urinary incontinence
advertisement

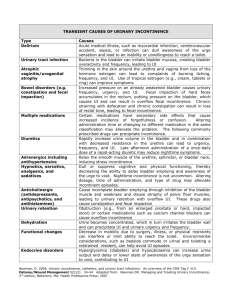
URINARY INCONTINENCE IN THE AGING PATIENT September 2007 Deb Mostek Definition UI is the involuntary loss of urine that is objectively demonstrable and a social or hygienic problem. International Continence Society Prevalence of UI 15-30% of community dwelling persons 65 years and older. F>M until age 80 years, then M=F Up to 50% in LTC GU Age-Related Changes Detrusor overactivity (20% of healthy continent) BPH PVR , nocturia, UO later in day Atrophic vagintis & urethritis ability to postpone voiding, total bladder capacity, detrusor contractility urine concentrating ability, flow DuBeau CE.Urinary Incontinence.Geriatric Review Syllabus Fifth Ed.2002-2004.139-148 Risk Factors for UI Impaired mobility Depression Stroke Diabetes Parkinson’s Disease Dementia (moderate to severe) 1/3 have multiple conditions FI, Obesity, CHF, Constipation, TIAs, COPD, Chronic cough, Impaired mobility & ADLs Consequences of UI Cellulitis, Pressure ulcers, UTI Falls with fractures Sleep deprivation Social withdrawal, depression Embarrassment (50%), interference with activities Caregiver burden, contributes to institutionalization Costs > $16 billion Types of Urinary Incontinence Transient UI (Acute) Established UI (Chronic) Urge UI Stress UI Mixed UI Overflow UI “Functional” UI Transient Incontinence Lower urinary tract pathology Precipitated by reversible factor 1/3 Community dwelling 1/2 Hospitalized incontinent aged patients Causes: Delirium, UTI, Meds, Psychiatric disorders, UO, Stool impaction Restricted mobility Causes of Transient (Acute) Incontinence D I A P P E R S Delirium Infection Atrophic Vulvovaginitis Psychological Pharmacologic agents Endocrine, excessive UO Restricted Mobility Stool impaction Source: Resnick NM. Urinary incontinence in the elderly. Med Grand Rounds. 1984;3:281-290. Pharmacologic Causes Opioids Calcium channel blockers Anti-Parkinsons drugs Anti-cholinergics Prostaglandin inhibitors Depress detrusor activity & produce urinary retention and overflow incontinence Pharmacologic Causes sedatives loop diuretics alcohol caffeine cholinergics (donepezil) awareness, detrusor activity Func & O UI Diuresis overwhelms bladder capacity Urge & O UI Polyuria, awareness Urge & Functional UI Polyuria, detrusor activity Urge detrusor activity Urge Culligan PJ Urinary Incontinence in women Evaluation and Management AFP Pharmacologic Causes, Continued alpha-agonists urethral sphincter tone retention and Overflow alpha-antagonists urethral sphincter tone Stress Mrs. R 85 y/o female brought to the emergency room with new onset urinary incontinence. Daughter is worried about possible UTI and inability to care for patient at home if incontinence persists. PMH: Dementia, hypertension, advanced osteoarthritis, gait disturbance. Meds: ASA 81mg daily, hydrochlorothiazide 12.5 mg daily, calcium with vitamin D tid. Mrs. R SH: lives with daughter and grandson. Dependent on family for assistance with ADL’s. Physical Exam: BP 138/80 P78 R18 T98 Gen: Alert, cooperative, vague historian; Chest: Clear; CV: RRR; Abdomen: Benign; GU: Atrophic changes; Ext: Trace edema Screening Ask sensitively worded questions Detailed History Duration, previous evaluation/treatment? Volume, how often, what situations? Urgency, dysuria, straining? EVALUATION: THE APPROACH Focused H & P for: 1) Reversible conditions 2) Conditions that require Urologic or Gynecologic consult or Urodynamics early on. 3) Function focused approach to the remaining cases 4) Contributing factors Evaluation, continued UA, C&S Creatinine, BUN, Glucose, Calcium, ?PSA Post-void residual Clinical urinary stress test Voiding record Post-Void Residual (PVR) Measure volume of urine left in bladder after voiding by catheter or bladder scan < 50-100 Normal 100—400 Monitor until consistently less than 200cc. > 400cc—Insert Foley catheter Clinical Stress Test Bladder should be full. Ask patient to strain (Valsalva maneuver). If no leakage, have her perform a half sit-up and cough—look for leakage. If no leakage in supine position, repeat testing in standing position. Patient should relax perineum and cough once—if immediate leakage=stress UI; if leakage is delayed several seconds=detrusor overactivity 20 Common Problems in Urology; JM Teichman, Ed. 2001 2003 GAYFP; DB Reuben et al Established Incontinence URGE STRESS Mixed type (both urge and stress) OVERFLOW (increased PVR) “Functional” incontinence Urge Incontinence Most common Detrusor overactivity with uninhibited bladder contractions Unpredictable, abrupt urgency, frequency, variable volumes lost, PVR usually normal (“Post-void residual”—the volume of urine left in bladder after spontaneous voiding) Management: bladder retraining, scheduled toileting, pelvic muscle exercises (PME), pharmacologic agents Stress UI 2nd most common cause in aging females Impaired urethral closure due to insufficient pelvic support, sphincter opens during bladder filling Leakage occurs with intra-abdominal pressure Management: pelvic muscle exercises, biofeedback, electrical stimulation, adrenergic agonists, pessary, surgical interventions. Mixed Incontinence Features of both urge and stress incontinence. Common in older women Management: bladder retraining, pelvic muscle exercises, other pelvic muscle rehabilitative options outlined previously, pharmacologic agents. Overflow UI Detrusor underactivity and/or outlet obstruction Continuous small volume leakage Dribbling, weak stream, hesitancy, nocturia Outlet obstruction=2nd most common cause of UI in Males Detrusor underactivity Urinary retention & overflow Incontinence in 12%F; 29%M Overflow UI Management: Obstruction—Treat cause; -antagonists. Detrusor Underactivity—Review meds, double voiding, intermittent selfcatheterization, Crede’s. “Functional” Incontinence Unable or unwilling to toilet due to physical impairment, cognitive dysfunction, environmental barriers No underlying GU dysfunction Diagnosis of exclusion 3)FUNCTION FOCUSED APPROACH TO REMAINING CAUSES Symptoms: URGE (REFLEX or NEUROGENIC) leakage variable volumes pattern of urine loss unpredictable delay voiding? unable voiding volumes variable STRESS OVERFLOW small volume with intrabd. pressure (cough, sneeze, laugh) able except with intrabd. pressure normal small volume almost continuous able, (at times) small (normally) N o c t u r n a l Yes (pt. is unaware) Rare Yes (dribbling) incontinence 1 1.Rovner ES, Wein AJ, The treatment of Operative bladder in the geriatric patient . Clinical Geriatrics Vol. 10 Number 1 Jan 2002 Mrs. J Pleasant, thin 86 y/o with c/o urgency, frequency, with variable UI for past 2-3 years. PMH: Osteoporosis with old thoracic vertebral compression fractures, hypertension SH: Widowed, lives alone Meds: Calcium w Vit. D tid; alendronate 70 mg weekly; amlodipine 5 mg daily; MVI daily ROS: Mild fatigue, sleep disturbance, admits to depressed ideation. Otherwise negative. Mrs. J PE: BP 126/70 sitting; 118/68 standing. Wt. 44kg Gen: Thin, alert, excellent historian. CV, Pulm, Abd, Neuro: all neg GU: Ext genitalia/BSU/Vag– Atrophic; no pelvic relaxation; Bimanual exam: consistent with previous hysterecomy, no masses. RV:Confirmatory Mrs. J PVR: 250 ml Clinical stress test: Some urine loss after several seconds delay after cough DHIC (Detrusor Hyperactivity with Impaired Contractility) Most common cause of UI in frail and old: Detrusor hyperactivity plus impaired bladder contractility (DHIC). The clinical picture is: a “story” of Urge incontinence with elevated or borderline PVR ie PVR= 100-400 cc range. Management of UI Treat reversible cause (ie. Constipation) Review meds General measures: Behavioral interventions before pharmacologic Rx,. Avoid caffeine & ETOH, minimize evening intake, pads, Surgery last. Pelvic Muscle exercises Motivated patient, careful instruction 56-95% decrease in UI episodes— dependent on intensity of program Focus on pelvic muscles (10 ctx 3-10 times/d)—avoid buttock, abdomen, thigh muscle contraction. Biofeedback may help Bladder Retraining Urge control exercises Scheduled toileting Prompted toileting Pelvic Muscle Rehabilitation Detailed instruction of pelvic muscle exercises Biofeedback techniques Electrical stimulation Anticholinergic Drugs Oxybutynin Tolterodine Trospium Darifenacin Variety of preparations: Immediate Release; Extended Release; Transdermal Outcomes same; Try different agent if one doesn’t work ***** ALL these drugs suppress the detrusor contractility and MAY CAUSE URINARY RETENTION!!! ALWAYS CHECK PVR PRIOR TO PRESCRIBING!!! Overflow UI Obstruction—Treat cause; -antagonists; finasteride Detrusor Underactivity—Review meds, double voiding, intermittent selfcatheterization, Crede’s. Further Urological Evaluation PVR > 400 cc Poor response to treatment Cystometry, cystoscopy, urodynamic studies Evidence of GU tract pathology UI Summary Look for reversible causes and Rx Check PVR (>100 cc investigate further) Start with behavioral interventions before meds Referral and urodynamic studies if no response to usual measures Early referral if underlying GU tract pathology present Acknowledgments Ahronheim JC. Aging. In Epps RP, Stewart SC eds. Women’s Complete Healthbook, 1995. The Philip Lief Group, Inc. and the American Medical Women’s Association, Inc. Stress Urinary Incontinence figure 11.2, p156. Edward Vandenberg, MD who contributed a number of the slides Acknowledgments Wendy Adams, MD MPH who also contributed slides DuBeau CE. Urinary Incontinence. Geriatric Review Syllabus, Fifth Edition 2002-2004. 139-148