PowerPoint - 埼玉医科大学総合医療センター 内分泌・糖尿病内科
advertisement

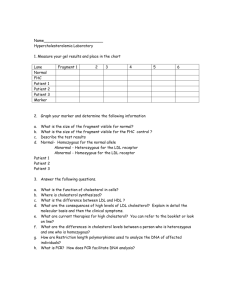
Journal Club Pencina MJ1, Navar-Boggan AM, D'Agostino RB Sr, Williams K, Neely B, Sniderman AD, Peterson ED. Application of New Cholesterol Guidelines to a Population-Based Sample. N Engl J Med. 2014 Mar 19. DOI: 10.1056/NEJMoa1315665 Emerging Risk Factors Collaboration, Di Angelantonio E, Gao P, Khan H, Butterworth AS, Wormser D, Kaptoge S, Kondapally Seshasai SR, Thompson A, Sarwar N, Willeit P, Ridker PM, Barr EL, Khaw KT, Psaty BM, Brenner H, Balkau B, Dekker JM, Lawlor DA, Daimon M, Willeit J, Njølstad I, Nissinen A, Brunner EJ, Kuller LH, Price JF, Sundström J, Knuiman MW, Feskens EJ, Verschuren WM, Wald N, Bakker SJ, Whincup PH, Ford I, Goldbourt U, Gómez-de-la-Cámara A, Gallacher J, Simons LA, Rosengren A, Sutherland SE, Björkelund C, Blazer DG, Wassertheil-Smoller S, Onat A, Marín Ibañez A, Casiglia E, Jukema JW, Simpson LM, Giampaoli S, Nordestgaard BG, Selmer R, Wennberg P, Kauhanen J, Salonen JT, Dankner R, Barrett-Connor E, Kavousi M, Gudnason V, Evans D, Wallace RB, Cushman M, D'Agostino RB Sr, Umans JG, Kiyohara Y, Nakagawa H, Sato S, Gillum RF, Folsom AR, van der Schouw YT, Moons KG, Griffin SJ, Sattar N, Wareham NJ, Selvin E, Thompson SG, Danesh J. Glycated hemoglobin measurement and prediction of cardiovascular disease. JAMA. 2014 Mar 26;311(12):1225-33. doi: 10.1001/jama.2014.1873. 2014年3月20日 8:30-8:55 8階 医局 埼玉医科大学 総合医療センター 内分泌・糖尿病内科 Department of Endocrinology and Diabetes, Saitama Medical Center, Saitama Medical University 松田 昌文 Matsuda, Masafumi 2012年7月より! 第83回 糖尿病臨床カンファレンス 新しい日本動脈硬化学会ガ イドラインに基く糖尿病の脂 質管理 2012/7/3 Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499-502. The Friedewald Equation the ultracentrifugal measurement of LDL is time consuming and expensive and requires specialist equipment. For this reason, LDLcholesterol is most commonly estimated from quantitative measurements of total and HDL-cholesterol and plasma triglycerides (TG) using the empirical relationship of Friedewald et al.(1972). [LDL-chol] = [Total chol] - [HDL-chol] - ([TG]/2.2) where all concentrations are given in mmol/L (note that if calculated using all concentrations in mg/dL then the equation is [LDL-chol] = [Total chol] - [HDL-chol] - ([TG]/5)) the quotient ([TG]/5) is used as an estimate of VLDL-cholesterol concentration. It assumes, first, that virtually all of the plasma TG is carried on VLDL, and second, that the TG:cholesterol ratio of VLDL is constant at about 5:1 (Friedewald et al. 1972). Neither assumption is strictly true. Limitations of the Friedewald equation The Friedewald equation should not be used under the following circumstances: when chylomicrons are present when plasma triglyceride concentration exceeds 400 mg/dL (4.52 mmol/L) in patients with dysbetalipoproteinemia (type III hyperlipoproteine 一次予防の糖尿病患者はすべてLDL-C<120mg/dLを目指すべきであるが、特にこれらの 特徴を持つ患者は管理目標達成を必須としたより厳格な対応が必要と考えられた。またこれら の特徴を複数合併した糖尿病患者は極めて冠動脈疾患発症リスクが高いと予想され、症例に よっては二次予防と同等の管理目標(LDL-C<100mg/dl)が考慮されてもよいと思われる。 On November 12, 2013, updated guidelines for the treatment of high blood cholesterol levels were released by the American College of Cardiology–American Heart Association (ACC-AHA) A Pragmatic View of the New Cholesterol Treatment Guidelines John F. Keaney, Jr., M.D., Gregory D. Curfman, M.D., and John A. Jarcho, M.D. November 27, 2013DOI: 10.1056/NEJMms1314569 Treatment Recommendations and Goals Lifestyle modification focusing on the reduction of saturated fat, trans fat, and cholesterol intake; increase of n-3 fatty acids, viscous fiber and plant stanols/sterols; weight loss (if indicated); and increased physical activity should be recommended to improve the lipid profile in patients with diabetes. A Statin therapy should be added to lifestyle therapy, regardless of baseline lipid levels, for diabetic patients: with overt CVD A without CVD who are over the age of 40 years and have one or more other CVD risk factors (family history of CVD, hypertension, smoking, dyslipidemia, or albuminuria). A For lower-risk patients than the above (e.g., without overt CVD and under the age of 40 years), statin therapy should be considered in addition to lifestyle therapy if LDL cholesterol remains above 100 mg/dL or in those with multiple CVD risk factors. C In individuals without overt CVD, the goal is LDL cholesterol <100 mg/dL (2.6 mmol/L). B In individuals with overt CVD, a lower LDL cholesterol goal of <70 mg/dL (1.8 mmol/L), with a high dose of a statin, is an option. B If drug-treated patients do not reach the above targets on maximum tolerated statin therapy, a reduction in LDL cholesterol of ∼30–40% from baseline is an alternative therapeutic goal. B Triglyceride levels <150 mg/dL (1.7 mmol/L) and HDL cholesterol >40 mg/dL (1.0 mmol/L) in men and >50 mg/dL (1.3 mmol/L) in women are desirable. C However, LDL cholesterol– targeted statin therapy remains the preferred strategy. A Combination therapy has been shown not to provide additional cardiovascular benefit above statin therapy alone and is not generally recommended. A Statin therapy is contraindicated in pregnancy. B Diabetes Care January 2014 vol. 37 no. Supplement 1 S14-S80 The following message was sent to members of the American Association of Clinical Endocrinologists (AACE) in response to recent guidelines published the American Heart Association (AHA) and the American College of Cardiology (ACC): Dear Members, The American Heart Association (AHA) and the American College of Cardiology (ACC) have issued four new guidelines: The Management of Cholesterol, Lifestyle Management to Reduce CV Risk, and, along with The Obesity Society (TOS), guidelines on the Management of Obesity. The AHA, ACC, and the Centers for Disease Control and Prevention (CDC) issued a science advisory on the management of hypertension. AACE was asked to review and endorse the obesity and cholesterol guidelines. After careful consideration by the appropriate scientific committees of our organization, AACE declined to endorse these new cholesterol and obesity guidelines. There are multiple reasons for this decision, including, principally, the incompatibility of these new guidelines with our existing guidelines. Additionally, there are questions and concerns regarding the scientific basis for these new guidelines and the populations of patients at risk from disease who are underserved or ill-considered in these new strategies. It should be noted that European Association for the Study of Diabetes (EASD), the European Society of Cardiology (ESC), and the International Atherosclerosis Society (IAS) also have recently published new guidelines and positions which are somewhat contrary to the AHA/ACC lipids guidelines. Therefore, the new AHA/ACC guidelines are now among many available guidelines, including the AACE Lipids Guidelines, to which clinicians can refer. We are currently thoroughly reviewing all four of the AHA/ACC guidelines and the science advisory on the management of hypertension, and our comments will be released in the near future. In the past, AACE has generally agreed with the Adult Treatment Panel 3 (ATP3) National Cholesterol Education Panel (NCEP) guidelines for cholesterol and lipid management and its update in 2004. No update by the NCEP has been forthcoming since that date. These new guidelines from AHA/ACC focus exclusively on large scale randomized clinical trials. They are highly restrictive regarding the database considered and omit much new information. Furthermore, no research after 2011 has been considered. Taken together, these actions have resulted in a considerable number of at-risk patients being omitted from consideration. A new Coronary Heart Disease (CHD) risk calculator has been introduced as one of these new guidelines. This new calculator is already outdated. It is based upon outmoded data, does not model the totality of the U.S. population, has not been validated, and therefore has only limited applicability. Additionally, the focus of the new Lipid guidelines is initiation of statin therapy and not the level of LDL cholesterol attained. To the extent that full dose statins are recommended, we agree with this position. But, AACE disagrees with the notion of removing LDL goals and that statin therapy alone is sufficient for all at-risk patients. A considerable number of high-risk patients with multiple risk factors, diabetes, and established coronary disease do not attain adequate reductions in LDL cholesterol and other lipid abnormalities without further therapies in addition to statins. Non-statin agents may be needed in combination with statins in very high risk groups to produce adequate LDL-cholesterol reduction to further reduce CHD risk. Failure to set targets for treatment makes the degree of risk reduction produced in these groups unknowable and eliminates proper monitoring of management. Worse, it diverts attention away from the ongoing disease process and may lead to unjustified complacency regarding disease recurrence and its prevention. The new obesity guidelines are similarly limited in their scope. They do not include data past 2011. These new guidelines fail to classify obesity as a disease and continue the paradigm of BMI-centric risk stratification, both of which are contrary to recently stated AACE positions. Moreover, the guidelines do not include any of the new FDA-approved pharmacologic agents to assist with weight loss. As a result, the focus of these new guidelines is primarily on lifestyle intervention and bariatric surgery. This is insufficient to meet the needs of the entire population of patients with overweight or obesity-related complications and is therefore inadequate. AACE welcomes the intent of the AHA and ACC in the creation of these new guidelines but does not agree with the complete content and therefore cannot endorse them. We recommend that AACE members continue to refer to AACE guidelines and position statements on Lipids and Obesity to assist decision making in their practices. http://media.aace.com/press-release/press-statement#sthash.9txqm2AL.dpuf the Duke Clinical Research Institute (M.J.P., B.N., E.D.P.), Department of Biostatistics and Bioinformatics (M.J.P), and Division of Cardiology (A.M.N.-B.), Duke University, Durham, NC; the Department of Mathematics and Statistics, Boston University and the Harvard Clinical Research Institute — both in Boston (R.B.D.); KenAnCo Biostatistics, San Antonio, TX (K.W.); and Royal Victoria Hospital, McGill University, Montreal (A.D.S.). DOI: 10.1056/NEJMoa1315665 Background The 2013 guidelines of the American College of Cardiology and the American Heart Association (ACC–AHA) for the treatment of cholesterol expand the indications for statin therapy for the prevention of cardiovascular disease. Methods Using data from the National Health and Nutrition Examination Surveys of 2005 to 2010, we estimated the number, and summarized the risk-factor profile, of persons for whom statin therapy would be recommended (i.e., eligible persons) under the new ACC–AHA guidelines, as compared with the guidelines of the Third Adult Treatment Panel (ATP III) of the National Cholesterol Education Program, and extrapolated the results to a population of 115.4 million U.S. adults between the ages of 40 and 75 years. For the NCEP ATPIII guidelines, based on the 2004 update: 1. Prevalent cardiovascular disease, defined as coronary heart disease, angina or stroke, and LDL cholesterol of 100 or higher; 2. LDL cholesterol of 190 mg/dL or higher; 3. Diabetes (self-reported or fasting glucose of 126 mg/dL or higher) and LDL cholesterol of 100 or higher; 4. Combination of calculated 10-year coronary heart disease risk (using the Framingham risk calculator) and LDL cholesterol levels: a. Risk of 20% or greater and LDL cholesterol of 100 mg/dL or higher; b. Risk of 10 to 20% and LDL cholesterol of 130 mg/dL or higher with 2 or more risk factors [smoking, hypertension, high-density lipoprotein (HDL) cholesterol less than 40 mg/dL, myocardial infarction or angina in first degree relative before age 50, and age (45 years or older for men, 55 years or older for women)]. c. Risk of less than 10% and LDL cholesterol of 160 mg or higher with 2 or more risk factors; For the 2013 ACC/AHA guidelines: 1. Prevalent cardiovascular disease, defined as coronary heart disease, angina or stroke; 2. LDL cholesterol of 190 mg/dL or higher; 3. Diabetes and LDL cholesterol of 70 mg/dL or higher; 4. Ten-year cardiovascular disease risk of 7.5% or greater, based on the pooled cohort equations and LDL cholesterol of 70 or higher; Patients reporting having been “told to” and “taking prescription for cholesterol” were considered to be receiving lipid-lowering treatment appropriately for both guidelines. * To convert the values for cholesterol to millimoles per liter, multiply by 0.02586. ACC–AHA denotes American College of Cardiology and American Heart Association, ATP III Third Adult Treatment Panel of the National Cholesterol Education Program, IQR interquartile range, and NHANES National Health and Nutrition Examination Surveys. † The number of participants who would be newly eligible for statin therapy according to the new ACC–AHA guidelines, as compared with the ATP-III guidelines, is greater than the net difference (552) because some participants who would have been eligible for statin therapy under the ATP-III guidelines would no longer be eligible under the ACC–AHA guidelines. ‡ Cardiovascular disease includes myocardial infarction, angina, and stroke. Figure 1. Extrapolation of the NHANES Sample to All U.S. Adults, According to Two Guidelines for the Management of Cholesterol. Shown are the criteria used to identify adults who would be eligible for statin therapy, indicating the breakdown of statin use and statin recommendations for the 115.4 million adults between the ages of 40 and 75 years on the basis of the guidelines of the Third Adult Treatment Panel (ATP III) of the National Cholesterol Education Program and the 2013 guidelines of the American College of Cardiology and the American Heart Association (ACC–AHA). The ATP-III guidelines use a combination of an assessment of the 10year risk of coronary disease and the low-density lipoprotein (LDL) level to determine eligibility. To convert the values for cholesterol to millimoles per liter, multiply by 0.02586. Figure S1: Number of United States women and men (millions) recommended for statins by guideline This figure shows the number of men and women aged 40 to 75 recommended for statin therapy for secondary prevention (prevalent cardiovascular disease) and primary prevention under ATPIII and the 2013 ACC/AHA guidelines. Results As compared with the ATP-III guidelines, the new guidelines would increase the number of U.S. adults receiving or eligible for statin therapy from 43.2 million (37.5%) to 56.0 million (48.6%). Most of this increase in numbers (10.4 million of 12.8 million) would occur among adults without cardiovascular disease. Among adults between the ages of 60 and 75 years without cardiovascular disease who are not receiving statin therapy, the percentage who would be eligible for such therapy would increase from 30.4% to 87.4% among men and from 21.2% to 53.6% among women. This effect would be driven largely by an increased number of adults who would be classified solely on the basis of their 10-year risk of a cardiovascular event. Those who would be newly eligible for statin therapy include more men than women and persons with a higher blood pressure but a markedly lower level of lowdensity lipoprotein cholesterol. As compared with the ATP-III guidelines, the new guidelines would recommend statin therapy for more adults who would be expected to have future cardiovascular events (higher sensitivity) but would also include many adults who would not have future events (lower specificity). Conclusions The new ACC–AHA guidelines for the management of cholesterol would increase the number of adults who would be eligible for statin therapy by 12.8 million, with the increase seen mostly among older adults without cardiovascular disease. (Funded by the Duke Clinical Research Institute and others.) Message 2005-06年の米国国民健康栄養調査のデータを基 に、スタチン療法の対象者数に及ぼす米国心臓 病学会と米国心臓協会(ACC-AHA)新規ガイドラ インの影響を推定。スタチン療法対象者は1280 万人増加*[4320万人から5600万人へ]した。対象 者の割合は、心血管疾患のない60-75歳の男性で 30.7%から87.4%へ、女性で21.2%から53.6% へ増加した。 *11540万人のうち 新しいガイドラインでどのくらいoutcomeが変化す るのだろうか?AACEのガイドラインは複雑すぎる 血糖介入による虚血性心疾患イベント抑制 -15% 有意差あり Lancet 2009; 373: 1765–72 血糖介入による脳血管疾患イベント抑制 -7% 有意差なし Lancet 2009; 373: 1765–72 University of Cambridge, Cambridge, United Kingdom (Di Angelantonio, Gao, Khan, Butterworth, Wormser, Kaptoge, A. Thompson, Sarwar, P. Willeit, Khaw, Griffin, Wareham, S. G. Thompson, Danesh); St George's University of London, London, United Kingdom (Kondapally Seshasai, Whincup); Brigham and Women’s Hospital, Boston, Massachusetts (Ridker); Baker IDI Heart and Diabetes Institute, Victoria, Australia (Barr); University of Washington, Seattle (Psaty); Group Health Research Institute, Seattle, Washington (Psaty); German Cancer Research Center, Heidelberg, Germany (Brenner); Inserm, Villejuif, France (Balkau); University Paris-Sud, Villejuif, France (Balkau); Vrije Universiteit Medical Center, Amsterdam, the Netherlands (Dekker); University of Bristol, Bristol, United Kingdom (Lawlor); Yamagata University, Japan (Daimon); Medical University Innsbruck, Austria (J. Willeit); University of Tromsø, Tromsø, Norway (Njølstad); National Institute of Health and Welfare, Helsinki, Finland (Nissinen); University College London, London, United Kingdom (Brunner); University of Pittsburgh (Kuller); University of Edinburgh, Edinburgh, United Kingdom (Price); Uppsala University, Uppsala, Sweden (Sundström); University of Western Australia, Perth, Australia (Knuiman); Wageningen University, Wageningen, the Netherlands (Feskens); National Institute for Public Health and the Environment (RIVM), Bilthoven, the Netherlands (Verschuren); Wolfson Institute of Preventive Medicine, London, United Kingdom (Wald); University of Groningen, University Medical Center Groningen, the Netherlands (Bakker); University of Glasgow, Glasgow, United Kingdom (Ford, Sattar); Sheba Medical Center, Tel Hashomer, Israel (Goldbourt); Hospital 12 de Octubre, Madrid, Spain (Gómez-de-la-Cámara); Cardiff University, Cardiff, United Kingdom (Gallacher); University of New South Wales, Kensington, Australia (Simons); Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden (Rosengren); Medical University of South Carolina, Charleston (Sutherland); University of Gothenburg, Gothenburg, Sweden (Björkelund); Duke University Medical Center, Durham, North Carolina (Blazer); Albert Einstein College of Medicine, New York, New York (Wassertheil-Smoller); University of Istanbul, Istanbul, Turkey (Onat); San Jose Norte Health Centre, Zaragoza, Spain (Marín Ibañez); University of Padova, Padova, Italy (Casiglia); Leiden University Medical Center, Leiden, the Netherlands (Jukema); University of Texas School of Public Health, Houston (Simpson); Istituto Superiore di Sanità, Rome, Italy (Giampaoli); Herlev Hospital, Copenhagen University Hospital, University of Copenhagen, Copenhagen, Denmark (Nordestgaard); Norwegian Institute of Public Health, Oslo, Norway (Selmer); Umeå University, Umeå, Sweden (Wennberg); University of Eastern Finland, Kuopio, Finland (Kauhanen); University of Helsinki, Helsinki, Finland (Salonen); The Gertner Institute for Epidemiology and Health Policy Research, Tel Hashomer, Israel (Dankner); Tel Aviv University, Tel Aviv, Israel (Dankner); The Feinstein Institute for Medical Research, New York, New York (Dankner); University of California, San Diego (Barrett-Connor); Erasmus Medical Center, Rotterdam, the Netherlands (Kavousi); Icelandic Heart Association, Reyjavik, Iceland (Gudnason); University of Iceland, Reykjavik, Iceland (Gudnason); Rush University Medical Center, Chicago, Illinois (Evans); University of Iowa College of Public Health, Iowa City (Wallace); University of Vermont, Burlington (Cushman); Boston University, Boston, Massachusetts (D’Agostino); Georgetown University Medical Centre, Washington, DC (Umans); Kyushu University, Kyushu, Japan (Kiyohara); Kanazawa Medical University, Ishikawa, Japan (Nakagawa); Osaka Medical Center for Health Science and Promotion/Chiba Prefectural Institute of Public Health, Osaka, Japan (Sato); Howard University, Washington, DC (Gillum); University of Minnesota, Minneapolis (Folsom); Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, the Netherlands (van der Schouw, Moons); Johns Hopkins University, Baltimore, Maryland (Selvin). JAMA. 2014;311(12):1225-1233. Importance The value of measuring levels of glycated hemoglobin (HbA1c) for the prediction of first cardiovascular events is uncertain. Objective To determine whether adding information on HbA1c values to conventional cardiovascular risk factors is associated with improvement in prediction of cardiovascular disease (CVD) risk. Design, Setting, and Participants Analysis of individual-participant data available from 73 prospective studies involving 294 998 participants without a known history of diabetes mellitus or CVD at the baseline assessment. Main Outcomes and Measures Measures of risk discrimination for CVD outcomes (eg, Cindex) and reclassification (eg, net reclassification improvement) of participants across predicted 10-year risk categories of low (<5%), intermediate (5% to <7.5%), and high (≥7.5%) risk. Participants with levels of glycemia measures below the mean were excluded. Baseline SD was used to calculate per-SD hazard ratio (HR). Analyses were conducted using studies with information across all levels of each subgroup variable. DCCT indicates Diabetes Control and Complications Trial; HPLC, highperformance liquid chromatography; ITA, immunoturbidimetric assay. A full list of the characteristics examined for heterogeneity is provided in eFigures 5 through 8 in Supplement. The index c estimates the probability that, of two randomly chosen patients, the patient with the higher prognostic score will outlive the patient with the lower prognostic score. Values of c near .5 indicate that the prognostic score is no better than a coin-flip in determining which patient will live longer. Values of c near 0 or 1 indicate the baseline data virtually always determine which patient has a better prognosis. The c index measures a probability; many clinicians are more used to dealing with a correlation index that ranges from -1 to +1. A Kendall or Goodman-Kruskal type of correlation index can easily be constructed by calculating γ = 2(c – .5), where γ is the estimated probability that the prognostic score correctly orders prognosis for a pair of patients minus the probability that it incorrectly orders prognosis. When the prognostic score is unrelated to survival time, gamma is zero. When gamma = .5, the relationship between the prognostic score and survival time is halfway between a random relationship and a perfect relationship, and the corresponding c value is .75. http://fujiitoshiki.com/wordpress/2013/10/17/post-3913/ Results During a median follow-up of 9.9 (interquartile range, 7.613.2) years, 20 840 incident fatal and nonfatal CVD outcomes (13 237 coronary heart disease and 7603 stroke outcomes) were recorded. In analyses adjusted for several conventional cardiovascular risk factors, there was an approximately J-shaped association between HbA1c values and CVD risk. The association between HbA1c values and CVD risk changed only slightly after adjustment for total cholesterol and triglyceride concentrations or estimated glomerular filtration rate, but this association attenuated somewhat after adjustment for concentrations of high-density lipoprotein cholesterol and C-reactive protein. The C-index for a CVD risk prediction model containing conventional cardiovascular risk factors alone was 0.7434 (95% CI, 0.7350 to 0.7517). The addition of information on HbA1c was associated with a C-index change of 0.0018 (0.0003 to 0.0033) and a net reclassification improvement of 0.42 (−0.63 to 1.48) for the categories of predicted 10-year CVD risk. The improvement provided by HbA1c assessment in prediction of CVD risk was equal to or better than estimated improvements for measurement of fasting, random, or postload plasma glucose levels. Conclusions and Relevance In a study of individuals without known CVD or diabetes, additional assessment of HbA1c values in the context of CVD risk assessment provided little incremental benefit for prediction of CVD risk. Message 前向き研究73件から糖尿病または心血管疾 患(CVD)のない参加者29万4998人のデータ を分析し、従来の心血管リスク因子にHbA1c 値を追加するとCVDリスク予測が改善するか を検証。HbA1c値の追加によるCVDリスク予 測モデルのC-index(0.7434)の変化は 0.0018で、CVD10年リスク予測の純再分類改 善度は0.42だった。 1次予防についてで、2次予防だと異なる