here - Urban Communication Foundation
advertisement
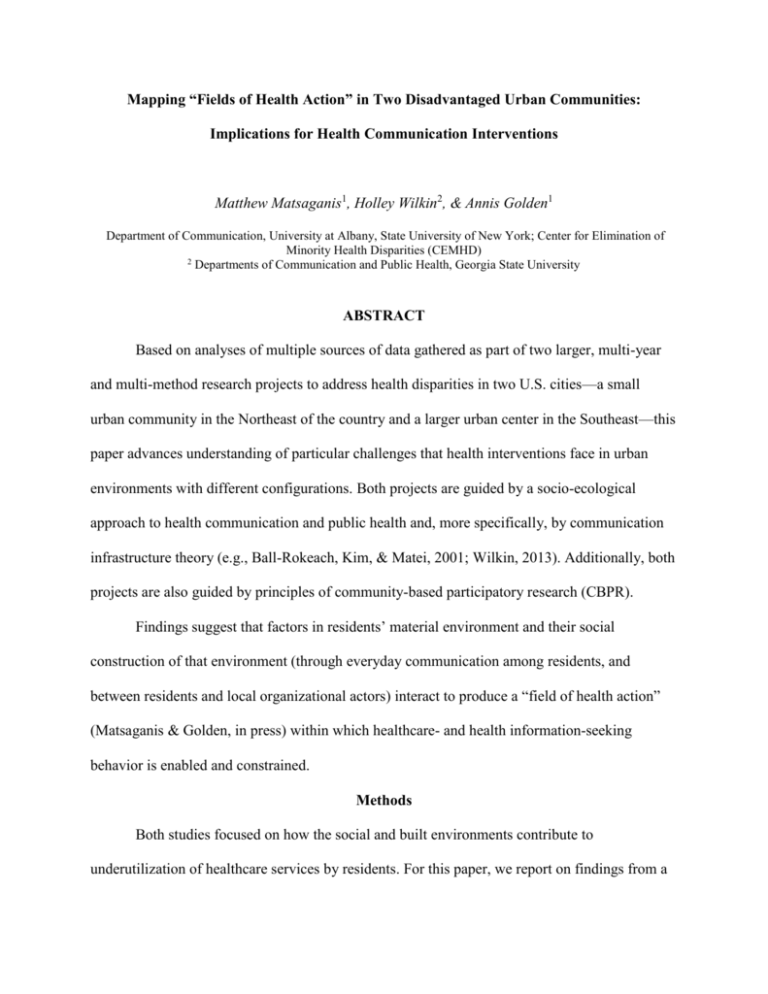
Mapping “Fields of Health Action” in Two Disadvantaged Urban Communities: Implications for Health Communication Interventions Matthew Matsaganis1, Holley Wilkin2, & Annis Golden1 Department of Communication, University at Albany, State University of New York; Center for Elimination of Minority Health Disparities (CEMHD) 2 Departments of Communication and Public Health, Georgia State University ABSTRACT Based on analyses of multiple sources of data gathered as part of two larger, multi-year and multi-method research projects to address health disparities in two U.S. cities—a small urban community in the Northeast of the country and a larger urban center in the Southeast—this paper advances understanding of particular challenges that health interventions face in urban environments with different configurations. Both projects are guided by a socio-ecological approach to health communication and public health and, more specifically, by communication infrastructure theory (e.g., Ball-Rokeach, Kim, & Matei, 2001; Wilkin, 2013). Additionally, both projects are also guided by principles of community-based participatory research (CBPR). Findings suggest that factors in residents’ material environment and their social construction of that environment (through everyday communication among residents, and between residents and local organizational actors) interact to produce a “field of health action” (Matsaganis & Golden, in press) within which healthcare- and health information-seeking behavior is enabled and constrained. Methods Both studies focused on how the social and built environments contribute to underutilization of healthcare services by residents. For this paper, we report on findings from a thematic analysis of qualitative data collected as part of each of the research projects (interviews, focus groups, community forum discussions, as well as ethnographic field observations). In the community located in the large Southeastern city, 52 community members (14 male and 38 female; 12 were 18-35 years old; 30 were aged 36-64; 10 were 65 and older) participated in 2-2.5 hour community forum discussions. Additionally, 32 semi-structured interviews were conducted with healthcare workers at 1) a public hospital, 2) community clinics associated with the hospital, and 3) a federally qualified health center located within the community. Questions were designed to determine factors contributing to primary healthcare access disparities. In the case of the smaller urban community in the Northeastern U.S., we draw on 105 semi-structured interviews conducted with 89 unique female attendees at 18 community health education events. Participants reported a median age of 49; 65% identified as African American (or as African American and some other ethno-racial group); 28% identified as White; 6% as Latino/a or Hispanic, and 1% as South Asian. We also draw on in-depth, semi-structured interviews with staff members of local CBOs (N = 20, representing nine CBOs). Researchers from the two projects identified the “field of health action” characteristics that emerged from their respective projects. We compared and contrasted our general findings and accounted for differences in the focus of the two projects that could influence a more finegrained analysis of the available data across both sites, interpretation, and conclusions. Subsequently, researchers from both projects engaged in a more systematic analysis of the data. Findings & Conclusion Four factors related to the “field of health action” of residents in both cities emerged as salient from our analysis: (1) actual availability of and perceptions of access to health resources, (2) transportation options, (3) communication resources (including interpersonal, media, and organizational) that aid health information and healthcare seeking, and (4) privacy concerns around healthcare-seeking. In discussing these factors, we highlight differences across the two urban communities studied. Overall, our findings show how a city’s built and social environment, as well as policies that shape everyday life at the local level impact residents’ health. We also offer recommendations as to how to improve the design of public health strategies, health communication campaigns, and policy interventions aimed at improving health outcomes and reducing health disparities in residential community contexts. References Ball-Rokeach, S. J, Kim, Y. C., & Matei, S. (2001). Storytelling neighborhood: Paths to belonging in diverse urban environments. Communication Research, 27, 392–427. doi:10.1177/009365001028004003 Matsaganis, M. D., & Golden, A. G. (in press). Interventions to address reproductive health disparities among African American women in a small urban community: The communicative construction of a “field of health action.” Journal of Applied Communication Research. Wilkin, H. A. (2013). Exploring the potential of communication infrastructure theory for informing efforts to reduce health disparities. Journal of Communication, 63, 181–200. doi:10.1111/jcom.12006