compulsive and Related Disorder Due to Another Medical Condition Other Specified Obsessive-Compulsive and Related Disorder Unspecified Obsessive-Compulsive and Related Disorder Trauma- and Stressor-Related Disorders Reactive Attachment Disorder Disinhibited Social Engagement Disorder Posttraumatic Stress Disorder Acute Stress Disorder Adjustment Disorders Other Specified Trauma- and Stressor-Related Disorder Unspecified Trauma- and Stressor-Related Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Dissociative Disorders Dissociative Identity Disorder Dissociative Amnesia Depersonalization/Derealization Disorder Other Specified Dissociative Disorder Unspecified Dissociative Disorder Somatic Symptom and Related Disorders Somatic Symptom Disorder Illness Anxiety Disorder Conversion Disorder (Functional Neurological Symptom Disorder) Psychological Factors Affecting Other Medical Conditions Factitious Disorder Other Specified Somatic Symptom and Related Disorder Unspecified Somatic Symptom and Related Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Feeding and Eating Disorders Pica Rumination Disorder Avoidant/Restrictive Food Intake Disorder Anorexia Nervosa Bulimia Nervosa Binge Eating Disorder Other Specified Feeding and Eating Disorder Unspecified Feeding and Eating Disorder Elimination Disorders Enuresis Encopresis Other Specified Elimination Disorder Unspecified Elimination Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Sleep-Wake Disorders Insomnia Disorder Hypersomnolence Disorder Narcolepsy Breathing-Related Sleep Disorders Obstructive Sleep Apnea Hypopnea Syndrome Central Sleep Apnea Sleep-Related Hypoventilation Circadian Rhythm Sleep-Wake Disorders Parasomnias Non–Rapid Eye Movement Sleep Arousal Disorders Sleepwalking Sleep Terrors Nightmare Disorder Rapid Eye Movement Sleep Behavior Disorder Restless Legs Syndrome Substance/Medication-Induced Sleep Disorder Other Specified Insomnia Disorder Unspecified Insomnia Disorder Other Specified Hypersomnolence Disorder Unspecified Hypersomnolence Disorder Other Specified Sleep-Wake Disorder Unspecified Sleep-Wake Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Sexual Dysfunctions Delayed Ejaculation Erectile Disorder Female Orgasmic Disorder Female Sexual Interest/Arousal Disorder Genito-Pelvic Pain/Penetration Disorder Male Hypoactive Sexual Desire Disorder Premature (Early) Ejaculation Substance/Medication-Induced Sexual Dysfunction Other Specified Sexual Dysfunction Unspecified Sexual Dysfunction The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Gender Dysphoria Gender Dysphoria Other Specified Gender Dysphoria Unspecified Gender Dysphoria Disruptive, Impulse-Control, and Conduct Disorders Oppositional Defiant Disorder Intermittent Explosive Disorder Conduct Disorder Antisocial Personality Disorder Pyromania Kleptomania Other Specified Disruptive, Impulse-Control, and Conduct Disorder Unspecified Disruptive, Impulse-Control, and Conduct Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Substance-Related and Addictive Disorders Substance Use Disorders Substance-Induced Disorders Substance Intoxication Substance Withdrawal Substance/Medication-Induced Disorders Included Elsewhere in the Manual Same substances as DSM-IV, plus gambling The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Neurocognitive Disorders Delirium Other Specified Delirium Unspecified Delirium Major & Mild Neurocognitive Disorders Major or Mild Neurocognitive Disorder Due to Alzheimer’s Disease Major or Mild Frontotemporal Neurocognitive Disorder Major or Mild Neurocognitive Disorder with Lewy Bodies Major or Mild Vascular Neurocognitive Disorder Major or Mild Neurocognitive Disorder Due to Traumatic Brain Injury Substance/Medication-Induced Neurocognitive Disorder Major or Mild Neurocognitive Disorder Due to HIV Infection Major or Mild Neurocognitive Disorder Due to Prion Disease Major or Mild Neurocognitive Disorder Due to Parkinson’s Disease Major or Mild Neurocognitive Disorder Due to Huntington’s Disease Neurocognitive Disorder Due to Another Medical Condition Major or Mild Neurocognitive Disorder Due to Multiple Etiologies Unspecified Neurocognitive Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Personality Disorders Paranoid Personality Disorder Schizoid Personality Disorder Schizotypal Personality Disorder Antisocial Personality Disorder Borderline Personality Disorder Histrionic Personality Disorder Narcissistic Personality Disorder Avoidant Personality Disorder Dependent Personality Disorder Obsessive-Compulsive Personality Disorder Personality Change Due to Another Medical Condition Other Specified Personality Disorder Unspecified Personality Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Paraphilic Disorders Voyeuristic Disorder Exhibitionistic Disorder Frotteuristic Disorder Sexual Masochism Disorder Sexual Sadism Disorder Pedophilic Disorder Fetishistic Disorder Transvestic Disorder Other Specified Paraphilic Disorder Unspecified Paraphilic Disorder The Present: DSM-5 Section II: Essential Elements: Diagnostic Criteria and Codes Other Mental Disorders Other Specified Mental Disorder Due to Another Medical Condition Unspecified Mental Disorder Due to Another Medical Condition Other Specified Mental Disorder Unspecified Mental Disorder Medication-Induced Movement Disorders and Other Adverse Effects of Medication The Present: DSM-5 Section III: Emerging Measures and Models Assessment Measures Cultural Formulation Alternative DSM-5 Model for Personality Disorders Conditions for Further Study Attenuated Psychosis Syndrome Depressive Episodes With Short-Duration Hypomania Persistent Complex Bereavement Disorder Caffeine Use Disorder Internet Gaming Disorder Neurobehavioral Disorder Due to Prenatal Alcohol Exposure (NDPAE) Suicidal Behavior Disorder Nonsuicidal Self-Injury The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 Culture and demography Included diverse individuals on study groups and work groups Study group dedicated to reviewing all proposals for cultural issues Provide assessment tool for clinical formulation List culture-bound syndromes Description of cultural expressions of disorders The Present: DSM-5 Cultural Formulation Interview Based on DSM-IV model Updated as a specific measure (14 items), subjected to field trials Cultural identity of the individual Including acculturation for immigrants Cultural explanations of individual’s illness Idioms of distress Meaning of symptoms in cultural context Other cultural factors related to functioning Social stressors and supports Cultural aspects of treatment relationship Cultural assumptions about mental health care Status issues The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 Severity assessments Cross-cutting dimensions Mood Anxiety Social Dysfunction Self-Concept Sleep Attention Cognition Certain Disorders Autism Spectrum The Present: DSM-5 Changes in the DSM-5 The Number 5 Connection to Medicine and Biological Focus Connection with ICD Chapter reorganization Issues of culture, demography Dimensional severity assessments Criterion Sets The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 Autism Spectrum DSM-IV Autism: profound, early onset difficulties with social behavior, communication, and atypical behaviors Asperger’s: (later age of onset, absence of language delay) PDD: sub-threshold autism DSM-5 proposal Replace these categories with a single diagnosis, ASD Require all monothetic social communication criteria Meet polythetic criteria for restricted, repetitive behaviors The Present: DSM-5 Autism Spectrum: The case for change Evidentiary Argument Quantitative evidence suggests a spectrum rather than categorical distinctions, that social and communication symptoms cohere Age of onset and language delay relate quantitatively, not qualitatively, to this spectrum Clinical Argument Monothetic criteria will result in more qualitative homogeneity while also permitting more quantitative heterogeneity Moral Argument Collapsing categories will permit greater access to services for people who do not have DSM-IV Autism The Present: DSM-5 Autism Spectrum: Prevalence hysteria in DSM-IV Prevalence and access to services “59 percent of those who were ‘diagnosed not autistic’ in the 1980s would qualify as having autism today” (Miller et al., 2013) 1 out of 88 people have autism 1 in 34 South Korean people have autism The Present: DSM-5 Autism Spectrum: DSM-5 Prevalence McPartland et al., 2012 (also Mattila et al., 2011 from Finnish epidemiological sample) Of people with DSM-IV ASD (any of the three) from DSM-IV field trial, 61% meet for DSM-5 ASD Of people without DSM-IV Autistic Disorder, 95% also do not have DSM-5 ASD Social Communication Disorder as a solution? The Present: DSM-5 Autism Spectrum: Prevalence hysteria “The American Psychiatric Association voted this weekend to remove the diagnosis of Asperger’s syndrome from the so-called bible of psychiatry, the Diagnostic and Statistical Manual of Psychiatric Disorders. People with Asperger’s will now more likely be diagnosed as having autism spectrum disorder. The APA says the change will lead to more accurate diagnoses for people with autism — but critics say removing the diagnosis may result in fewer people getting the services and care they need.” Excerpt from NPR discussion, 2011 “DSM-5 under-identifies PDDNOS” (Mayes et al., 2013) The Present: DSM-5 Autism Spectrum: Prevalence hysteria “One child doesn't talk, rocks rhythmically back and forth and stares at clothes spinning in the dryer. Another has no trouble talking but is obsessed with trains, methodically naming every station in his state. Autistic kids like these hate change, but a big one is looming.” USA Today, 2012 “Proposed changes in the definition of autism would sharply reduce the skyrocketing rate at which the disorder is diagnosed and might make it harder for many people who would no longer meet the criteria to get health, educational and social services” NY Times, 2012 The Present: DSM-5 Autism Spectrum: Prevalence hysteria http://usatoday30.usatoday.com/news/health/story/ 2012-04-05/doctors-change-autismdefinition/54047994/1 1:08 1:35 The Present: DSM-5 Larger Point: Prevalence is important and arbitrary The problem of getting appropriate services is a real one, and it is reasonable to be concerned, even if the hyperbole isn’t necessary. But… How many tall people are there? How many short people are there? All the short people get $50 – are you short? The Present: DSM-5 Deeper issue Dimensions and Categories The Present: DSM-5 Validity of Dimensional Models (Markon, 2011) In 2 meta-analyses involving 58 studies and 59,575 participants, we quantitatively summarized the relative reliability and validity of continuous (i.e., dimensional) and discrete (i.e., categorical) measures of psychopathology. Overall, results suggest an expected 15% increase in reliability and 37% increase in validity through adoption of a continuous over discrete measure of psychopathology alone. This increase occurs across all types of samples and forms of psychopathology, with little evidence for exceptions. For typical observed effect sizes, the increase in validity is sufficient to almost halve sample sizes necessary to achieve standard power levels. With important caveats, the current results, considered with previous research, provide sufficient empirical and theoretical basis to assume a priori that continuous measurement of psychopathology is more reliable and valid. Use of continuous measures in psychopathology assessment has widespread theoretical and practical benefits in research and clinical settings. The Future: DSM-5.1 and beyond Clinical Utility of Dimensional Models (First, 2005) A potential obstacle to implementing dimensional representations in the Diagnostic and Statistical Manual of Mental Disorders (DSM) is lack of data about clinical utility and user acceptability. Adopting a dimensional approach would likely complicate medical record keeping, create administrative and clinical barriers between mental disorders and medical conditions, require a massive retreating effort, disrupt research efforts (e.g., meta-analyses), and complicate clinicians’ efforts to integrate prior clinical research using DSM categories into clinical practice. Efforts to empirically demonstrate the clinical utility of dimensional alternatives should be a prerequisite for their future implementation in order to establish that their advantages outweigh the disadvantages. Approaches to promote user acceptability and the development of an empirical database include dimensionalizing existing DSM categories and including research dimensions in the DSM appendix. The Future: DSM-5.1 and beyond How do you think about patients? The Future: DSM-5.1 and beyond Challenge Clinical decisions are usually categorical It is possible that it is more natural to think about types of people rather than patterns of variables Nature seems to be dimensional Do we learn to think differently and tolerate arbitrary cuts, or do we force nature to accommodate our cognitive style and clinical needs? The Future: DSM-5.1 and beyond Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 ADHD Now a ‘Neurodevelopmental Disorder’ Oppositional and Conduct disorders now in “Disruptive, Impulse Control, and Conduct Disorders” Relax age-of-onset criterion Replace subtypes with specifiers Adults Age-appropriate criteria Expanded impulsivity criteria Lowered diagnostic thresholds for adults Permit dual diagnosis with autism The Present: DSM-5 ADHD: Age of onset For It can be difficult to recall age of onset – only 50% of adults with ADHD symptoms above diagnostic cut recalled onset prior to 7, whereas 95% recalled symptoms prior to age 16 This criterion was based on clinical lore in the first place One study suggested that using a cutoff of age 12 would not affect prevalence (Kessler et al., 2005) Against Relaxing any criterion will inevitably increase prevalence Questions about motives given the most common treatment for ADHD is pharmaceutical Does not fit with commonly accepted theoretical models of ADHD The Present: DSM-5 ADHD: Specifiers For Several studies have shown that inattentive and hyperactive/impulsive dimensions are correlated, and can be represented as a bifactor model ADHD severity Hyperactive/impulsive style Inattentive style Against Clinicians are more accustomed to typological approach Specifiers are, in essence, still a typological approach The Present: DSM-5 ADHD: Age-appropriate criteria For Provides for a more accurate diagnosis for adults (which would include increasing sensitivity and thus prevalence) Has been hard to know if decline in rates is due to actual declines (as is clinical lore) or insensitivity of childhood symptoms to portray adult problems (e.g., examples of things that might be lost include toys, school assignments, pencils, and books) Against Giving more behavioral examples and lowering diagnostic thresholds likely to increase prevalence Increasing impulsivity content may worsen diagnostic overlap The Present: DSM-5 ADHD: Autism For No reason a person could not have both autism and ADHD Against Increase in prevalence in ADHD The Present: DSM-5 Larger Point: Diagnostic breadth Diagnostic Dilemma Include everyone with similar features Distinguish everyone with different features Lumping – Diagnostic heterogeneity Splitting – Comorbidity Is the hierarchical approach a solution? The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 PTSD Listed in "trauma and stressor-related disorders" DSM-IV: 3 clusters re-experiencing avoidance arousal DSM-5: 4 clusters intrusion symptoms avoidance symptoms arousal/reactivity symptoms negative mood and cognitions Criterion A2 (requiring fear, helplessness or horror immediately after the trauma) will be removed The Present: DSM-5 PTSD: the case for change PTSD is unique etiologically and splits off from anxiety disorders in structural research More consistent with empirical research on the structure of symptoms (Anthony et al., 1999) Evidence not consistent with the importance of immediate stress upon exposure to traumatic event (Karam et al., WHO study, 2010) Prevalence is not affected (Nat Center for PTSD, 2012) The Present: DSM-5 PTSD: the case against change To the extent that the disorder is not about the effects of trauma (i.e., acute stress reaction), the basis of the disorder is lost (McNally, 2011) Adding mood symptoms will increase overlap with other mood, anxiety, and personality disorders, despite moving the disorder to its own chapter The Present: DSM-5 Larger Point: Change is difficult Is change worth it? Patients are re-classified Will affect access to services, forensic issues, billing procedures, organization of interventions National Center for PTSD is re-norming CAPS, PCL Will services really improve? Another perspective: the manual constrains clinical care Do we need the manual to provide effective services once ‘caseness’ is determined? What if there were another way to determine ‘caseness’ (clinician judgment of dysfunction)? Need to maintain consistent prevalence The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 Depression and Grief DSM-IV grief criterion “The symptoms are not better accounted for by Bereavement, i.e., after the loss of a loved one, the symptoms persist for longer than 2 months or are characterized by marked functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychotic symptoms, or psychomotor retardation.” (p. 356) The Present: DSM-5 Depression and Grief: The case for change Research support for dropping exclusion Only 20% of bereaving people meet criteria for depression (Brent et al., 1994; 2009) Depression in the context of loss has a course (Kendler et al., 2008) , correlates (Zisook & Kendler, 2007), and treatment response (Zisook et al., 2001) similar to depression without loss Moral argument for dropping exclusion Leaving depression untreated because a person is grieving is unethical (Shear et al., 2011) Bereavement increases suicide risk (Ajdacic-Gross et al., 2008) The Present: DSM-5 Depression and Grief: The case against change Research support against dropping exclusion Research review was based on genuine MDD cases with and without bereavement no cases with bereavement without MDD, or in mixed cases, these were not distinguished “The challenge is to distinguish those bereavement-related depressions that are likely intense normal grief from those that have turned into pathological depressions” (Wakefield & First, 2011) Bereavement-excluded depression does not increase risk for future depressive episodes, whereas DSM-IV depression (with or without bereavement) does (Mojtabai, 2011) Moral argument for dropping exclusion Cases excluded in DSM-IV by definition lack suicidal ideation Pathologizing normal reactions The Present: DSM-5 Larger Point: Harmful Dysfunction (Wakefield, 1992) Harm Some kind of problem in living e.g., Difficulty getting out of bed, difficulty concentrating Dysfunction Some kind of systemic failure e.g., Hypothyroidism The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 Disruptive Mood Dysregulation Disorder Severe nonepisodic emotional and behavioral problems involving irritability New diagnostic category for children and adolescents: Severe temper outbursts Negative mood between outbursts Present for 12 months or more in multiple settings Onset before age 10 Child must be at least 6 for the diagnosis The Present: DSM-5 Disruptive Mood Dysregulation Disorder Copeland et al (2013) Prevalence: .8% to 3.3%, declines with age Co-occurrence: “62-92% of the time across ages DMDD is given with another diagnosis” Depression Oppositional Defiant Disorder Significant predictor of dysfunction The Present: DSM-5 Controversies Diagnostic splitting Role of drug companies (viz., grief criterion for depression) Lack of consensual definition and validity data The Present: DSM-5 Larger Point: The role of development Precursor to unipolar depression to a greater degree than bipolar depression (Stingaris et al., 2009) Is this an early manifestation of depression? Assess the current presentation Assess the underlying syndrome Is the focus on current presentation consistent with the medical model? The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 Substance Dependence and Abuse Drop distinction between Dependence and Abuse, to have one single Substance Use Disorder category The Present: DSM-5 Dependence and Addiction “The term dependence is misleading, because people confuse it with addiction, when in fact the tolerance and withdrawal patients experience are very normal responses to prescribed medications that affect the central nervous system,” said Charles O’Brien, M.D., Ph.D., chair of the APA’s DSM Substance-Related Disorders Work Group. “On the other hand, addiction is compulsive drug- seeking behavior which is quite different. We hope that this new classification will help end this wide-spread misunderstanding.” -Recovery Today, 2010 The Present: DSM-5 Substance Dependence and Abuse (The Scientist, 2012) Allen Frances, chair of the DSM-IV Task Force (blog): “The further watering down of definitional standards will make psychiatric diagnosis so ubiquitous as to be almost meaningless—and divert scarce resources away from those who do need them.” Marc Schuckit, member of the Substance Use Disorder Work Group for the DSM-5 : "Our goal was to try to make the criteria easier for the usual clinician to use, and so we're no longer asking them to remember one criteria set for abuse and a separate set for dependence.” The Present: DSM-5 Larger Point: Whose Clinical Utility? Schuckit: easier for clinicians Frances: focus clinician attention on most severe These are not evidentiary issues with respect to the nature of pathology, they are evidentiary issues with respect to the nature of practice…so what is the point of the manual, exactly? Carve nature at its joints Provide a vehicle for efficient classification Triage people to appropriate services Box (1987): “all models are wrong, but some are useful” The Present: DSM-5 Changes to Disorder Criteria Autism spectrum ADHD PTSD Depression Disruptive Mood Dysregulation Disorder Substance Use Disorders Psychotic Disorders Eating Disorders The Present: DSM-5 Other changes Psychotic Disorders Add schizotypal personality disorder Drop schizophrenia subtypes in favor of dimensional ratings of positive and negative symptoms Eating disorders Drop amenorrhea requirement for Anorexia Lower frequency of bingeing Add Binge Eating Disorder The Present: DSM-5 DSM-5 Committee Exercise Pick leaders with expertise for each topic Dropping multi-axial format Addressing issues of culture Autism spectrum ADHD PTSD Depression grief criterion Disruptive Mood Dysregulation Disorder Substance abuse/dependence Dimensionalizing schizophrenia spectra Adding Binge Eating Disorder Assemble groups Discuss advantages and disadvantages of changing the diagnosis Come to a final decision to present to the group The Present: DSM-5 DSM-5 Committee Exercise How much did the proposals change the DSM-IV? Dropping multi-axial format Addressing issues of culture Autism spectrum ADHD PTSD Depression grief criterion Disruptive Mood Dysregulation Disorder Substance abuse/dependence Dimensionalizing schizophrenia spectra Adding Binge Eating Disorder How much variability of opinion was there within groups? How were differences resolved? Is this the right way to develop a manual? The Present: DSM-5 Outline The Past: Competing models of psychopathology The Present: Specific changes in the DSM-5 The Edge: DSM-5 personality disorders The Future: DSM-5.1 and beyond The Edge: DSM-5 Personality Disorders What are Personality Disorders? Patients and Families: Chronic and severe Insurance Companies: Untreatable NIMH: Insufficiently biological Clinicians: Annoyance Psychoanalysts: Fundamental context Descriptive Psychiatrists: Questionable categories Quantitative Psychologists: The vanguard of psychopathology (Krueger, in press) The Edge: DSM-5 Personality Disorders DSM-IV (and DSM-5…) Cluster A Cluster B Cluster C Appendix Paranoid Borderline Avoidant PassiveAggressive Dependent Sadistic ObsessiveCompulsive Depressive Antisocial Schizoid Histrionic Schizotypal Narcissistic The Edge: DSM-5 Personality Disorders Problems with DSM-IV Structure (Fossati et al., 2000) Dimensionality (Widiger & Clark, 2000) Diagnostic overlap (Lenzenweger et al., 2007) Link to normal personality (Widiger & Trull, 2009) Diagnostic Heterogeneity (Widiger & Trull, 2009) Problems with particular diagnoses Antisocial PD vs. Psychopathy (Hare, 1991) Grandiose and Vulnerable Narcissism (Pincus et al., 2009) Many PDs understudied (Widiger & Trull, 2009) No specific treatments (Widiger & Trull, 2009) The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders What does “Dimensional” mean? No qualitative distinction between normal and abnormal How do you determine caseness? Using severity ratings within diagnostic categories? Doesn’t solve the co-occurrence problem, but provides more valid data Variable centered constructs Hybrid system in which categories are constellations of dimensions The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders Trait Models Markon, K.E., Krueger, R.F., & Watson, D. (2005). Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology, 88, 139-157. The Edge: DSM-5 Personality Disorders Trait Models Integrate competing theories of normative personality (Widiger & Simonsen, 2005; Wright et al., in review) Link to biological structures and processes (DeYoung et al., 2010) Integrate normal personality, abnormal personality, and psychopathology (Markon et al., 2005) Well-defined heritability profile and course (Hopwood et al., 2010) The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders Personality and Psychopathology There is nothing special about the relationship between personality traits and personality disorders The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Trait Specificity N E O A C PDs 0.31 -0.14 0.02 -0.18 -0.13 Axis I 0.39 -0.24 -0.09 -0.02 -0.30 The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Specificity (Ruiz et al., 2008) The Edge: DSM-5 Personality Disorders Personality and Psychopathology So how are personality traits and personality disorders different? The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Distributions (CLPS) The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Stability (Hopwood et al., in press) (Morey et al., 2007) Figure 1. Mean 10-year rank-order stability values for personality traits and disorders. The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Incremental Validity (Morey et al., 2007) Disorders increment normal traits Hybrid model performs best Normal traits increment disorders The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Trait Predictions (Hopwood et al., 2007) The Edge: DSM-5 Personality Disorders Normative vs. Pathological Personality: Clinical Utility Personality Trait Personality Problem Valueless Problematic Stable Malleable Decontextualized Occur in Social Contexts No Treatments Treatments The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders Exercise You are on the DSM-5 committee and have been mandated to trim the number of PDs down to 6 or less. What do you cut? Schizotypal Schizoid Paranoid Antisocial Borderline Narcissistic Histrionic Dependent Avoidant Obsessive-Compulsive The Edge: DSM-5 Personality Disorders Exercise How similar is your list to the DSM-5 proposal? Antisocial Avoidant Borderline Narcissistic Obsessive-Compulsive Schizotypal On the strategy of trimming disorders… The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders Severity and Style (Hopwood et al., 2011) GAF Social Dysfunction Work Dysfunction Leisure Dysfunction C P C P C P C P -.56* -.44* .52* .50* .33* .38* .49* .41* Peculiarity -.14* -.23* .25* .20* .03 .14 .13* .21* Withdrawal -.09 -.05 .12* .08 .02 .07 .13* .14* Fearfulness -.01 .02 .06 -.04 .10 -.10 .16* .03 Instability -.17* -.05 .04 .01 .09 .05 .01 -.01 Deliberateness .12* .09 -.10 -.07 -.07 -.11 -.07 -.06 ΔR2 .07* .07* .09* .05* .02 .05 .07* .07* Overall R2 .38* .26* .35* .30* .14* .17* .30* .24* Step 1 Severity Step 2 C = concurrent, P = 3-year prospective The Edge: DSM-5 Personality Disorders Proposed Solutions Dimensionalize Link to established basic models of personality Distinguish symptoms from traits Trim list of disorders Distinguish general from PD-specific symptoms Determine optimal way of characterizing PD symptoms The Edge: DSM-5 Personality Disorders Continuous or Prototype Diagnoses Symptom counts More reliable than categories (Heumann & Morey, 1990) More valid than categories (Morey et al., 2007) Prototypes DSM-I and II SWAP (Westen & Shedler, 2000) The Edge: DSM-5 Personality Disorders Continuous or Prototype Diagnoses Samuel et al. in press 320 patients rated by treating clinicians using a prototype form and structured diagnostic interview by research interviewers for AVPD, BPD, OCPD, STPD Diagnostic interview incremented prototype for indicating patient functioning in every case Prototype rating never incremented interview Results replicated for self-report of PD vs. prototype On the strategy of proposing prototypes… The Edge: DSM-5 Personality Disorders DSM-5 Work Group Proposal Level: Self and Interpersonal dysfunction Types: 6 PD types defined by trait constellations Traits: 5 higher order and 25 lower order traits The Edge: DSM-5 Personality Disorders Level Self: Identity: Experience of oneself as unique, with clear boundaries between self and others; stability of self-esteem and accuracy of self-appraisal; capacity for, and ability to regulate, a range of emotional experience Self-direction: Pursuit of coherent and meaningful short-term and life goals; utilization of constructive and prosocial internal standards of behavior; ability to self-reflect productively Interpersonal: Empathy: Comprehension and appreciation of others’ experiences and motivations; tolerance of differing perspectives; understanding of the effects of own behavior on others Intimacy: Depth and duration of positive connections with others; desire and capacity for closeness; mutuality of regard reflected in interpersonal behavior The Edge: DSM-5 Personality Disorders Level Ratings 0-4 (4 is worst), field studies to determine cutoff Empathy = 0 Capable of accurately understanding others’ experiences and motivations in most situations. Comprehends and appreciates others’ perspectives, even if disagreeing. Is aware of the effect of own actions on others. Empathy = 4 Pronounced inability to consider and understand others’ experience and motivation. Attention to others' perspectives virtually absent (attention is hypervigilant, focused on need-fulfillment and harm avoidance). Social interactions can be confusing and disorienting. The Edge: DSM-5 Personality Disorders Types 6 types Based on trait criteria (all traits must be met) Antisocial Avoidant Borderline Narcissistic Obsessive-Compulsive Schizotypal The Edge: DSM-5 Personality Disorders Traits 5 domains based on PSY-5, Big 5 models 25 lower order traits linked to specific PDs 0-3 scale (3 is worst) Can be used to assess individuals without PD with PD who don’t fit into type (PDTS) in addition to type The Edge: DSM-5 Personality Disorders Traits-Disorder Crosswalk Schizotypal All three psychoticism traits Suspisciousness, Withdrawal, Restricted Affectivity Antisocial Hostility, Manipulativeness, Deceitfulness, Callousness, Irresponsibility, Impulsivity, Risk Taking Borderline Separation Insecurity, Anxiousness, Emotional Lability, Depressivity, Impulsivity, Risk Taking The Edge: DSM-5 Personality Disorders Traits-Disorder Crosswalk Narcissistic Attention Seeking, Grandiosity Avoidant Anxiousness, Withdrawal, Intimacy Avoidance, Anhedonia Obsessive Compulsive Perseveration, Rigid Perfectionism The Edge: DSM-5 Personality Disorders NA DET ANT DIS PSY Submissiveness Restricted Affectivity Separation Insecurity Anxiousness Emotional Lability Hostility Perseveration Suspiciousness Depressivity Withdrawal Intimacy Avoidance Anhedonia Manipulativeness Deceitfulness Callousness Attention Seeking Grandiosity Irresponsibility Impulsivity Distractibility Rigid Perfectionism Risk Taking Eccentricity Perceptual Dysregulation Unusual Beliefs and Experiences Hopwood et al., 2012 STPD .15 .31 .28 .39 .42 .38 .51 .51 .51 .51 .31 .46 .29 .39 .39 .18 .31 .41 .26 .39 .37 .10 .61 .61 .64 ASPD .04 .26 .18 .17 .22 .40 .35 .37 .38 .23 .29 .28 .43 .55 .54 .30 .28 .49 .56 .40 .11 .53 .38 .44 .37 BPD .20 .17 .45 .53 .56 .53 .54 .46 .61 .35 .26 .49 .29 .40 .37 .24 .20 .44 .39 .47 .32 .18 .46 .55 .41 NPD .11 .25 .31 .31 .32 .48 .41 .44 .31 .28 .24 .25 .49 .51 .47 .51 .54 .36 .30 .32 .36 .16 .39 .43 .38 AVPD .38 .24 .40 .51 .41 .38 .48 .38 .51 .48 .24 .50 .12 .28 .20 .10 .12 .27 .10 .39 .28 -.16 .36 .36 .21 OCPD .26 .23 .28 .42 .35 .32 .46 .27 .27 .28 .18 .22 .23 .19 .15 .18 .25 .15 .11 .30 .54 -.07 .34 .35 .31 The Edge: DSM-5 Personality Disorders The challenge Coverage, construct consistency more overlap, diagnostic heterogeneity Discriminant validity limited coverage, consistency with past definitions Solution: Divorce PD symptoms and traits The Edge: DSM-5 Personality Disorders DSM-5 Proposal 1. Is impairment in personality functioning (self and interpersonal) present or not? 2. If so, rate the level of impairment in self (identity or self-direction) and interpersonal (empathy or intimacy) functioning on the Levels of Personality Functioning Scale. 3. Is one of the 6 defined types present? 4. If so, record the type and the severity of impairment. 5. If not, is PD-Trait Specified present? 6. If so, record PDTS, identify and list the trait domain(s) that are applicable, and record the severity of impairment. 7. If a PD is present and a detailed personality profile is desired and would be helpful in the case conceptualization, evaluate the trait facets. 8. If neither a specific PD type nor PDTS is present, evaluate the trait domains and/or the trait facets, if these are relevant and helpful in the case conceptualization. The Edge: DSM-5 Personality Disorders Jennifer Case Example 28 year old woman History of abuse by father and romantic partners Close to mother and several women but chronic difficulties in romantic relationships with men PTSD from witnessing death of child 3 years prior Long history of self-harming behavior including promiscuous sex, alcohol and drug abuse increased with trauma Recently sought treatment after being fired for missing work (6 months), moving to shelter (2 weeks), shoplifting for food and alcohol (2 weeks), cutting (2x in 1 week) The Edge: DSM-5 Personality Disorders Jennifer’s DSM-IV diagnosis Borderline PD (7) + unstable relationships, identity disturbance, impulsivity, suicidal behavior, affective instability, emptiness, inappropriate anger - efforts to avoid abandonment, stress related paranoia Histrionic PD (5) + inappropriate sexual behavior, rapidly shifting and shallow emotions, use of physical appearance for attention, theatricality, suggestibility - uncomfortable unless center of attention, impressionistic speech, considers relationships to be closer than they are Antisocial PD (3 + Conduct Disorder) + childhood conduct disorder, failure to conform, deceitfulness, impulsivity, recklessness, irresponsibility - lack of remorse and aggressiveness The Edge: DSM-5 Personality Disorders Jennifer’s Level of Functioning Self Identity = 4 Self-direction = 3 Interpersonal Empathy = 2 Intimacy = 4 The Edge: DSM-5 Personality Disorders Jennifer’s Diagnosis (PDTS) Jennifer’s Traits Negative Emotionality Submissiveness Restricted Affectivity Separation Insecurity Anxiousness Emotional Lability Hostility Perseveration Detachment Suspiciousness Depressivity Withdrawal Intimacy Avoidance Anhedonia 1 0 2 3 3 1 0 2 2 1 1 1 Antagonism Manipulativeness Deceitfulness Callousness Attention-Seeking Grandiosity Disinhibition Irresponsibility Impulsivity Distractibility Rigid Perfectionism Risk Taking Psychoticism Eccentricity Cognitive Dysregulation Unusual Beliefs/Experiences 1 1 0 2 0 3 3 2 0 3 0 2 0 Borderline Traits in Red The Edge: DSM-5 Personality Disorders Jennifer’s DSM-5 Summary Diagnosis PD Trait Specified with Deficits in Identity and Intimacy and the following significant traits: Anxiousness Emotional Lability Irresponsibility Impulsivity Risk Taking The Edge: DSM-5 Personality Disorders Exercise Which diagnosis describes the patient more accurately? best suggests treatment strategies? is most efficient? do you prefer overall? The Edge: DSM-5 Personality Disorders DSM-5.0 Task Force recommended Work Group proposal Board of Trustees voted to retain DSM-IV model The Work Group proposal will be printed verbatim in Section III The Edge: DSM-5 Personality Disorders The traits are in What does this decision mean for the short-term? Alternative PD diagnoses? Clinical use of trait model What does this decision mean for the long-term? The first step towards a reconceptualization? The Edge: DSM-5 Personality Disorders Momentum RDoC Unified Treatments Comorbidity problems and the increasing acceptance of dimensionality has positioned quantitative psychology as a guidepost The Edge: DSM-5 Personality Disorders Outline The Past: Competing models of psychopathology The Present: Specific changes in the DSM-5 The Edge: DSM-5 personality disorders The Future: DSM-5.1 and beyond The Future: DSM-5.1 and beyond What is the point? Patient welfare (Box’s models) Diagnostic validity Diagnostic and treatment efficiency Trainability Parsimony Link between assessment and treatment How do we get there? Modesty and openness Maturity Integration of competing models Integration of science and practice The Future: DSM-5.1 and beyond Two Goals Validity Clinical Utility Is there a tension between these goals? Validity is a prerequisite for clinical utility, and dimensional models are more valid than categorical ones (Krueger & Markon, 2010) Clinical utility is the first priority, and the issues with dimensional models are too great to adopt them at this time (First, 2005) The Future: DSM-5.1 and beyond Theoretical Models of Psychopathology Descriptive Psychiatry Quantitative Psychology Psychoanalysis Learning Theory The Past: Competing Models of Psychopathology Psychoanalysis The Past: Competing Models of Psychopathology Assumptions of Psychoanalysis Psychopathology reflects compromise formations between desires and social acceptability Disorders blend together dynamically, with a basic distinction between between neurotic, character, and psychotic illness based on psychosocial maturation Effective taxonomy needs to take the complexity of patient presentation across levels of analysis into account The Past: Competing Models of Psychopathology Freud Research in neurology, neuropathology, anesthesia The Past: Competing Models of Psychopathology Freud’s research accomplishments prior to psychoanalysis (Galbis-Reig, 2004) Freud first studied the phylogenetic association between the central nervous system of lower vertebrates and humans. Using Crayfish, Freud demonstrated that nerve fibers emerge from a web-like substance in the neurons and that the structure is always fibrillary. Freud introduced the use of gold chloride to stain nerve tissues. Freud studied the structure and function of the medulla oblongata and the connection between the posterior columns of the spinal cord, the acoustic nerve, and the cerebellum. Freud wrote the first analytical and scientific summary of research on cocaine and was the first investigator to predict its potential use as a local anesthetic. Freud wrote four major texts on neurological disorders from 1891-1893 and was an international expert in aphasia and paralysis. The Past: Competing Models of Psychopathology Freud Research in neurology, neuropathology, anesthesia Applied Neurology Hypnosis, catharsis: Unconscious Fundamental tension between drives and socialization plays out in relation to society, and takes different forms over time Psychoanalysis: Personality theory Clinical Technique The Past: Competing Models of Psychopathology Diaspora Complexity and freshness of the topic Historical forces such as anti-semitism and feminism Core values (and the need to make bets) Diaspora Complexity and freshness of the topic Model Value Historical forces such as anti-semitism and feminism Id: Freud Neurology Ego: values A. Freud,(and Rappaport, Adaptation Core the need to make bets) Reich, Shapiro Interpersonal: Horney, Fromm, Sullivan, Blatt Justice and empiricism Object Relations: Klein, Mahler, Winnicot, Bion Mother-infant relationship Self: Kohut Experience Contributions of psychoanalysis Major principles have evidentiary merit (Westen, 1998) Unconscious (Underwood, 1996) Developmental factors (Sroufe, 2005) Social behavior regulates affect (Sadikaj et al., 2010) Importance of motives (Karoly, 1999) Psychotherapy is effective (Shedler, 1010) Focus on dynamics Influences across different spans of times Non-linear associations Conflicts between systems The Past: Competing Models of Psychopathology Limitations of psychoanalysis Metapsychology With respect to window-makers, to look at a window as if it is the point is to misunderstand the purpose of a window Insularity Dissemination Antagonism towards contemporary research methods “Failure to lead” Disinterest in integration is ironic given that it is the most comprehensive model When opportunities arose the analytic community bristled Politically unpopular, out of fashion However, some exciting stuff is happening in psychology (e.g., process dissociation, TMT) The Past: Competing Models of Psychopathology What might psychoanalysis contribute to nosology? Structure Self-Other-Affect Implicit-Explicit Autonomy-Sociotropy Dynamics Impulse-Defense Thematic recurrence Plasticity of drives Treatment Rich clinical description of phenotypes Use of relationship Focus on affect and thematic connections Theoretical Models of Psychopathology Descriptive Psychiatry Quantitative Psychology Psychoanalysis Learning Theory The Past: Competing Models of Psychopathology Learning Theory The Past: Competing Models of Psychopathology Assumptions of Learning Theory Observable behavior is the most trustworthy and therefore most important behavior Psychopathology requires inference and should be approached skeptically Most dysfunctional behavior is a function of learning history and triggering contextual factors Assessment requires understanding the function of behaviors, which vary from case to case The Past: Competing Models of Psychopathology Watson 1879-1958 The “behaviorist manifesto” Offered an inductive, basic science alternative to understanding behavior rooted in British Associationism The Past: Competing Models of Psychopathology Skinner 1904-1990 Focused on instrumental learning and contingent factors in behavior Together with classical conditioning, provided a coherent model for understanding the influence of proximal context The Past: Competing Models of Psychopathology Social and Cognitive Models Spence and others: fleshed out schedules of reinforcment, discrimination learning, etc. Bandura and others: added notion of social learning and modeling Tolman and others: added notion of cognition, which paved the way for cognitive revolution The Past: Competing Models of Psychopathology “CBT” Effort to be more practical and better connected to contemporary science Notion of using thoughts to affect change in emotions and behavior Teach a scientific mode of information processing Use what works The Past: Competing Models of Psychopathology Where did “CBT” come from? Learning Logical extension of Watson’s efforts to understand behavior using basic science Contemporary with cognitive revolution Ego Psychology Logical Extension of Freudian emphasis on drives and drive reduction Emphasis on cognition and notion of cooling down affect toward insight (making unconscious conscious) The Past: Competing Models of Psychopathology The Faustian bargain between CBT and the Medical Model Did you ever wonder why CBT cornered the market on manuals and RCTs? Organizing treatment around latent disorder constructs? Packaged treatments rather than functional interventions? “Evidence-based” as a reason not to need evidence? Was this strategic? Treatment-Patient matching research has mostly failed The Past: Competing Models of Psychopathology Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes Two parallel but independent randomized clinical trials were conducted, one with alcohol dependent clients receiving outpatient therapy (N = 952; 72% male) and one with clients receiving aftercare therapy following inpatient or day hospital treatment (N = 774; 80% male). Clients were randomly assigned to one of three 12-week, manual-guided, individually delivered treatments: Cognitive Behavioral Coping Skills Therapy, Motivational Enhancement Therapy or Twelve-Step Facilitation Therapy. Clients were then monitored over a 1-year posttreatment period. Clients attended on average two-thirds of treatment sessions offered, indicating that substantial amounts of treatment were delivered, and research follow-up rates exceeded 90% of living subjects interviewed at the 1-year posttreatment assessment. Significant and sustained improvements in drinking outcomes were achieved from baseline to 1-year posttreatment by the clients assigned to each of these well-defined and individually delivered psychosocial treatments. There was little difference in outcomes by type of treatment. Only one attribute, psychiatric severity, demonstrated a significant attribute by treatment interaction: In the outpatient study, clients low in psychiatric severity had more abstinent days after 12-step facilitation treatment than after cognitive behavioral therapy. Neither treatment was clearly superior for clients with higher levels of psychiatric severity. The findings suggest that psychiatric severity should be considered when assigning clients to outpatient therapies. The lack of other robust matching effects suggests that, aside from psychiatric severity, providers need not take these client characteristics into account when triaging clients to one or the other of these three individually delivered treatment approaches, despite their different treatment philosophies. (Journal of Studies on Alcohol, 1997 Jan;58(1):7-29.) The Past: Competing Models of Psychopathology The Faustian bargain between CBT and the Medical Model Did you ever wonder why CBT cornered the market on manuals and RCTs? Organizing treatment around latent disorder constructs? Packaged treatments rather than functional interventions? “Evidence-based” as a reason not to need evidence? Was this strategic? Treatment-Patient matching research has mostly failed CBT and other treatments tend to tie metaanalytically The Past: Competing Models of Psychopathology Psychotherapy for Depression in Adults Although the subject has been debated and examined for more than 3 decades, it is still not clear whether all psychotherapies are equally efficacious. The authors conducted 7 meta-analyses (with a total of 53 studies) in which 7 major types of psychological treatment for mild to moderate adult depression (cognitive– behavior therapy, nondirective supportive treatment, behavioral activation treatment, psychodynamic treatment, problem-solving therapy, interpersonal psychotherapy, and social skills training) were directly compared with other psychological treatments. Each major type of treatment had been examined in at least 5 randomized comparative trials. There was no indication that 1 of the treatments was more or less efficacious, with the exception of interpersonal psychotherapy (which was somewhat more efficacious; d = 0.20) and nondirective supportive treatment (which was somewhat less efficacious than the other treatments; d = 0.13). The drop-out rate was significantly higher in cognitive– behavior therapy than in the other therapies, whereas it was significantly lower in problem-solving therapy. This study suggests that there are no large differences in efficacy between the major psychotherapies for mild to moderate depression. (Cuipers et al., Journal of Consulting and Clinical Psychology 2008; 76:909 –922) The Past: Competing Models of Psychopathology The Faustian bargain between CBT and the Medical Model Did you ever wonder why CBT cornered the market on manuals and RCTs? Organizing treatment around latent disorder constructs? Packaged treatments rather than functional interventions? “Evidence-based” as a reason not to need evidence? Was this strategic? Treatment-Patient matching research has mostly failed CBT and other treatments tend to tie meta-analytically Contemporary “CBT” is becoming unified The Past: Competing Models of Psychopathology Strengths of Learning and CBT perspectives Values straightforward, parsimonious explanations Intended to be efficient Notion of stepped care built in to treatment Flexible and responsive to evidence Focuses on functions Why did this person become depressed here and not there? What interventions seem to be helping, and to what degree? The Past: Competing Models of Psychopathology Limitations of “CBT” Focus on diagnosis and symptoms Essential functionalism was lost (temporarily?) The virtue of behaviorism is its focus on why a person is doing what they are doing This is lost when the explanation becomes a latent disorder construct Assessment is over-simplified as checklists Who is carrying the flag for functional assessment? ABA Haynes’ Clinical Case Modeling The Past: Competing Models of Psychopathology Clinical Case Modeling (Haynes et al., 1997) Back to the Future: A Different Strategy? The Future: DSM-5.1 and beyond A Different Strategy Respect all of the major nosological traditions toward a transtheoretical model that maximizes the clinical utility and evidentiary links of clinical formulation Next: A thought experiment/demonstration of how this could happen The Future: DSM-5.1 and beyond Step 1: Structure Trait models provide the broad architecture for individual differences in personality and psychopathology Five-factor level of traits provides a parsimonious entry point for classification N E A O (P) C The Future: DSM-5.1 and beyond Traits as Psychological Systems: A medical model analogy The Future: DSM-5.1 and beyond Step 2: Clinical Focus Psychoanalysis, with its focus on the mapping of problems in living to clinical encounter, provides experience-near clinical focus At the broadest level, various schools agree (Kernberg, 1984) Patient’s Mind Self Other Affect The Future: DSM-5.1 and beyond Step 3: Integration via Systems N Affect E A O C Self Other The Future: DSM-5.1 and beyond Step 3: Systems as the bridge N Affect E A O Self C Other The Future: DSM-5.1 and beyond How did Extraversion get split? E facets on NEO-PI-R (Costa & McCrae, 1992) Interpersonal Gregariousness Warmth Assertiveness Affective Activity Excitement-Seeking Positive Affectivity The Future: DSM-5.1 and beyond Experimental Evidence (Morrone-Stupinsky & Lane, 2007) Extraversion is comprised of agentic and affiliative components, which are characterized by distinct positive emotional states of positive activation and warmth-affection, respectively. This study examined these positive emotions using the International Affective Picture System, a standardized set of pictures used to induce emotion. Compared to response to neutral pictures, the following target emotions were induced: (1) affiliative pictures induced warmth-affection and pleasantness, (2) agentic pictures induced positive activation, pleasantness, and arousal, (3) high arousal nonagentic pictures induced pleasantness and arousal, and (4) low arousal nonaffiliative pictures induced pleasantness. Agentic picture-induced positive affective ratings were significantly related to a trait measure of social potency, but not to other extraversion scales. The results support a multicomponent conceptualization of the extraversion trait, where agentic and affiliative components are associated with distinctive positive emotional experience. The Future: DSM-5.1 and beyond What about O and C? (Saucier, 1992) The Future: DSM-5.1 and beyond What about O and C? Issues like impulse control and thought disorder are important Interstitiality Some aspects are wrapped into Agency and Communion (depends on where you cut the hierarchy) Achievement Sensation-seeking Openness to new relationships Concern for others It would be practically useful to assess cognitive features in addition to the integrative model The Future: DSM-5.1 and beyond Systems as the bridge N Affect E Self A Other The Future: DSM-5.1 and beyond The interpersonal system The Future: DSM-5.1 and beyond The Interpersonal System: Agency and Communion Agency Communion Interpersonal Behavior Interpersonal Dominance Interpersonal Warmth Trait Achievementorientation (C), Gregariousness (E), Stimulus-Seeking (O) Sociability (E), Agreeableness (A), Fitting in (C), Socialization (N), Tolerance (O) Regulation Esteem Anxiety Functioning Work Love Gender Masculine Feminine Pronouns I We The Future: DSM-5.1 and beyond Theorist Agency Communion Freud Ability to work Ability to love Adler (1912) Striving for superiority Social interest Horney (1937) Moving against others Moving towards others Fromm (1941) Separate entity Oneness with the world Erikson (1950) Autonomy; Generativity Basic trust; Intimacy Sullivan (1953) Need for power Security Leary (1957) Control Affiliation Foa (1974) Status Love Hogan (1983) Achieving status Achieving popularity Beck (1983) Autonomy Sociotropy McAdams (1985) Power motivation Intimacy motivation Buss (1991) Negotiating status Forming alliances Depue (1995) Dopamine Oxytocin Digman (1997) Beta (E, O) Alpha (N, A, C) The Future: DSM-5.1 and beyond The Interpersonal Circumplex The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Personality Disorders The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Severity and Style The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Severity and Style Profile 1: High Severity, Cold Style Profile 2: High Severity, Warm Style Dominant Cold Dominant Warm Cold Submissive Profile 3: Low Severity, Warm Style Dominant Warm Submissive Cold Submissive The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Heterogeneity in GAD Dominant Antagonistic Extraverted Cold Warm Introverted Agreeable Submissive The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Heterogeneity GAD (Salzer et al., 2008) Bulimia Nervosa (Hopwood et al., 2007) Depression (Cain et al., 2011) PTSD (Thomas et al., 2012) Social Phobia (Kachin et al., 2001) Fear of Failure (Wright et al., 2009) The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Levels within Systems The inter-individual structure of the IPC allows for a comparison of functioning interpersonal several domains Leary’s (1957) levels and process dissociation Self/other report IPC assessment batteries Traits (Markey & Markey, 2009; Wiggins, 1995) Behaviors (Moskowitz, 1994) Problems (Alden, Wiggins, & Pincus, 1990; Soldz, Budman, Demby, & Merry, 1995) Efficacies (Locke & Sadler, 2007) Strengths (Hatcher & Rogers, 2009) Values (Locke, 2000) Sensitivities (Hopwood et al., 2009). The Future: DSM-5.1 and beyond (BC); 135° Competitive Vindictive Sensitive to Antagonism (DE); 180° Indifferent Cold-hearted Sensitive to Remoteness (FG); 225° Aloof Socially Avoidant Sensitive to Timidity (PA); 90° Assertive Domineering Sensitive to Control A g e n c y (NO); 45° Gregarious Intrusive Sensitive to Attention Seeking Communion (LM); 0° Warm Overly Nurturing Sensitive to Affection (JK); 315° Trusting Exploitable Sensitive to Dependency (HI); 270° Submissive Nonassertive The Future: DSM-5.1 and beyond Sensitive to Passivity Case Example The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Variability Across Situations Lewin (1936): B = f (P, E) Leary (1957, p. 121) proposed two variance parameters related to problematic functioning “rigidity, which brings a narrow adjustment to one aspect of the environment, and unstable oscillation, which is an intense attempt to adjust to all aspects of the presented environment.” The Future: DSM-5.1 and beyond Variability in Intra-individual Structure r=0 r=– r=+ The Future: DSM-5.1 and beyond Intra-individual Variability: Pulse Dominant Antagonistic Extraverted Warm Cold Introverted Agreeable Submissive (Moskowitz & Zuroff, 2004) Intra-individual Variability: Spin Dominant Antagonistic Extraverted Warm Cold Introverted Agreeable Submissive (Cote, Moskowitz & Zuroff, 2011; Erikson, Newman, & Pincus, 2009; Moskowitz & Zuroff, 2004; Russel et al., 2007) Interpersonal Taxonomy of Dynamics: Complementarity (Carson, 1969; Sadler et al., 2009) Dominant Antagonistic Extraverted Cold Warm Introverted Agreeable Submissive The Future: DSM-5.1 and beyond Interpersonal Taxonomy of Dynamics: Copy Processes (e.g., Critchfield, 2009) Identification Recapitulation Dominant Antagonistic Extraverted Introjection Cold Warm Introverted Agreeable Submissive The Future: DSM-5.1 and beyond Interpersonal Assessment of Dynamics Across Situations Different relationships Same relationship, different context Within Situations Course of a difficult interaction Psychotherapy session The Future: DSM-5.1 and beyond Interpersonal Variability Across Situations (Roche et al., 2013) The Future: DSM-5.1 and beyond Interpersonal Variability Across Situations (Roche et al., 2013) The Future: DSM-5.1 and beyond Procedure for Assessment of Interpersonal Variability within Situations The Future: DSM-5.1 and beyond Complementarity Coefficient Warmth Control r = -1 1 Time The Future: DSM-5.1 and beyond Intra-individual Structure in Psychotherapy Gloria with Ellis Gloria with Rogers r = .19 r = .12 Gloria with Perls r = –.56 The Future: DSM-5.1 and beyond Assessment of Interpersonal Dynamics in Psychopathology Control Experimental BPD The Future: DSM-5.1 and beyond Cross-correlation: Affiliation r = .86 The Future: DSM-5.1 and beyond Assessment of Interpersonal Dynamics Generally strong complementarity effects on both dimensions overall Both participants were warmer in the control condition (d = .65 for women, 1.30 for men) Greater complementarity on warmth for the experimental group (d = 1.07) Greater complementarity on dominance for the control group (d = .65) The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Clinical Styles (Andrews, 1989) Dominant Ellis Antagonistic Perls Extraverted Beck Cold Davanloo Warm Rogers Introverted Kernberg Agreeable Kohut Submissive The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Interventions Two implications Selection into best-fitting school Therapeutic flexibility “Evidence-Based Practice” Using certain techniques Using techniques certain ways The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Therapeutic Tasks (Tracey, 1999) The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Supervision (Tracey et al., 2012) Parallel processes in supervision occur when (1) the therapist brings the interaction pattern that occurs between the therapist and client into supervision and enacts the same pattern but with the therapist trainee in the client's role, or (2) the trainee takes the interaction pattern in supervision back into the therapy session as the therapist, now enacting the supervisor's role. We examined these processes in the interactions of 17 therapy/supervision triads (i.e., supervisor, therapist/trainee, and client). Each session was rated for dominance and affiliation, and the similarity of these dimensions across equal status pairs (supervisortherapist and trainee-client) was examined. It was hypothesized that if parallel process existed, there would be more similarity in dominance and affiliation between equal status pairs in contiguous sessions than would be true relative to general responses; the dominance and affiliation would be more closely matched than would be expected given general response tendencies. This was examined separately for each supervision triad using single-case randomization tests. The Future: DSM-5.1 and beyond Interpersonal Taxonomy: Supervision (Tracey et al., 2012) Significant results were obtained for each dyad indicating the presence of parallel processes in each supervision triad. Additionally, the relation between parallel processes over the course of treatment and client outcome was examined using hierarchical Bayesian modeling. Results indicate that a positive client outcome was associated with increasing similarity of therapist behavior to the supervisor over time on both affiliation and dominance (increasing parallel process) and an inverted U pattern of highlow-high similarity of client behavior to trainee behavior over time. This study provides support for the existence of bidirectional parallel processes at the level of interpersonal interaction. The Future: DSM-5.1 and beyond Affective Taxonomy: Trait and State Temperament dimensions (Rothbart & Ahadi, 1994; Watson et al., 2009) Positive Emotionality/Surgency Negative Emotionality (Constraint/Effortful Control) Adult personality dimensions Neuroticism Extraversion (Conscientiousness) State affects (Watson et al., 2009; Russell, 1980, Carver et al., 1994) Positive Affect/Arousal/Activation Negative Affect/Valence/Inhibition The Future: DSM-5.1 and beyond Affective Categories and Dimensions The Future: DSM-5.1 and beyond Step 4: Functions The Future: DSM-5.1 and beyond Step 4: Functions (CAPS) The Future: DSM-5.1 and beyond Step 4: Functions The Future: DSM-5.1 and beyond Functional Affective Dynamics: Case example r = .42 Step 5: Psychiatric Taxonomy Categories are still arbitrary, but now there is a clinically useful and evidence-based system underneath it Nomothetic Idiographic The Future: DSM-5.1 and beyond Psychiatric Taxonomy: Step A Review Systems Interpersonal Affect Agency Communion Organization Arousal Valence Constraint Intellect Intelligence Achievement Attention Memory Executive Functioning Schizotypy The Future: DSM-5.1 and beyond Psychiatric Taxonomy: Step B Discern Patterns Interpersonal Affect Agency + Communion Organization Arousal + Valence Constraint Intellect Intelligence Achievement Attention Memory Executive Functioning Schizotypy The Future: DSM-5.1 and beyond Psychiatric Taxonomy: Step C Get specific durations, frequencies, and contexts Interpersonal Affect Agency + elevated in last 2 months Communion Organization Arousal + elevated in last 2 months Valence Constraint Intellect Intelligence Achievement Attention Memory Executive Functioning – functionally related to affective arousal Schizotypy The Future: DSM-5.1 and beyond Psychiatric Taxonomy: Step D Establish Dysfunction Interpersonal Affect Agency + lost friendships and job Communion Organization Arousal + poor sleep and eating habits Valence Constraint Intellect Intelligence Achievement Attention Memory Executive Functioning – disorganization and poor planning Schizotypy The Future: DSM-5.1 and beyond Psychiatric Taxonomy: Step E Apply diagnostic match Agency + lost friendships and job Arousal + poor sleep and eating habits Executive Functioning – disorganization and poor planning How to do this is an interesting question The main difference in this approach is that the symptom domains are all cross-cutting There would still be a need for specific indicators (e.g., trauma, eating, objects of obsessions) The Future: DSM-5.1 and beyond Another Example Presenting concerns: Suicide risk, loneliness, lack of support, impulsive aggression Affect Impulse control: low NA: high, vacillates from anger to sadness to emptiness rapidly; moderated by attachment loss PA: low Interpersonal Organization: low D: low, moderated by anger W: low, but with underlying desire/wish for closeness Cognitive PSY: low IQ: high Most likely diagnosis? The Future: DSM-5.1 and beyond A Third Example Suppose I refer a patient with Bulimia Nervosa. How many questions does that answer? What else would you want to know? The Future: DSM-5.1 and beyond Another Example Presenting concerns: Eating in binges, marital conflict Affect Impulse control: low NA: high but often suppressed, moderated by sense of control PA: low, moderated by loss of control Interpersonal Organization: somewhat low D: low, but with underlying wish for control W: high, but with underlying desire/wish for separation Cognitive PSY: low IQ: average The Future: DSM-5.1 and beyond Implications Integration of brain and behavior Currently exists an antagonism between basic research and practice Systems thinking is an integrative path forward with momentum in basic and applied clinical psychology and medicine Integration of dimensional and categorical thinking Categories are arbitrary constellations of dimension scores Broad and hierarchical: beyond lumping and splitting Trans-theoretical Dominant viewpoints are political Beyond extra-scientific influences and treatment packaging Focused on the lived life and clinical setting Box’s models… Beyond the DSM as serving all purposes Practical utility Existing assessment tools Dynamic assessment tools Existing treatment models Integrative treatment models Revisiting the notion of treatment matching The Future: DSM-5.1 and beyond Pushing it even further: Including dynamics Presenting problem Themes on 2 circles plus PSY, C, and cognition Can vary in hierarchical specificity depending on initial findings Can vary across levels within systems Could use multi-method assessment Patterning in problem situations Influence of exogenous variables Treatment of “personality” with relationship or treatment of “symptoms” with technique: Involvement of interpersonal issues Dynamic assessments of functions with joystick, EMA Developmental dynamics Implicit wishes and Fears Optional Match to diagnostic concept The Future: DSM-5.1 and beyond Pushing it even further: A Clinical Example Presenting concerns: Suicide risk, loneliness, lack of support, impulsive aggression Affect Impulse control: low NA: high, vacillates from anger to sadness to emptiness rapidly; moderated by attachment loss PA: low Interpersonal Organization: low D: low, moderated by anger W: low, but with underlying desire/wish for closeness Cognitive PSY: low IQ: high Diagnosis: Borderline Personality Disorder The Future: DSM-5.1 and beyond Lower in the Hierarchy NA PAI Suicidal Ideation, Affective Depression, Affective Instability, Self-harm, Traumatic Stress Informant DSM-5 Separation Insecurity, Depressivity, Anhedonia Rorschach D, Afr, SumV, S-CON+ Impulse Control PAI Self Harm, Sensation Seeking, Aggression Informant DSM-5 Risk Taking, Hostility Rorschach EB+ (extratensive), S-% Detachment PAI Nonsupport, Resentment Informant DSM-5 Submissiveness, Suspiciousness Rorschach AG, GHR:PHR The Future: DSM-5.1 and beyond Levels of interpersonal functioning The Future: DSM-5.1 and beyond Daily Diary: Functional precursors to suicidal ideation r = .42 Pushing it even further: A Clinical Example Joystick Findings Therapist submissiveness leads to patient coldness Initially Discussed this with patient Patient submissive, eventually dominant interpreted therapist submissiveness as disinterest Pattern remitted, leading to more efficient and productive sessions The Future: DSM-5.1 and beyond Pushing it even further: A Clinical Example Formulation: desires warmth but expects coldness so acts aloof, gets coldness back. Attachment anxiety + temperamentally limited impulse control lead to maladaptive behaviors including aggression and selfharm. Treatment Hypotheses: Short term: Warmth on the part of the therapist will provide comfort and will reinforce the patient’s warmth. Discussing and planning more adaptive ways to cope with negative feelings will reduce risk for self-harm and relationship problems. Long-term: Focusing on painful affects associated with significant developmental experiences will improve mentalization, perceptual accuracy, affect regulation, maturity of defenses, and functioning. The Future: DSM-5.1 and beyond Two Concluding Points Diagnosis is essentially the closest match of idiographic style with a nomothetic concept or category. But level of severity is still an essentially arbitrary clinical decision, which basically amounts to ‘I think this person needs help’. The DSM is a cover for the anxiety created by this responsibility. In order to see the world more as it is, we are going to need to face the fact that this is a value judgment more squarely. The goal of taxonomy is to bridge the gap between researchers and clinicians. Diabetes Example Currently clinicians go from idiographics to diagnosis but there is a lot in between There are advantages of filling this in: Clinicians use more evidence-based models, can do more to tailor treatments to existing research evidence, have an evidence based structure with which to select and organize assessments Researchers not constrained by categories that are not that useful, oriented towards clinically important question The Future: DSM-5.1 and beyond Applying this to your own case Presenting Problems: Diagnosis: Interpersonal System Organization: Agency: Communion: Affect System Constraint: Positive Affect/Arousal: Negative Affect: Cognition Psychoticism: Intellect: Applying this to your own case Environmental Factors: Functional Dynamics: Wishes and Fears: Issues of Culture and Demography: