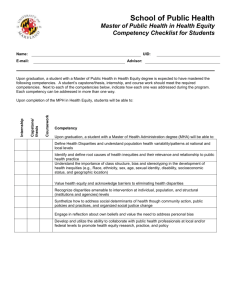
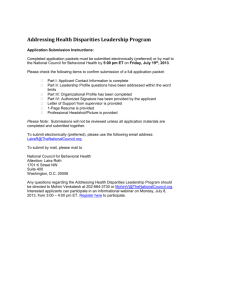
Manual for Addressing Health Disparities
advertisement

Taking Action to Address Health Disparities Guidelines for Implementing Health Promotion and Chronic Disease Prevention Strategies _____________________________________________________________________________________ This guidance document was developed to help employees of the Health Promotion and Chronic Disease Prevention Section of the Texas Department of State Health Services to: Raise awareness about health disparities and their impact on community growth and development – descriptions of health disparities and their causes. Engage program staff, stakeholders, and community partners in conversations about health disparity-related problem and solutions – guide efforts to promote systems change. Take action to eliminate health disparities and improve the health of all residents – information and steps to help program staff, stakeholders, and community partners increase health equity. _____________________________________________________________________________________ This document was developed by the Texas Health and Human Services Commission, Center for Elimination of Disproportionality and Disparities, Texas State Office of Minority Health Acknowledgements We would like to express our appreciation to the following individuals who contributed to the development of this guidance document: Rosanna Barrett, DrPH, MPH Texas Health and Human Services Commission, Center for Elimination of Disproportionality and Disparities, Texas State Office of Minority Health Courtney McElhaney Peebles, MPH, CHES Texas Health and Human Services Commission, Center for Elimination of Disproportionality and Disparities, Texas State Office of Minority Health Brandi Mayes, MPH Department of State Health Services, Division of Disease Control and Prevention, Health Promotion and Chronic Disease, Primary Prevention Branch, Community Transformation Grant Ramah Leith, MPH Department of State Health Services, Division of Disease Control and Prevention, Health Promotion and Chronic Disease, Primary Prevention Branch, Community Transformation Grant Rocky Payne, MA Department of State Health Services, Division of Disease Control and Prevention, Health Promotion and Chronic Disease, Primary Prevention Branch, Community Transformation Grant Christina Thi, MPH, RD, LD Department of State Health Services, Division of Disease Control and Prevention, Health Promotion and Chronic Disease, Primary Prevention Branch, Community and Worksite Wellness Program Page 1 of 35 Table of Contents Introduction and Background 3 Defining Key Terms 4 Defining the Problem 5 Texas Model for Addressing Disproportionality and Disparities 6 Chronic Disease in Texas 8 I. Prevalence and Mortality 8 II. Economic Impact 9 Addressing Health Disparities in Texas 10 Guidelines for Addressing Health Disparities 14 I. II. III. IV. V. VI. VII. VIII. 17 25 26 27 31 31 33 33 Gathering Data and Assessing Health Disparities in Target Communities Using Health Data to Inform Activities Developing Multi-Sector Partnerships/Coalitions Applying Best Practices to Intervention Strategies Developing Culturally and Linguistically Appropriate Messages Evaluating Programmatic Processes and Outcomes Disseminating Best Practices Sustaining Practice-based Interventions Summary 34 Page 2 of 35 Introduction and Background The Texas Department of State Health Services (DSHS) Health Promotion and Chronic Disease Prevention (HPCDP) Section is charged with providing “information, education, resources, and assistance to the people of Texas to make healthy life choices, reduce the human and economic impact of poor health, reduce the incidence of premature death and disability, and promote healthy communities1.” Ultimately, the goal of the Section is to coordinate efforts between communities, coalitions, and stakeholders to support and sustain an environment that makes possible a whole and healthy Texan.2 According to the Centers for Disease Control and Prevention (CDC), chronic diseases such as heart disease, stroke, cancer, diabetes, and arthritis are among the most common, costly, and preventable of all health problems in the United States (U.S.). Seven out of 10 deaths among Americans each year resulted from chronic diseases, and heart disease, cancer, and stroke account for more than 50% of all deaths each year in the United States.3 Several modifiable health risk factors have been identified to prevent illness, suffering, and early death related to chronic diseases, including tobacco use, poor nutrition, and physical inactivity. Coordinating the efforts of the chronic disease prevention and health promotion programs when targeting these common risk factors is the logical next step in public health, and the Section has made great strides in coordination of its programs. This document combines this spirit of coordination with a focus on populations that experience disproportionate burden of chronic disease. Though the Section’s efforts are designed to reach the entire population of the State of Texas, special emphasis must be placed on reducing health disparities among population subgroups if disease prevalence is to be truly impacted. Where there are no grocery stores or fresh food markets, it is clear that individuals’ access to fresh fruits and vegetables will be limited. As individuals that live in communities, it is easy for us to see these outcomes as a possibility for others, but in our work these factors can be difficult to include, or forgotten entirely, when designing programs and/or selecting service providers at the community level. Similarly, it is difficult for individuals to be physically active if there are no parks, walking trails and sidewalks in their communities. In some neighborhoods, it may be unsafe to walk or engage in outdoor activities because of the absence of pedestrian crossings, street lights, and adequate security. Unless a true assessment of a community’s resources is completed before a program is implemented, or community input is provided during the process, it is difficult to select interventions that will truly engage impacted populations and result in our desired outcomes. Populations that are disproportionately impacted by chronic diseases are more likely to be concentrated in communities that do not have grocery stores or fresh food markets, or that lack parks, walking trails, or other infrastructure to support physical activity. 1 Texas Health and Human Services System. (July 10, 2010). Health and Human Services Systems Strategic Plan 2011-2015. Retrieved April 18, 2011 from Chapter I: Statewide Vision, Mission, and Philosophy: http://www.hhs.state.tx.us/StrategicPlans/HHS05-09/final/pdf/Chapter01.pdf 2 Health Promotion and Chronic Disease Prevention Section. New Employee Manual. May 2012. 3 Kung HC, Hoyert DL, Xu JQ, Murphy SL. Deaths: final data for 2005. National Vital Statistics Reports 2008;56(10). Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf Page 3 of 35 It is also important to note that an individual's ability to access health-related opportunities is influenced by socioeconomic and lifestyle characteristics such as race/ethnicity, education level, economic status, language, culture, mental and physical capability, working and commuting hours, and personal and family obligations. These are critical factors that should be considered when designing and implementing interventions to eliminate chronic disease health disparities. This guidance document provides evidence- and practice-based examples of addressing chronic disease disparities by illustrating how the concepts of health equity can be achieved through Section activities by: Promoting tobacco-free environments in public places and work sites, with a focus on reducing exposure to second-hand smoke for all residents. Increasing access to fruits and vegetables via healthy food retail with a focus on underserved communities. Increasing access to opportunities for physical activity with a focus on disparate populations. Using data to identify populations that experience disproportionate chronic disease outcomes, and determine culturally appropriate strategies for reducing health disparities. This guidance document presents a process that can be referenced depending on infrastructure, capacity, and resources inherent to the program and disease for which health disparities are being examined. This document is designed to give an overview of a suggested process for planning, implementing, and evaluating interventions to eliminate/reduce chronic disease health disparities. Links to other resources and examples of success stories in Texas communities are provided to guide community-based chronic disease intervention efforts. Defining Key Terms The following terms, with the exception of health inequalities and built environment, are from the Health Promotion and Chronic Disease Prevention Section Health Disparities Glossary that was approved October 2013. Additional terms can be located in the full glossary, contained within the appendix of this document as well as on SharePoint for Section employees. Health Disparities are preventable differences in the burden of disease, or availability of opportunities to achieve optimal health that are experienced based on gender identity, race, ethnicity, education, income, disability status, sexual orientation, primary language, health literacy, or geography.4 Health inequalities, sometimes used interchangeably with the term health disparities, this term is more often used in scientific and economic literature to refer to summary measures of 4 Centers for Disease Control and Prevention. (n.d.) Adolescents and School Health – Health Disparities. Retrieved July 25, 2013 from CDC: http://www.cdc.gov/healthyyouth/disparities/index.htm Page 4 of 35 population health associated with individual- or group-specific attributes (e.g., income, education, or race/ethnicity).5 Health inequities are systemic, unjust, unnatural, and avoidable differences in health status in the distribution of morbidity and mortality rates across population groups that are sustained over time and generations, and beyond the control of individuals.6 Health Equity is the concept that everyone has the opportunity to attain their full health potential and no one is disadvantaged from achieving this potential because of their social position or other socially determined circumstances.7 Social Determinants of Health the circumstances in which people are born, grow up, live, work, pray, and age, as well as the systems put in place to deal with illness. These circumstances are in turn shaped by a wider set of forces: economics, social policies, and politics.8 Built environment refers to the human-made surroundings that provide the setting for human activity, ranging from buildings and parks or green spaces in communities or neighborhoods. The built environment usually includes availability and accessibility of food and drink, and the safety, accessibility, and existence of space for physical activity.9 Additional components of built environments include “bikeability”, "walkability" and healthy food access, such as proximity to grocery stores and community gardens. Both “walkability” and “bikeability” have been cited as determinants of physical activity. “Bikeability” refers to the access to areas for safe biking through bike paths or lanes. Defining the problem Racial and ethnic subpopulations, persons with disabilities, persons living in rural areas and other disparate or vulnerable groups are more likely to experience barriers to achieving optimal health outcomes. In Texas, racial and ethnic groups are disproportionately impacted by chronic diseases, particularly cancers, diabetes, and cardiovascular disease and stroke. 5 Asada, Y. (2010). A summary measure of health inequalities for a pay-for-population health performance system. Prevention of Chronic Disease, 7:A72. s.l. : Retrieved from: http:www.cdc.gov/pcd/issues/2010/jul/09_0250.htm. 6 Holfrichter, R. (2006). Tackling Health Inequities Through Public Health Practice: A Handbook for Action. The National Association of County and City Health Officials, Washington D.C. and The Ingham County Health Department. Lansing, MI. Retrieved July 24, 2013 from http://www.naccho.org/topics/justice/upload/naccho_handbook_hyperlinks_000.pdf. 7 Brennan Ramirez, L., Baker, E., & Metzler, M. (2008). Promoting Health Equity: A Resource to Health Communities Address Social Determinants of Health. Atlanta, GA: Centers for Disease Control and Prevention. 8 World Health Organization. (n.d.) Key Concepts: Social Determinants of Health. Retrieved July 23, 2013 from http://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en/index.html 9 Huang, T.T., Drewnowski, A., Kumanyika, S.K., & Glass, T.A. (2009). A systems-oriented multilevel framework for addressing obesity in the 21st century. Preventing Chronic Disease, 6(3): A82. Page 5 of 35 The guiding principle for improving minority health states that “The future health of the nation will be determined to a large extent by how effectively we work with communities to reduce and eliminate health disparities between non-minority and minority populations experiencing disproportionate burdens of disease, disability, and premature death.”10 Although the occurrence of chronic disease is a function of biology, genetics, and behavioral factors, the roles of social, environmental, and economic factors increasingly contribute to the heightened prevalence of chronic diseases. Chronic diseases and their risk factors are impacted by the social environment, including societal and cultural norms for smoking, eating, being active, and accessing medical care. With these factors in mind, it is important to engage program staff, stakeholders, and community members in the assessment, development, implementation, and evaluation of health promotion and chronic disease prevention strategies aimed at eliminating health disparities among vulnerable subpopulations. Texas Model for Addressing Disproportionality and Disparities The core principles of the Texas Model for Addressing Disproportionality and Disparities (TMADD) as embodied by the Center for Elimination of Disproportionality and Disparities (CEDD) can be easily applied to the work involved in eliminating chronic disease health disparities. The five (5) principles and their applications are outlined below in Table 1. The relevance of each principle to work activities, where applicable, will be mentioned throughout this document. Table 1. Texas Model for Addressing Disproportionality and Disparities Principles Advancing data driven strategies Application of Principles Increasing the availability, quality, and use of data by ensuring that data collection standards for race, ethnicity, sex/gender, primary language, disability status, etc., are implemented in data collection activities (e.g., surveys) and are used consistently by all programs, and that results are made available to the public; ensuring relevant data that clearly define the population at greatest risk are collected (race, ethnicity, primary language, geographic location, etc.,); use data to identify and map highneed/disparate areas, and encourage alignment of funding and program activities to meet these needs; and ensure the appropriate use of disparities data, particularly for the development of intervention strategies that address the root of the problem (systems: policies, procedures, etc.), not just the symptoms or conventionally viewed causes. 10 Centers for Disease Control and Prevention, Office of Minority Health & Health Disparities. (n.d.) Eliminating Racial & Ethnic Health Disparities. Retrieved January 15, 2014 from http://www.cdc.gov/omhd/about/disparities.htm Page 6 of 35 Developing Leaders Engaging Communities Collaborating Across Systems Promoting Work Defined by Race Equity Principles Engage leadership in learning opportunities and trainings on how to best address health disparities through communitybased intervention efforts that are specific to the vulnerable populations as identified by the data: identify the root (core) of problems, barriers or challenges, and brainstorm potential solutions to implementation; support community interventions that address the needs of residents as identified by the community; make decisions (i.e., policies, infrastructure, programmatic, and environmental) that will produce positive outcomes for community members and/or vulnerable populations. Encourage staff at all levels to become leaders in health equity. Support the development of a culturally competent workforce that demonstrates best practices through equitable service design and delivery, and access to programs and services. Engage community members when conducting needs assessments or collecting local data to get their input on what is most needed in their communities, and to obtain "buy-in" for successful implementation, sustainability of the project, and to produce long-lasting impacts. Programs should seek to develop relationships with community leaders or organizations that have established community ties before writing grants and designing programs, in order to better determine community needs and capacity for implementation of Section activities. Ensure adequate representation of community or vulnerable populations (race/ethnicity, geographic, etc.) on councils to ensure a perspective other than professionals in the field is present when state plans are being developed and decisions are made. To avoid creation and/or maintenance of a siloed approach to addressing health disparities. Integration of activities across systems to reduce duplication, align or leverage resources where appropriate, and eliminate administrative burdens that limit efficient use of resources. Race equity principles include learning from history, celebrating culture, analyzing power, developing leaders, reshaping gatekeeping, maintaining accountability, networking, collaborating across systems, understanding the manifestations of racism, and undoing internalized racial oppression. Additional information on antiracist principles can be found from CEDD. Can be accomplished through trainings that promote equity (fair and just treatment for all), and focus on ongoing societal efforts to address avoidable inequities, historical and contemporary injustices, and the elimination of disparities. The Center for Elimination of Disproportionality and Disparities (CEDD), is working to expand the scope of its efforts to eliminate health disparities by identifying and strategically confronting the connections between health disparities and the social determinants of health, and reforming/modifying proposed strategies for achieving positive outcomes. In addressing Page 7 of 35 chronic disease health disparities, the Center’s efforts are aimed at working collaboratively with partners and stakeholders across systems to: Enhance the capacity of systems to eliminate health disparities. Align the Center’s core principles with the goals, strategies, and actions of programs. Improve coordination of state, regional, and local efforts for achieving health equity. Thoughtfully and authentically engage community members in the process of addressing health disparities and improving health outcomes. Chronic Disease in Texas Prevalence and Mortality According to the 2012 Texas Department of State Health Services (DSHS) Cardiovascular Disease in Texas11 Report, in 2010; nearly one (1) out of three (3) deaths (30.5%) in Texas are due to cardiovascular disease, and 38,096 Texans (22.9% of total deaths in Texas) died from heart disease. In 2010, more Texans died from heart disease and stroke compared to the rest of the United States (U.S.), and Texas ranks in the twenties, thirties, and forties for cardiovascular diseases, stroke, and common risk factors that are associated with these diseases. 39,072 Texans (22.1% of total deaths in Texas) died from malignant neoplasms (cancer) in 201012; prevalence data from 2010 for all sites of cancer is slightly more than 10%13. As with so many other chronic conditions, adequate prevention, diagnoses, and treatment of risk factors associated with development of cancer has the potential to significantly decrease the impact this disease has on our state. Representing opposite ends of the life-course, chronic diseases like asthma and Alzheimer’s disease are also impacting the health of the state. Nationwide, the prevalence of asthma has increased since the late 1990s; this trend holds true for Texas as well. Though asthma is the most prevalent chronic disease among children (8%13), and is one of the most frequent reasons cited for hospitalization of children, prevalence of asthma in adults is approximately seven percent14. This falls short of the decrease that would be expected if asthma were truly a “children’s disease”, and exemplifies the chronic nature of the disease. Accounting for 3.13% of deaths in 2010, Alzheimer’s disease is the 6 th leading cause of death in Texas. Prevalence data from 2010 indicates that approximately 340,000 individuals are living with Alzheimer’s disease, with an estimated 852,820 individuals providing unpaid care and 11 Ang, R. (2012). Cardiovascular Disease in Texas: A Surveillance Report- 2012. Texas Department of State Health Services, Austin, TX. Retrieved January 21, 2014 from http://www.dshs.state.tx.us/wellness/data.shtm 12 Texas Department of State Health Services, Vital Statistics Annual Report, Mortality Narrative 2010. Retrieved January 23, 2014 from http://www.dshs.state.tx.us/chs/vstat/vs10/nmortal.shtm. 13 Texas Cancer Registry, Cancer Epidemiology and Surveillance Branch, Texas Department of State Health Services. Retrieved February 11, 2014 from http://www.dshs.state.tx.us/tcr/default.shtm.. 14 Texas Department of State Health Services, Center for Health Statistics, Behavioral Risk Factor Surveillance Survey (BRFSS), 2012. Page 8 of 35 support to those with the condition15. These statistics highlight that not only do chronic diseases impact the individual diagnosed with the condition, but the effects of chronic disease on the state also include caregivers and loved ones. Examining diabetes prevalence in Texas reveals that nearly 11% of the State has been diagnosed with diabetes, and of those individuals, nearly one-quarter reported one or more comorbidities such as overweight or obesity, cardiovascular disease, heart disease, hypertension, stroke, and kidney disease.16 Because there are so many comorbid conditions that are seen with diabetes, it is perhaps unsurprising that diabetes only accounts for 2.85% of deaths in Texas, though this is still large enough to be the 7 th leading cause of death statewide. Related to diabetes, though distinct conditions, nephritis and related diseases of the kidney combined were the 8th leading cause of death in Texas. The overlap between these chronic conditions, and the populations that are bearing excessive disease burden, highlights the urgent need for increasing access to healthy lifestyle choices. Systems-level changes (e.g., smoke-free environments, physical activity, and healthy foods and beverages), rather than efforts solely focused on individual behavior change, will greatly reduce the development and exacerbation of chronic diseases and health disparities. Increased access to high quality preventive services (e.g., screening and follow-up care) is essential for minimizing risks, early detection, reducing incidence, delaying onset of disability, alleviating severity of disease, prolonging life, and reducing medical costs associated with emergency hospitalization, and rehabilitation. Economic Impact The cost of not addressing and preventing chronic disease is an important reason for eliminating health disparities in Texas. In Texas: The cost of cancer increased from $25.3 billion in 2010 to an estimated $28.1 billion in 201117 Total charges for hospital stays with any mention of diabetes as a principle or co-morbid condition in the medical record were $29.05 billion in 201018. Hospital charges for ischemic heart disease exceeded $6.5 billion in 2010.11 Total hospital charges for stroke exceeded $2.7 billion in 2010. 11 People who are obese pay in excess of $1,400 a year more in medical costs than people who are not obese.11 Unpaid caregiver costs for Alzheimer’s in Texas are estimated to be $11.2 billion, the second highest in the nation.15 15 Texas State Plan on Alzheimer’s Disease. (2010). Accessed February 11, 2014 from http://www.alz.org/national/documents/alzheimerstateplan-texas.pdf. 16 Diabetes Prevalence by Demographics and Selected Health Indicators. BRFSS. Center for Health Statistics, DSHS, 2012. Retrieved January 22, 2014. 17 The Perryman Group. (2011). An Economic Assessment of the Cost of Cancer in Texas and the Benefits of the Cancer Prevention and Research Institute of Texas (CPRIT) and its Programs. Retrieved February 11, 2014 from http://www.cprit.state.tx.us/images/uploads/cprit_impact_12-23-11.pdf. 18 Texas Health Care Information Collection (THCIC), DSHS, 2009. Page 9 of 35 Texas businesses lose an estimated $14 billion annually due to healthcare costs and lost productivity associated with Alzheimer’s.15 The cost of asthma-related hospital stays in 2011 was in excess of $622 million.19 Addressing Health Disparities in Texas Addressing health disparities in Texas could result in a dramatic reduction nationwide. Texas is the second most populous state, with an estimated 26,059,203 people in 201220. It is also the second-largest of the 50 states in the U.S., sharing an international border with Mexico to the south, and borders the New Mexico to the west, Oklahoma to the north, Arkansas to the northeast, and Louisiana to the east. Texas has an area of 268,820 square miles (696,200 km 2) and a growing population of 26.1 million residents20. According to the 2010 United States Census, Texas ranked 18th in the U.S. for percentage (12%) of African Americans; only one percent less than that of the nation (13%). Furthermore, the percentage of the Hispanic and Latino population in Texas is approximately two and half times more than that in the nation (38% versus 15%)20. Additional details regarding the demographics of Texas can be found in Figure 1, below. Racial composition of Texas (2010 US Census): White: 80.9% (44.8% non-Hispanic, 36.1% White Hispanic ) Black or African American: 11.8% Native American Native: 0.7% Asian: 3.8% (1.0% Indian, 0.8% Vietnamese, 0.6% Chinese, 0.4% Filipino, 0.3% Korean, 0.2% Pakistani, 0.07% Japanese, 0.05% Laotian, 0.05% Cambodian) Pacific Islander: 0.1% (0.02% Guamanian, 0.01% Samoan, 0.01% Tongan, 0.01% Native Hawaiian) Some other race: 10.5% Two or more races: 2.7% 37.6% of the population Hispanic or Latino (of any race) (31.6% Mexican, 0.5% Puerto Rican, 0.2% Cuban) Figure 1. 2010 Demographics for the State of Texas. Chronic Disease Health Disparities in Texas: As seen in Table 2, below, Texas falls short of Healthy People 2020 goals for nearly all of the health outcomes listed. When prevalence and mortality rates are examined by race and ethnicity, a more dismal scenario is revealed. Diabetes death rates in particular are high among Blacks and Hispanics, with similar trends observed for several other chronic diseases. 19 Texas Health Care Information Collection, 2011 Inpatient Hospital Discharge Public Use Data File. U.S. Census Bureau Announces 2010 Census Population Counts. U.S. Census Bureau. December 21, 2010. Retrieved September 5, 2013. 20 Page 10 of 35 Table 2. Texas Health Disparities Profile: Major Causes of Death and Health Risk Factors Population (2010) (all ages) NonHispanic White NonHispani c Black Hispani c America n Indian/ Alaskan Native 67.8 26.5 3.9 0.8 1.4 Asian/Pacif ic Islander State Total Healthy People 2020 Nationa l Target State Rank 4,779,736 Major causes of death (rate per 100,000)¶ All cause 897.9 1,062.4 288.1 278.6 356.8 921.2 + 52 Heart disease Coronary heart disease 227.0 115.7 261.6 124.7 63.3 32.1 81.2 59.9 66.1 * 231.5 116.0 + 100.8 53 25 Total cancer 191.4 225.2 56.8 33.2 71.6 195.6 160.6 48 Colorectal cancer 16.1 24.2 * * * 17.5 14.5 43 Lung cancer 64.5 55.1 * * * 61.8 45.5 49 47.5 71.2 18.8 * 32.3 51.9 33.8 53 167.9 70.9 * * * 147.4 98.5 47 Diabetes–related Influenza and pneumonia 65.2 18.5 126.4 19.0 17.1 * * * 35.5 * 76.2 18.5 65.8 + 34 41 Unintentional injuries 55.3 35.4 28.1 * 25.9 49.1 36 45 Suicide 17.5 4.9 * * * 13.9 10.2 34 35.9 30.5 30.3 26.2 20.4 50.7 40.9 35.4 20.1 18.8 35.9 28.5 46.1 27.8 21.9 47.4 43.9 35.7 40.0 * * * * * * 39.7 32.8 32.1 24.6 20.4 26.9 30.6 32.6 12 + 52 49 47 42 43 76.6 79.5 67.1 77.4 89.2 55.6 78.2 77.7 61.8 69.7 87.6 49.9 * * * 77.0 81.8 63.2 82.1 + + 14 20 41 71.6 70.7 54.9 * 77.8 100 33 Stroke Chronic obstructive pulmonary diseases (age 45 & over) Health risk factors (percent) § Diagnosed high blood pressure (2011) Obesity (2011) (age 20 & over) No leisure–time physical activity (2011) Smoking currently (2011) Eats 5+ fruits and vegetables a day Preventive care (percent) § Cholesterol screening in past 5 yrs. (2011) Routine check–up in past 2 yrs. (2011) Dental visit within the past year (2010) Health insurance coverage (percent) Health insurance coverage (2011) (ages 18–64) 80.8 ¶ Estimate age-adjusted and for all ages unless noted. § Estimate age-adjusted and for 18 years of age and over unless noted. * Figure does not meet standard of reliability or precision. + No Healthy People 2020 target associated with this health indicator. NOTE: All data are from 2009 unless noted. NOTE: Low numerical rankings indicate better relative health status. NOTE: State rank includes the 50 states, District of Columbia, Guam, Puerto Rico and Virgin Islands, where data are available and reliable. NOTE: Healthy People targets correspond with the Healthy People 2020 Objectives. Data Source: Department of Health and Human Services, Office on Women's Health: Health Status 2020, Health Disparities Profile by State. Available from http://www.healthstatus2020.com/disparities/ChartBookData_search.asp For cardiovascular diseases (CVD), on average, males or all races and ethnicities have slightly higher prevalence, and are more likely to die, than females (Figures 2a and 2b). Meanwhile, African Americans in Texas, regardless of gender, are disproportionately affected by CVD as compared to Whites, and are more likely die from CVD. (Figure 2b). As expected, because of the etiology and life course of chronic diseases, older individuals (65 years and older) have higher prevalence of CVD than individuals in other age groups (Figure 2a). Page 11 of 35 Figure 2a. Prevalence of Cardiovascular Diseases by Race, Ethnicity, Sex, and Age in Texas, 2011-2012 Data Source: Texas Behavioral Risk Factor Surveillance System, DSHS. 2012 Figure 2b. Age-Adjusted Cardiovascular Diseases Mortality Rates by Sex and Race/Ethnicity in Texas, 2011-2012 Data Source: Texas Vital Statistics Unit, DSHS. 2012. From a geographical perspective, in 2012, Public Health Regions (PHRs) 4, 5, and 11 were shown to have the highest prevalence of heart disease when compared to other regions of Page 12 of 35 Texas (Figure 3). 2012 prevalence rates were considerably different from those in previous years; possibly due to enhanced survey methods used in the 2012 BRFSS, or effective public health campaigns in the regions previously identified as having high prevalence. Though it will be discussed later, these changes in prevalence in such a short amount of time are just one example of how important evaluation is when examining public health outcomes, particularly as they relate to health disparities. Figure 3. Age-Adjusted Prevalence of Heart Diseases by Public Health Regions, Texas, 2012 Data Source: Texas Behavioral Risk Factor Surveillance System and Center for Health Statistics, DSHS. 2010. Page 13 of 35 Guidelines for Addressing Health Disparities Although there may be several approaches to addressing health disparities for chronic diseases, this document focuses on systems and environmental changes. Systems and environmental changes have been proven successful for addressing social determinants of health. This highlevel approach has the potential for broader reach, more impacting results, and may be more effective at reaching subpopulations that are at higher risk for, or disproportionately affected by, chronic diseases. Figure 4 illustrates the framework for increasing impact through systemlevel interventions. Figure 4. Health Impact Pyramid: The Framework for Public for Public Health Action Source: Thomas Frieden. (2010). American Journal of Public Health: 100(4) This document provides an eight-step process for achieving health equity. Steps One through Seven are recommended nationally for obesity prevention, a risk factor that impacts nearly all of the chronic diseases the Section works with. Step Eight was added to increase statewide impact and maximize reach of the interventions undertaken by the Section. Consistent communication and adaption of cultural competency should be the core of all these activities. These steps are as follows: 1. Gathering data on chronic disease burden, and assessing health disparities Section program staff should gather data to ensure they understand state, regional, and local demographics, institutions, and relevant programmatic factors. This includes cataloguing other groups, agencies, coalitions, organizations, faith communities, etc., that can partner with or assist the Section with coalition building and/or accessing disparate populations. 2. Using health data to inform activities There are Public Health Regions (PHRs) and communities across the State with multiple and/or overlapping disparate conditions. The Section should explore reaching the most Page 14 of 35 underserved populations when designing interventions and/or selecting providers, while retaining enough flexibility to target populations they believe offer a high likelihood of success. Gathering regional and community-level data on chronic diseases and social and environmental factors that contribute to them is an important step toward addressing health disparities through a health equity lens. 3. Developing multi-sector partnerships/coalitions Building from available data (needs assessments, BRFSS, ACS, etc.), the Section should reach out to a variety of health and community groups to develop partnerships, attract coalition members, identify local champions (i.e., community leaders -e.g., pastors, parent-teacher organizers), and connect with subject matter experts (e.g., city planners, parks and recreational staff, health department staff). There are six legislatively established/mandated councils within the Section, many of which currently have community participation. Given that these councils are in the position to represent key drivers for statewide change, Section/program staff should explore providing formal technical assistance on effective coalition development and sustainability, particularly for those councils that do not have community representation. For those councils that do have community representation, establishing targets for participation by members from vulnerable populations and/or PHRs that experience excess chronic disease burden are another strategy for addressing health equity. 4. Applying best practices to intervention strategies Section/program staff should use the Checklist (located within the Health Disparities Toolkit) as a template for ensuring program activities, policy changes, interventions, etc. address disparities. Additions to the Checklist could include criteria concepts such as affordability, accessibility, high reach/impact potential, multilingual resources, implementing the Culturally and Linguistically Appropriate Services standards, data collection standards, etc. The Literature Review, also included as part of this Toolkit, contains information on best- and promising-practices for interventions targeting populations experiencing disparate health outcomes. Consistent utilization of these tools will further the Section’s ability to address health disparities in an equitable way. 5. Developing culturally and linguistically appropriate messages Section/program staff should ensure that the chronic disease prevention messages developed and used by all programs are appropriate for the population being targeted. Messages should be reflective of cultural norms within the population, and the educational/grade level the messages are written at should be understandable to the intended audience. One method for ensuring that this step is followed is soliciting a review of the message(s) by community representative(s) before they are publicized or distributed. 6. Evaluating programmatic processes and outcomes Section program and evaluation staff members must define process and programmatic success for activities and strategies (as appropriate). Reach numbers can inform some Page 15 of 35 outcome evaluations; however, if media campaigns are part of the intervention, some perception/attitudinal change should be captured as well (e.g., through focus groups with community members). Additionally, programs will likely benefit from processoriented benchmarks, which could be met by demonstrating completion or a significant attempt at completion (e.g., recruitment for coalitions, changing policies, participation in trainings, etc.). If updated quarterly, as it was designed, the Health Equity Dashboard is an excellent way to evaluate these types of process measures for the entire Section. 7. Disseminating best practices Section/program staff should compile and disseminate best practices that have proven successful at the regional or local level. These best practices could be added to the evidence-base for replication in similar localities, which could result in statewide transformation for chronic disease prevention, with the potential for national replication. 8. Sustaining practice-based interventions Section/program staff will need to demonstrate that intervention activities can and will continue beyond the life of grants or other time-limited funding. Addressing health disparities by increasing health equity is a major initiative, and continuing the work beyond an initial project is essential for the long-term goals of the Section to be achieved. Tools/Resources for Addressing Health Equity To implement these steps it is important to have a full understanding of health equity. Several health equity tools are available and can be used as resources, a few are listed below: The Office of Minority Health and Health Equity (OMHHE) The OMHHE works closely with state, tribal, and local governments, as well as nonprofit organizations, to improve health status and eliminate health disparities among Americans of all racial and ethnic groups. The combined resources of CDC/Agency for Toxic Substances and Disease Registry and its partners provide the vital link between policy and practice. http://www.cdc.gov/minorityhealth/resources.html National Partnership for Action (NPA) The NPA Guide to Health Disparities Resources is an easy-to-use guide published by the Office of Minority Health. The NPA guide lists phone numbers and addresses to OMH regional coordinators, Public Health Service minority liaisons, Federal information centers and clearinghouses, and national organizations categorized by target population. https://minorityhealth.hhs.gov/npa/templates/browse.aspx?lvl=2&lvlid=47 Page 16 of 35 CDC Workbook Promoting Health Equity This is a resource to help communities address the social determinants of health through a health equity lens. http://www.cdc.gov/nccdphp/dach/chhep/pdf/sdohworkbook.pdf Unnatural Causes website The website provides several resources on health equity through community-based scenarios. http://www.unnaturalcauses.org/resources.php Health Equity Resources for State Practitioners Addressing Health Disparities This document provides examples of strategies and surveillance data which can be used to inform obesity prevention initiatives. Many of the examples and success stories listed in this document were conducted by organizations outside of CDC and the federal government and without CDC or federal funding. http://www.cdc.gov/obesity/downloads/CDCHealthEquityObesityToolkit508.pdf Racial and Ethnic Approaches to Community Health (REACH) a national initiative coordinated through the Centers for Disease Control and Prevention to eliminate racial and ethnic disparities in health. Partners are awarded funding to establish communitybased program and interventions designed to eliminate health disparities among African American, American Indian, Alaska Native, Asian American, Hispanic or Latino, Native Hawaiian, and Pacific Islander populations. http://www.cdc.gov/nccdphp/dch/programs/reach/index.htm CDC’s Healthy Communities Program Tools for Community Action http://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/tools/index. htm#rp Step 1: Gathering Data and Assessing Health Disparities. Most, if not all, Section programs were provided, or have conducted activities to develop, materials, tools, and trainings that can be used to initiate this step in the process. These activities, materials, and tools include: Disease burden reports Community assessment/asset mapping Organization infrastructure and capacity assessment Behavioral Risk Factor Surveillance Survey (BRFSS) United States Census data Disease Burden Reports Disease burden reports are facts and figures that estimate incidence, prevalence, mortality rates, and other measures of health outcomes for diseases, frequently based on sociodemographic factors. Tracking disease rates over time is essential in noting differences that Page 17 of 35 may occur after interventions or policy changes have been implemented. Three actions, as provided below, may be useful when investigating disease occurrence. Identify the rate at which disease is occurring by geographic region (state, regional, local): Examining disease occurrence by observing incidence (those who recently acquired the disease) and prevalence (those with the disease at a point in time) can provide helpful information about persons living with a given disease. Mortality rates, which indicate those who have died from a disease, can also be useful when examining chronic disease. Investigating data is the first step towards defining the problem of chronic disease for your program or area of interest (location, population, etc.). Using data from DSHS Vital Statistics Unit, Examples 1 and 2 show the age-adjusted mortality rates for heart attacks and stroke by county in Texas. Example 1. Age-adjusted Heart Attack Rates per 100,000 by Counties, 2006-2010, Texas Example 2. Age-adjusted Stroke Mortality Rates per 100,000 by Counties, 2006-2010, Texas Examine how disease occurrence varies within different population groups in the same geographic area: Determine who is most likely to be affected by the disease. This involves comparing the risk or incidence of the disease among people within the population by specific characteristics (e.g., age, gender, race/ethnicity, disability status). If possible, determine the differences in the rate of the disease between two or more groups (i.e., rate ratio or risk ratio -relative risk). Recognizing and understanding the reasons for these differences will provide greater insight into health disparities, which is important for designing effective interventions and programs. If the underlying reasons for these differences are not apparent, and they are not likely to be, consider what additional questions could be asked, or if the data could be improved/if there are Page 18 of 35 additional data sources that could provide a new perspective. These questions can help gain a better understanding of what the data is telling you, and guide the development of next steps. Compare the burden of disease by locality (within the intervention area): Comparing the burden of disease within an intervention area (public health region, city, municipality, town, etc.) may be limited because of small numbers, and accessing this type of data through traditional surveillance systems may be challenging. In some instances, this information may be reported anecdotally by the public, or by clinicians as "clusters" of disease to public health departments. The data, when available, can be distorted due to factors such as differing age, sex, and race, or even where individuals are seeking care. Make sure to use standardized data or data adjusted for other factors (e.g., age-adjusted, gender-specific) when examining a specific characteristic for comparison. Use this data to target your activities to the area of greatest need, and to develop focused and achievable interventions. Surveillance Systems: Several surveillance (data) systems exist that provide quantitative data on chronic disease. Generally, quantitative methods use standard measures, and data collected is presented in an aggregated format. Quantitative data can also be drawn from other sources, such as one-time surveys, commercial data, and census data. Surveillance data can range from specific disease registries (population or hospital based), to continuous or repeated surveys of representative samples of the population, or aggregate data for recording trends about chronic diseases. Geographic Information Systems (GIS) is a useful tool for visually presenting data by location (e.g., state, region, county or city), and can be used in the identification and illustration of disparate populations in specific localities, and to demonstrate the need for intervention in these specific groups. There are several surveillance data system resources available for using data to address health disparities through a health equity lens. Some commonly used sources are: Vital statistics Disease registries Health surveys Administrative data collection systems US Census data system State-Based Prevention programs It is important when using existing data sources to understand the advantages and limitations inherent these systems. Table 3, below, provides a short overview of this information. Page 19 of 35 Table 3. Strengths and Limitations of Existing Data Systems Data System Vital Statistics Example of Data Morbidity data Disease Registries Cancer incidence, prevalence, and morbidity Health Surveys (e.g., Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavioral Surveillance (YRBS)) Smoking prevalence (cigarette and tobacco use); physical inactivity Administrative Data Collection Systems Hospital discharge data US Census Data System (including the American Community Survey (ACS)) Information on population and housing characteristics (e.g., age, race, education, income, nationality, etc.) State-Based Prevention Programs Tobacco prevention and cessation data (e.g., quit line participation) Strengths Data widely available at local, state, and national level. Data are populationbased and can be used to monitor trends in ageadjusted rates and target areas with high/increased mortality rates. Data increasingly available and includes information on site specific diagnosis (e.g., lung, breast, cervical, prostrate, colorectal, etc.). Monitors trends in risk factor prevalence; the data can be used for program design and evaluation. The data provide information on preventative health practices (e.g., screening for breast, cervical, and colorectal cancers) Data readily available; reflects regional differences in disease hospitalization rates; compare cost information; may have morbidity information Readily available online. Require calculation of rates (available in counts and percentages). Provides important predictors of health status. In 2010, the Census Bureau released the first 5-year estimates for small areas based on 20052009 ACS data. Data may be available at the local level. Detailed information can be collected to aid in designing control programs. Limitations Information on causes of death may not always be accurate without an autopsy or if not clearly stated on death certificate. Information on risk factors is usually not available. Risk factor information is seldom available. Data may be affected by migration patterns of patients between geographic areas, especially in the absence of a robust and comprehensive electronic medical system that shares disease information between clinics or hospitals. Information is based on self-report and may not be representative of the population of interest due to nonresponse rates (e.g., telephone surveys). The data may not be available for some geographic areas unless oversampling occurs. Usefulness is limited by incomplete records, unreliable or invalid coding, and missing clinical variables. Rates may be affected by changing patterns of diagnosis based on reimbursement mechanisms; difficult to separate initial from recurrent hospitalizations. Generally, collected infrequently (every ten years). The ACS is collected every year (population ≥65,000) or every three years (population ≥20,000). May undercount certain populations (e.g., low-income individuals and homeless persons). Data may not be representative of the population at-risk. Require participation by community-based programs or clinician-based systems. Low reporting rates due to non-responsive and passive reporting system. Page 20 of 35 Despite the limitations listed, these data systems can serve as useful sources of information on health disparities. Work with your program’s epidemiology staff, or someone from the State’s surveillance team to access the most current and complete data, then use the data to identify disparate/vulnerable populations, and design and implement meaningful interventions or changes. It is also important to effectively communicate the data or information you gather to local stakeholders. This degree of transparency can result in greater community engagement, the establishment of new relationships, or even additional activities conducted in support of Section initiatives. A list of state resources is provided below as a reference for accessing chronic disease surveillance data. Department of State Health Services (DSHS) Center for Health Statistics provides an access point for health-related data for Texas, and is home to the Vital Statistics Unit, Texas Behavioral Risk Factor Surveillance System (BRFSS). http://www.dshs.state.tx.us/chs/ Texas Behavioral Risk Factor Surveillance System (TX-BRFSS), initiated in 1987, is a federally funded telephone survey conducted on a monthly basis of randomly selected adult Texans to collect data on lifestyle risk factors contributing to the leading causes of death and chronic diseases. BRFSS is a primary source for comprehensive statewide data on preventive health practices and health risk behaviors. http://www.dshs.state.tx.us/chs/brfss/ Texas Youth Risk Behavior Surveillance System (TX-YRBSS), initiated in 1991, is a federally funded classroom-based paper survey conducted biennially on odd years to monitor priority health-risk behaviors that contribute substantially to the leading causes of death, disability, and social problems among youth in the United States. As a primary source for comprehensive statewide data on preventive health practices and health risk behaviors, YRBSS is an important tool for decision-making throughout DSHS, the Texas Education Agency (TEA), and the public health community. http://www.dshs.state.tx.us/chs/yrbs/ Texas Data Center and Office of the State Demographer, in cooperation with a network of affiliates, functions as a focal point for the distribution of Census information for Texas. The Data Center also disseminates population estimates and projections for Texas, as well as other information from the federal government, state government, and other sources. http://txsdc.utsa.edu/data/TPEPP/Index.aspx National data sources may be useful for local needs, as well as for comparing state and local data to national data to determine how better- or worse-off your geographic area is in chronic disease burden and addressing health disparities. Page 21 of 35 County Health Rankings, Robert Wood Johnson Foundation, University of Wisconsin provides information to help counties see where they are doing well and areas that would benefit from making changes to improve health. http://www.countyhealthrankings.org/ CDC Behavioral Risk Factor Surveillance System (CDC-BRFSS) tracks individual health behaviors, such as smoking, alcohol use, sexual activity, exercise, receipt of screenings, diet, obesity, and medication use measures. Data are collected each year and are available at the national and state levels as far back as 1984. http://www.cdc.gov/brfss/ CDC Youth Risk Behavior Surveillance System (CDC-YRBSS) monitors six types of healthrisk behaviors among youth and adults, including unhealthy dietary behaviors and physical activity. They also measure prevalence of obesity among youth and young adults. http://www.cdc.gov/HealthyYouth/yrbs/index.htm CDC Wonder is an array of health related data sets. Each data set can be queried using a series of menus. It is valuable in public health research, decision making, priority setting, program evaluation, and resource allocation. http://wonder.cdc.gov/ CDC State Indicator Reports: Highlights selected behaviors, policies, and environments that affect fruit and vegetable consumption, breastfeeding, physical activity, and child obesity. http://www.cdc.gov/obesity/resources/reports.html Census Data Reports: American FactFinder provides access to data about the United States, Puerto Rico, and the Island Areas. The data in American FactFinder come from several censuses and surveys, including the American Community Survey; American Housing Survey; and the American Economy Survey. Population estimates can also be obtained. Its functions, features, and a help guide are available at the website. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml Qualitative data are data that can be obtained using methods such as focus groups, in-depth interviews, concept mapping, and photo voice techniques where respondents contribute their knowledge and experience to highlight the assets, concerns, and solutions that are important to them for optimizing health. Health disparity data on knowledge and attitudes were collected in specific CTG communities in 2012, and this information is available to interested Section staff through the CTG program. Though this Health Disparities Manual is designed for all Section staff, the CTG disparities research could prove useful for other program staff when examining their own program’s initiatives. The data collected can be used to garner greater insight on how to address health equity based on community members and stakeholders perception of health disparity. Page 22 of 35 Community Assessment A community assessment is conducted to develop an informed understanding of the gaps or needs that exist within a community, and their consequent impacts upon community members. Generally, this type of assessment is conducted to: Identify strengths, weaknesses, and gaps within the State, region, or community; Compile an inventory of the resources currently available within the State, region, or community that can be leveraged to improve the quality of life for residents; Determine service delivery priorities and where those services are most needed; Make decisions about the actions that can be taken to address Statewide, regional, or community needs, and how to use the available assets or resources; Inform strategic planning, priority setting, program outcomes, and program improvements. Below are links to tools for conducting community assessments, including tools that can be used for specific risk factors (e.g., nutrition and physical activity): Community Action Partnership provides basic data on counties and states through an online data retrieval system, and provides a downloadable and editable Microsoft Word document which can serve as the basis for conducting a more detailed comprehensive community needs assessment. http://www.communityactioncna.org/ Community Assessment Toolkit: Nutrition and Physical Activity is used to develop programs and services that address the nutrition and physical activity needs and wants of a community. http://healthvermont.gov/local/grants/documents/CommunityAssessmentToolkit.pdf Community Assessment Toolkit: Walk Friendly Communities serves to both recognize existing walkable communities, and to provide a framework for communities seeking to improve their walkability. http://www.walkfriendly.org/WalkFriendlyCommunitiesAssessmentTool.pdf Links to resources provided below contain information on community factors that may affect health disparities: Healthier Food Retail: Beginning the Assessment Process in Your State or Community provides a summary of state, county, and municipal data available to assess access to healthy retail foods. http://www.cdc.gov/obesity/downloads/HFRassessment.pdf Good Health Counts is a report that focuses on indicators associated with community factors, and how indicator report cards can support community efforts to improve health. http://www.preventioninstitute.org/component/jlibrary/article/id-85/127.html Page 23 of 35 Organization Infrastructure and Capacity Assessment While conducting organization resource or asset mapping, you will identify gaps in program staff knowledge, skills, and resources for addressing health disparities. It is also useful to conduct a SWOT (Strengths, Weaknesses, Opportunities, and Threats) analysis to identify the strengths and weaknesses of your program (S-W), and the opportunities and threats that exist in the external environment (O-T). Developing awareness of your organization or program’s current status as it relates to health equity and health disparities can help with both strategic planning and decision-making. You can use the information gleaned from the SWOT analysis to identify gaps in staff and program knowledge, skills, and resources. It may be important to conduct surveys, interviews, or focus groups to follow-up and/or determine your staff’s level of confidence and competence in addressing health disparities in the work that they do, their overall level of cultural competence, and their ability to work with diverse populations. New staff should be encouraged to participate in trainings to increase their understanding of health disparities and equitable mechanisms for addressing them. Annual refresher courses should also be required for existing staff. A wealth of resources that can help facilitate improvement in knowledge and skills related to health inequities can be found at CEDD’s website: https://www.hhsc.state.tx.us/hhsc_projects/cedd/services-resources.shtml If Section or program staff members have not attended a Courageous Conversation workshop on health equity conducted by CEDD, ask leadership for information on how you can access this useful resource for building your staff capability to address health disparities in your community. Here are several links to additional resources that are available online: Unnatural Causes: "Is inequality making us sick?” is a seven part documentary series with an associated toolkit and discussion guide about health equity that is useful for the lay-person and public health professionals alike. http://www.unnaturalcauses.org/ Why Place and Race Matter, produced by PolicyLink and the California Endowment, examines how environmental factors can be strengthened to benefit the health of all communities. http://www.policylink.org/atf/cf/%7B97c6d565-bb43-406d-a6d5eca3bbf35af0%7D/WPRM%20FULL%20REPORT%20(LORES).PDF Promoting Health Equity: A Resource to Help Communities Address Social Determinants of Health is a CDC-published workbook designed for public health practitioners and partners interested in addressing social determinants of health to promote health and achieve health equity. http://www.cdc.gov/nccdphp/dach/chhep/pdf/sdohworkbook.pdf Tackling Health Inequities Through Public Health Practice: A Handbook for Action raises questions and provides a starting point to assist health practitioners in considering the potential for reorienting public health practice to address the root causes of health inequities, particularly with respect to restructuring the organization, Page 24 of 35 culture, and daily work of public health. http://www.naccho.org/topics/justice/upload/NACCHO_Handbook_hyperlinks_000.pdf Common Health Action (CHA) Training and Health Disparities Curriculum Though specifically designed for CTG sub-awardees' staff and coalition members, the health disparities training provided by CHA as part of the technical assistance provided through CTG state office is an excellent resource for learning more about health disparities and health equity. If appropriate and available, Section staff can utilize this resource in order to gain a common language surrounding health equity; to understand the social determinants of health; identify and engage stakeholders and community members on the topic of health disparities; and build and maintain effective coalitions to achieve health equity. The curriculum can be used as a companion to this guidance document for advancing your efforts to achieve health equity. Step 2: Using Health Data to Inform Programmatic Activities in Target Communities or Populations When using chronic disease disparities information collected in step 1 to select/design intervention strategies, it can be beneficial to characterize high-risk population into subgroups that may respond differently to specific intervention strategies. This characterization can be done, by demographics, socioeconomic status, health care access, health knowledge and attitudes, potential or actual exposure to chronic disease risk factors, or media use patterns. If this information is not readily available through secondary or existing data sources, the data can be collected from or through key informant interviews, focus groups, or surveys. In public health regions or communities with multiple and/or overlapping disparate conditions, you should aim to reach the most underserved population. Programs can work with state, regional, and local partners to prioritize and streamline intervention strategies for the targeted areas and for the subpopulations that are most likely to be affected by your program’s chronic disease. This will allow the development of comprehensive approaches to address the economic, social, and political roots of health and illness. Determine the appropriateness of intervention possibilities for achieving program objectives, including access to and ability to influence members of the at-risk subpopulations, current level of health activity, potential support for change, and barriers to change. Specific subgroups of the population may also be strongly influenced by community leaders, organizers, or other organizations who serve as gatekeepers (e.g., pastors, parent-teacher liaisons, etc.) to accessing your target population. These community leaders may operate through different intervention channels (e.g., schools and churches), so working with them to identify effective strategies for addressing the risk factors and social determinants identified as risk factors will increase the likelihood of your program’s success. Page 25 of 35 Step 3: Developing Multi-Sector Partnerships/Coalitions Actions to eliminate health disparities will require a sustained effort by public, private, regional, and local stakeholders, with a focus on making systems-level changes. If your program is seeking to implement a community-based intervention, research indicates they are best carried out by residents and local advocates for change. It is important to look beyond traditional partnerships, and reach across sectors for partners to create systems and environmental change(s) to reduce chronic disease health disparities. Ensuring that program staff and, as appropriate, legislative councils are representative of diverse sectors, as well as different racial, ethnic, and other groups is one way to strengthen this. Include partners, such as city planning departments, public works, park and recreation, transportation, and others who can actively participate in community-based interventions when developing activities. Likewise, consider engaging community champions, schools, local companies (e.g., grocery/food store chains), private sector organizations, hospital/medical centers, and foundations. These non-traditional partners have a vested interest in the community, and can assist in leveraging resources and building and maintaining local coalitions. Building and maintaining coalitions and councils is a helpful process when implementing community-based interventions, as well as engaging statewide stakeholders. These coalitions or councils can create alliances of partners or organizations who are willing to work together to achieve a common goal or purpose and are composed of individuals who are passionate about their cause. Ensure that the coalition includes the necessary partners, address pertinent health issues and implement strategies that meet the needs of the target population. An added benefit is that coalition/council participants can provide direct access to intervention channels within a community, including but not limited to, the health care systems (e.g., community clinics and local hospitals), churches, schools, businesses and worksites. Councils/coalitions can also provide opportunities to involve other community organizations and strong representatives for effecting change in areas that have traditionally been difficult to reach through mobilizing the human resources needed to plan and implement culturally-sensitive community-based interventions. The partnership developed can be used to: Increase the effectiveness and strength of program strategies by helping stakeholders raise awareness, strengthen local stewardship, improve health outcomes, foster cultural competency, and facilitate the collection and diffusion of data and evidence/practicebased strategies. Guide stakeholders at the state, regional, and local levels to adopt the most effective goals, strategies, and action steps for successful outcomes. In their 2003 article, Merzel and D’Afflitti21 found that simply having a community advisory board did not increase program success. The ability to choose which issues should be addressed by the group, rather than just implementing strategies for topics that were pre-selected, was an 21 Merzel, C. and D’Afflitti, J. (2003). Reconsidering Community-Based Health Promotion: Promise, Performance, and Potential. Am J Public Health. 93(4): 557-574. Page 26 of 35 important predictor of success and continued engagement of the group. When attempting to engage stakeholders, it is important to keep this in mind if a program is to be successful. Step 4: Applying Best Practices to Intervention Strategies Understanding unique worldviews, priorities, social expectations, and cultural norms within communities or segments of a target population is important for designing or modifying interventions that fit the specific needs of any group. Determine if similar programs exist in the region or community where your program is working, and examine the possibility of expanding on these programs and increasing collaborations, rather than creating new projects that may exhaust community resources and/or hinder full participation and acceptance of your program. Develop and implement community-based approaches that target the whole population while focusing on higher-risk groups to reduce health disparities. This community-wide approach addresses both high-risk individuals within the community, and prevents the proliferation of the health condition over time. Work with the community to examine, prioritize, and implement multi-level intervention activities that can effect wide-spread change, enhance impact, and maximize reach. Full, authentic partnerships between your program, health professionals, community champions, and local residents can influence broader economic, social, and political forces. Participation of community members in this process will provide a more accurate assessment of interventions that are best suited for the community, and provides access to available resources to supplement grant funding and pursue sustainability. Ensure that the system-level changes implemented are informed by traditional best-practices and cultural and societal norms of the community for wide-spread and long-term improvement of health. Upon identifying these best practices, work through local stakeholders and organizations to ensure that they are implemented properly. Program staff and councils/coalitions can engage community members and leaders in creating healthier communities by: Hosting workshops/seminars at convenient locations in the community (e.g., schools, libraries, community centers, churches, etc.) to discuss health disparities within the community; advocating for more sidewalks, bike lanes, walking trails, parks, and recreation facilities; encouraging workplaces to promote wellness activities and create tobacco-free campuses; encouraging local schools, workplaces and assisted living facilities to provide healthier foods and beverages; encouraging farm to school and farm to work programs to increase access for fresh fruits and vegetables; asking neighborhood supermarkets and convenience stores to provide fresh fruit and vegetables to the public and local food banks; asking local restaurants to provide healthy menu options; Page 27 of 35 working with farmers’ markets and local HHSC offices to accept food stamps/SNAP benefits; and working with local universities and organizations to collect and track data about health disparities and monitor changes over time. Examples five through eight illustrate best practices used in to implement strategies for tobacco-free living (schools); worksite wellness; and healthy eating (a food hub, implementation of menu labeling in local restaurants). Example 5. Tobacco-free Living As a result of Youth Risk Behavior Survey results, South Carolina’s School Board Association partnered with CDC and the South Carolina Department of Public Health and Environmental Control to develop comprehensive smoke-free policies to be implemented on campuses statewide. Roundtables were held throughout the state in 2009 and 2010, giving school board members, school district employees, health department staff, local government and elected officials, and community-based organizations an opportunity to discuss existing policies and successful strategies for adopting and implementing the newly created policies. Through CDC funding, a School Health Policy coordinator was hired to facilitate this focus on policy change and promotion. In early 2009, only 22% of South Carolina school districts were in compliance with the new comprehensive tobacco-free schools policies. Upon completion of the roundtables, this number improved to 35%. In the year after completion, 58% of schools had 100% tobacco-free campus policies, though not all had completely implemented the comprehensive policies. The collaboration between the School Board Association, CDC, and Department of Public Health and Environmental control is expected to continue conducting roundtables to increase community awareness of the policies and increase the number of schools meeting the guidelines. Source: http://www.cdc.gov/healthyyouth/stories/pdf/2010-11/success_1011_sc.pdf Page 28 of 35 Example 6. DELL Computers’ “Well at Dell” worksite wellness program The comprehensive wellness program provides an on-site physician, 24-hour access to a nurse hotline, individual health coaching, online health management programs, an on-site fitness center, and cafeterias offering healthy food options. In 2009, about 40% of Dell’s Texas employees participated in the “Well at Dell”. In addition to the benefits described above, the program also uses health risk assessments and insurance claims to gauge employee health risks. When obesity was determined to be a major health risk and cause of increased insurance claims, Dell developed a strategy for their on-site cafeterias to account for this: healthy foods are usually less expensive than unhealthier options, baked goods are less expensive than fried foods, and bottled water was priced lower than soft drinks. These are just some of the ways in which Dell made small changes to make a big impact on employee health. In mid-2009, 83% of employees using the health coaching benefit of the wellness program reported reduction or elimination of at least one health risk, 71% of all program participants eliminated or lessened high blood pressure risks, and 56% met recommended physical activity goals. The “Well at Dell” program also includes a Cardiac Management Program that showed positive results for participants: 86% improved cholesterol levels, 88% improved LDL cholesterol levels, 72% reported increased exercise, and 64% reported meeting BMI goals or at least making improvements toward meeting these goals. Source: Dell Inc.: Tre McCalister, global benefits manager, Dell Inc.; and National Business Group on Health, “Well at Dell: Creating a Campus Culture of Employee Health,” Platinum Awards: Best Employers for Healthy Lifestyles 2009 (2009), pp. 1-4.Summary accessed from http://www.window.state.tx.us/specialrpt/obesitycost/work.php#114 Example 7. San Antonio Healthy Restaurant Coalition, ¡Por Vida! A partnership between public health organizations, food-industry professionals, registered dieticians, and other stakeholders, the San Antonio Healthy Restaurant Coalition (HRC) was formed. The HRC began the ¡Por Vida! initiative in 2010 to promote healthy selections to restaurant patrons and move forward in the fight against obesity. Sub-committees of the HRC were assigned to develop health menu item criteria based on national guidelines, create a logo and marketing plan, and find restaurants willing to participate in the project. The first phase of the program involved seven restaurant brands with a total of 75 locations, with an additional five restaurants joining after the initial wave. Working with registered dieticians, the restaurants evaluated and changed existing menu items to meet the criteria established by the HRC. A pilot project was conducted to evaluate changes made to the children’s menu of a local Mexican-food restaurant. Results of the pilot showed that overwhelmingly, restaurant patrons liked the look of the redesigned menu, and that 65% chose a healthy item on the menu. Of those individuals, nearly 84% reported that the logo, identifying that the item was healthier, helped in their decision-making. Nearly 97% reported that they were satisfied with the portion size, and 98.4% of children liked the taste of the food. Source: Biediger-Friedman L, Sosa ET, Shields K,& Shutt A. A voluntary approach to improve menu options in restaurants through a local collaborative partnership. (2014). Texas Public Health Journal, Vol 66, Issue 1, Winter 2014. Page 29 of 35 Example 8. Azle Food Hub, part of the Community Transformation Grant Below is an example of a flyer advertising a food hub in Azle, Texas. Additional information on the initiation of this project and more resources can be found at http://www.texashealth.org/food-hub-produce-program Source: http://www.texashealth.org/workfiles/THAZ/LLT/Parker_County_Food_Hubs.pdf Page 30 of 35 Step 5: Developing Culturally and Linguistically Appropriate Messages Cultures throughout the state are different, and each target population’s cultural norms and practices should be assessed before developing educational materials and media campaigns. It is important to understand how individuals of a particular group perceive, think, interact, behave, and make judgments about their community and health. Across cultures, some words and phrases are used in different ways, so effective communications with a community, should include presenting information in the most culturally and linguistically relevant manner. Some points to remember when framing these messages include: Examine the cultural implications and relevance of messages and written materials; ensure that messages and written materials developed will benefit the target population; ensure uniformity of messages and written materials; use culturally competent and appropriate language and images; pursue publicity and advertising in population-specific media outlets (e.g., local and culture-specific newspapers, and radio and television programs); ensure that program staff, stakeholders, and/or coalitions review all media messages for cultural and linguistic appropriateness before they are publicized; and consider modifying messages if the community response is negative, or the message does not produce the intended result(s). The Robert Wood Johnson Foundation Commission to Build a Healthier America is an excellent guide on developing appropriate messaging: http://www.rwjf.org/en/aboutrwjf/newsroom/features-and-articles/Commission.html Step 6: Evaluating Programmatic Processes and Outcomes The evaluation process should begin during the initial planning stages of your program’s activities. Objectives should be specific, measurable, achievable, and realistic, as well as attainable within a specific time frame (SMART), see Example 10. This process should be followed by designing and implementing activities aimed at addressing health disparities for each objective. During the evaluation process, program staff should ensure that the activities and anticipated outcomes of the interventions are also practical for the intervention/target population. Page 31 of 35 Example 10. Ensuring that evaluation criteria are consistent with goals, objectives, and activities Multi-Year Goals are general broad intentions, usually intangible that a program desire to achieve. Here are some examples that may be applicable to the CTG project: Increasing access to opportunities for physical activity in rural areas of the community Creating safer routes to school communities with no sidewalks or pedestrian crossings Providing access to healthy food options in underserved neighborhoods Annual Objectives are usually narrower than goals and provide precise and concrete ways of reaching/obtaining intended outcomes. Some examples for the CTG project may include: By September, 2014, establish three (3) joint use agreements to increase physical activity in x community for at least 200 residents in Starr County. Support the construction of walkable and bikeable lanes to access two elementary schools in x community, within Webb County by September 29, 2014. Work with at least two (2) local farmers to establish food stands in x community that contain more than 80% of WIC recipients by September 29, 2014. Activities are actions that take place when planning and implementing the system and/or environmental change program, which includes: Building and maintaining coalitions - engaging community for action Increasing awareness through earned media and media campaigns Organizing farmers' markets, farm-to-schools/work and community gardens Organizing/supporting changes to infrastructure (e.g., creating bike lanes, pedestrian crossing, parks and walking trails) Encouraging tobacco-free worksites through implementation of worksite wellness programs Outcomes are results or changes in communities, organizations, or systems. These include: Intermediate outcomes such as development of coalitions and community taskforce Longer Term outcomes such as changes to the infrastructure, programs, and environment (e.g., passing of county-wide/state-wide tobacco-free ordinances) Public Health Impacts, including the cost effective achievement of population level improvements in overall health status and equitable distribution of improvements across population subgroups. It is important when planning and evaluating programmatic activities, to facilitate continuous collaboration between partners and stakeholders for ongoing data collection. Program staff should access tools that can help them evaluate system-level changes. The tools used should answer questions similar to these: Were the desired system and/or environmental changes achieved? If not: o Which strategy (ies) and/or activity (ies) need to be revised or modified? o Who else at the statewide, regional, and/or local level should be involved to achieve the desired system/environmental change? Did the desired system/environmental change benefit the community? How? o If not: Should these evidence-based practices be modified to better suit the community and achieve the desired outcome? Page 32 of 35 How can local coalitions gain community support or influence decision makers to achieve the desired system/environmental change? Step 7: Disseminating Best Practices Program staff should envision ways in which to document and share intervention strategies that produce successful (i.e., effective and impacting) outcomes in target population. This is essential, given that, due to limited funding, replication of program activities cannot always be accomplished one by one throughout the state. The Section as a whole may consider adding to this toolkit a “best practices” section, designated by geographic area (i.e., urban, rural, frontier, and border) with this information. The assumption made from this approach is that geographically identical communities will have similar infrastructure, resources, and capacity to carry out these programs. Other strategies may be to consider using demographic characteristics (e.g., racial/ethnic composition and/or gender distribution), the magnitude/prevalence of disease, or using disease morbidity data to determine similarities between localities. The outcomes of interventions, including success stories, should also be promoted through local and other media channels, at regional, state and national conferences and seminars and publish on statewide websites (e.g., Love Live Texans) and in peer-reviewed journals. Step 8: Sustaining Practice-Based Interventions During this step, Section and program staff should plan for sustainability of interventions to eliminate chronic disease disparities. Staff should start by creating a sustainability plan for an intervention at the beginning of the planning process. Through building and maintaining local partnerships (as described in Step 3), staff should collaborate with multi-level stakeholders to meet and strategize about funding, and identify champions to address health disparities at the systems and community level long after the initial program/project funding has ended. Sustainability is not just achieved by maintaining project funding; rather, it is achieved by creating and enhancing community commitment to change, and by streamlining, prioritizing, organizing, and maximizing community assets and resources. Stakeholders should be encouraged to institutionalize policies and practices within local communities and organizations. Involving local participation in the planning and prioritizing of project activities (step 2) should be the first phase in getting community buy-in for all Section programs. Local participation will facilitate community ownership of the interventions, and may provide better access to target population leaders, and ultimately influence long-term changes in the community. In addition, local participation shapes the interventions, facilitates cultural sensitivity, and ensures that the intervention is adoptable to the norms and values of the community. Stakeholders on a more local level can play a key leadership role by becoming involved in implementing the intervention through offering vital services (e.g., healthcare providers, community health workers, local farmers and grocery store owners), coordinating local participation, or Page 33 of 35 empowering decision makers to make lasting systems and environmental changes. Involving community-based organizations, schools, universities, churches, faith-based and philanthropic organizations, as well as social, civic, and professional clubs, businesses, and media/communication organizations can strengthen community contribution and facilitate long-term maintenance of practice-based interventions. The following links are for additional resources for developing sustainability plans. CDC's Sustainability Planning Guide for Healthy Communities is a synthesis of scienceand practice-based evidence designed to help coalitions, public health professionals, and other community stakeholders develop, implement, and evaluate a successful sustainability plan. The Guide provides a process for sustaining policy strategies and related activities, introduces various approaches to sustainability, and demonstrates sustainability planning in action with real-life examples. http://www.cdc.gov/healthycommunitiesprogram/pdf/sustainability_guide.pdf Washington University’s Center for Tobacco Policy Research (CTPR), The Sustainability Framework and Toolkit. The Sustainability Framework outlines eight domains that are critical to a program’s capacity for sustainability. The Program Sustainability Assessment Tool provides public health, clinical care, and social service programs and their partners with a reliable way to measure their capacity for sustainability. Users assess their program’s current capacity across a range of specific organizational and contextual factors. The program is given an overall sustainability score as well as a composite score for each domain. The tool can be used with national, state, and local level programs. http://cphss.wustl.edu/Projects/Pages/Sustainability-Framework-and-AssessmentTool.aspx The following link is for article on planning for the sustainability of community-based health programs: conceptual frameworks and future directions for research, practice and policy. http://www.ncbi.nlm.nih.gov/pubmed/10178339 Summary This document was designed to provide information on the planning process for developing and enacting systems and environmental changes that will eliminate chronic disease health disparities and achieve health equity. It outlined and provided examples of the following steps for implementing these changes: Gather data to assess health disparities in target communities Use health disparities data to inform programmatic activities Develop multi-sector partnerships Apply best practices to intervention strategies Develop culturally and linguistically appropriate messages Evaluate processes and outcomes Disseminate best practices Page 34 of 35 Sustain interventions Taking action to eliminate chronic disease health disparities starts with defining the burden of chronic diseases and assessing existing population-based strategies to address them. It is important to use population-based strategies to increase public awareness of the signs and symptoms of chronic diseases, and identify culturally appropriate approaches to prevent chronic disease disparities among racial, ethnic, and other disparate populations. It is critical to continually engage the community in each of these steps to ensure the cultural competence of your program’s health disparity efforts, and to attain successful project implementation and long-term sustainability. Ultimately, everyone benefits when communities are structured to facilitate healthy and active living and provided the opportunity to enhance the health and long-term development of their residents. Eliminating health disparities could result in healthy and productive adults that boost workforce capacity and capability, reduced reliance on healthcare and other support systems because adults will have healthy options and are able to make better decisions to improve their health, and a strengthening of local infrastructure and overall economy. To increase the likelihood of achieving chronic disease health equity through systems and environmental changes, Section and program staff must continually assess, refine, implement, monitor, and evaluate their strategies for addressing chronic disease. Continued utilization and updating of this document and the Toolkit as a whole will contribute to the Section’s goal of coordinating efforts between communities, coalitions, and stakeholders to support and sustain an environment that makes possible a whole and healthy Texan. Page 35 of 35