Myofascial Medicine Where are we now? Where should we be going?
advertisement
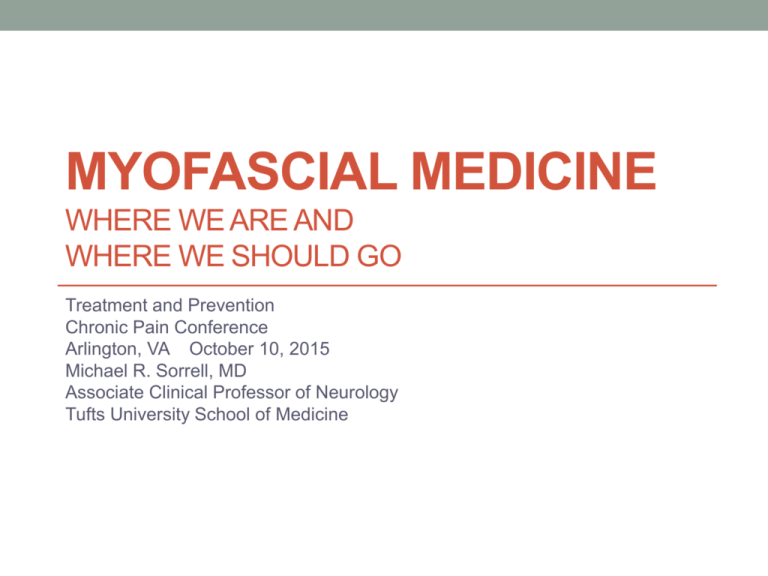
MYOFASCIAL MEDICINE
WHERE WE ARE AND
WHERE WE SHOULD GO
Treatment and Prevention
Chronic Pain Conference
Arlington, VA October 10, 2015
Michael R. Sorrell, MD
Associate Clinical Professor of Neurology
Tufts University School of Medicine
The University of Minnesota requires financial disclosures from
the lecturer and the spouse of the lecturer
Michael R. Sorrell, MD
• Journal of
Musculoskeletal Pain:
Editor-in-Chief
• All illustrations are in
the public domain
Spouse
• None. She discloses
she is fed up with the
lecturer not having
other financial
disclosures.
Proposed definition:
Myofascial Medicine
• is a medical specialty
• concerned with the diagnosis and treatment of pain and
other symptoms
• caused by disturbance of myofascial trigger points,
• [hyperirritable spots in skeletal muscle or in the fascia
associated with skeletal muscle].
• Myofascial pain occurs regionally in all parts of the body;
it can cause symptoms of or can be caused by
disturbances of nerve, bone, viscera, cranial and
intracranial structures.
Trigger Points
• Trigger Points (TrPs) are hyperirritable and electrically active
•
•
•
•
spots in muscles and ligament.
Pressure on these TrPs will cause enough discomfort to cause
the patient to jump or wince (Jump Sign) and/or notice pain or
numbness at a location at a distance from the area pressed
(Referred Pain).
TrPs are nodules usually located in Taut Bands of muscle.
When a taut band is stimulated, i.e. plucked or strummed, it
often contracts, causing a local twitch response, which is a
spinal reflex. TrPs are less frequently located in tendons.
Pressure on Active TrPs replicate the patient’s symptoms and
pressure Latent TrPs do not.
Myofascial Pain can mimic radiculopathy, migraine aura,
boney, abdominal, cardiac pathology, and other symptoms.
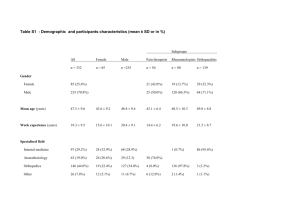
Myofascial Pain: Demographics
Simons DG, Chapter 1 in Travell & Simons’ Myofascial Pain and Trigger Point Dysfunction,
the Trigger Point Manual,,2nd ed, 1999; Williams & Wilkins, Baltimore
• 50% of young adults have Latent TrPs in the shoulder;
•
•
•
•
25% have referred pain
Similar frequency in the masticatory muscles
28% had pain in the temple, 33% in splenius capitis, 33%
in upper trapezius
In an Internal Medicine practice, 29% complained of pain;
30%of these were myofascial
In a Comprehensive Pain Clinic, a neurologist found 93%
of the patients had some part of their complaint from TrPs
and 74% were primarily caused by active TrPs
The Examination of Myofascial Pain
• Find the taut band
• Press where the patient says the pain originates
• Enough pressure to blanche the fingernail (at least 4
Kg/cm)
• Reproduce the patient’s pain
• Identify secondary sites in the referral pattern and in the
same muscle
• Press 5-15 seconds to provoke secondary phenomena,
e.g. ipsilateral blurred vision, lightheadedness
Examples of Referred Pain from
Myofascial Trigger Points
Diagnosis of Myofascial Pain
• Replicate the patient’s symptoms by pressing on the
trigger points
• Use the physical exam to determine if the trigger point is
secondary to disease elsewhere ( a primary source) or is
primary from no other cause.
• If the trigger point is primary, send the patient for physical
therapy featuring stretching of the involved muscles along
their lengths. If this worsens the symptoms, re-evaluate
for a primary source.
Janet Travell, MD
David G. Simons, M.D
MYOFASCIAL MEDICINE:
WHAT GOOD IS IT?
Case report
Back pain in the Emergency Room (1)
• 39 y.o. 7 month pregnant mother 2 picks up her 4 y.o. son
from a chair and has the sudden onset of severe left low
back pain radiating to the buttock and upper thigh.
• After lying flat on the floor for 1 hour, she goes to the local
university affiliated hospital in suburban Boston, where
she reports 9-10/10 level pain.
Back pain in the Emergency Room (2)
• After evaluation by the ER physician, Ultrasonography
shows no problem with the pregnancy
• Plans are made for an MRI the next day to rule out an
acute herniated nucleus pulposus and for overnight
admission. An orthopedist is consulted.
• The patient calls in a neurologist from another city, who,
10 hours after onset of pain, finds that pressure on the left
L4 paraspinal musculature reproduces her symptoms.
The patient has an antalgic gait but no other abnormalities
on examination.
Back pain in the Emergency Room (3)
• The patient says, “Dad, nobody examined my back the way
•
•
•
•
that you did. Nobody even touched it.”
The neurologist demonstrated the physical findings to the ER
attending and suggested injecting 1% Lidocaine into the
tender area would probably resolve the pain, eliminating the
need for hospitalization and the MRI.
The ER room MD demurred, explaining she was not trained in
such a technique, and would not perform it even if the
neurologist talked her through it.
The anesthesiologist on-call refused to consider performing a
lidocaine block, since she was not Pain Fellowship trained.
The neurologist called a neurologist friend on the hospital
staff to ask if he would perform a nerve block. He demurred,
explaining he did not perform injections at all.
Back pain in the Emergency Room (4)
• The patient was admitted to the obstetrics ward. She was
•
•
•
•
given Tylenol III
At 06:30 the next AM, the neurologist walked the patient
down the corridor to the nurses’ station. She felt well
enough to go home.
The orthopedics consultation was cancelled.
The nursing staff applauded, since they had seen similar
patients with acute back pain.
The patient had follow-up care with a physical therapist
familiar with the treatment of myofascial pain. Symptoms
resolved in 5 days.
MYOFASCIAL MEDICINE:
WHAT GOOD IS IT?
Pilot Study
Myofascial Examination Leads to Diagnosis and
Successful Treatment of Migraine Headache
Sorrell MR, Journal of Musculoskeletal Pain, 2010. 18: 31-37.
• 49 patients with
• 23 of 23 (100%) of
Migraine
Migraine Without Aura
• All given Myofascial
• 5 of 11(45%) of
Exam
Migraine With Aura
• % whose migraine
• 15 of 15 (100%) of
headache pain could
Chronic Migraine
be reproduced by the
exam
Myofascial Headache study
2
• Effect of Physical Therapy with stretching involved
muscles along their lengths (PTS)
• Global scale of self-improvement in %
• % = or >50% improvement in a group (vs. no PT)
• Group improvement %
Myofascial Headache 3
• Migraine without Aura: 11 of 13 treated had 50% or >
improvement (85%) [group improvement 64%], 0 of 5 not
treated with PTS = or >50%, p=0.01.
• Chronic Migraine: 5 of 6 treated had 50% or >
improvement (86%) [group improvement 72%], 1 of 5
without PTS had 50% or > improvement {fentanyl patch}
(20%) [group improvement 10%],p=0.0004.
What do we know about the Trigger Point?
• Heisenberg uncertainty principle: the more precisely the
position of some particle is determined, the less precisely
its momentum can be known
• Biologic variant of the Heisenberg uncertainty principle:
disturbing tissue by using instruments to study one
manifestation of a structure will probably alter another
manifestation of the structure.
The Trigger Point is electrically different
from other muscular tissue:
Spontaneous Electric Activity
The Trigger Point is biochemically different from other
muscular tissue
Altered Biochemistry of the Trigger Point
Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local
biochemical milieu of human skeletal muscle. J Appl Physiol. 2005; 99: 1977-84.
Higher in Active TrPs
(no change in normal
muscle and in Latent
TrPs):
• Bradykinin
• CGRP
• Substance P
• TNF α
• Interleukin 1β
And Reduction in pH
• Serotonin
• Norepinephrine
The Trigger Point has different material properties
than other tissue: sonoelastography shows it is stiffer
The Trigger Point has blood supply
The Trigger Point has its own theory of energy supply
But what is the anatomic structure of the Trigger Point?
Muscle fibers slide in and out of each other when
they contract and release
Spontaneous electrical activity comes from end plate
zones in the muscles
Buchtal F, Rosenfalck M. Spontaneous electrical activity of human muscles. Clinical Neurophysiology
.
1966; 20: 321-336
Motor end plate pattern in muscle
(nerve fiber in green, acetylcholine in red)
Or is the Trigger Point a Muscle Spindle?
Partanen JV, OjalaTA, Arokoski JP. Myofascial syndrome and pain: a neurophysiological approach. Pathophysiology
2010; 17: 19-28.
Tissue specimens look like Muscle Spindles
Normal Anatomy of a Muscle Spindle
Muscle Spindle in Myofascial Pain
David Hubbard, M.D., Hubbard Foundation website, 2011
MYOFASCIAL MEDICINE
Where we are
Trigger point injections for headache disorders: expert
consensus methodology and narrative review.
Robbins M, Kuruvilla D, Blumenfeld A, Charleston L 4th, Sorrell M, Robertson CE,
Grosberg BM, Bender SD, Napchan U, Ashkenazi A.
Headache, 2014. 54: 1441-59.
• 2014 Headache
Member’s Choice
Award
• Brick Cox, illustrator
Trigger Point Treatment Options
• 3,060,000 results on
• Trigger Point injections
Goggle in 0.41 seconds
(September 14, 2015)
• Myotherapy
• Mechanical vibration
• Ultrasound
• Electrostimulation
• Dry needling
• Spray and stretch
• Low level laser therapy
• Massage
• Tapotement
• Muscle energy
techniques
• Proprioceptive
neuromuscular
facilitation
Physician and Physical Therapy Treatment of
Myofascial Pain
• Trigger Point Injections : 838,000 results on Google but
very few physicians know how to do them
• Dry Needling: can be done by mid level providers, but
government standards should be required
• Absence of consensus: in preparation of a study on the
effect of a specific stretching technique for the treatment
of headache, a group in Springfield, MA surveyed over
200 Physical Therapy Clinics. In the 130 replies, there
was no common practice for the treatment of headache
and fewer than 10 regularly used a stretching technique
which the patient could use at home.(Laura Martorello DPE,
MSPT, American International College, Department of Physical Therapy,
personal communication, 2012)
MYOFASCIAL MEDICINE
Where should we go?
How can society benefit from Myofascial
Medicine?
• Faster and more accurate diagnoses
• Improved understanding of disease processes
• Reduce needless testing
• Reduce needless treatment
• Recognize certain illnesses are mostly myofascial, e.g.
headache
• Reassures patients
• Reduce costs
Myofascial Medicine: what do we lack?
• Identify the anatomic nature of the trigger point
• Identify the mechanism of referred pain (spinal cord,
sympathetic ganglia, other structures)
• Determine if the central physiologic (and perhaps
anatomic) manifestations of MFP are different from other
types of pain.
• Identify the exact biochemistry , metabolism, and genome
of the trigger point
• Devise a pharmacology for the trigger point (revisit
botulinum toxin injections?)
Myofascial Medicine: what do we lack? 2
• Physician training program starting in medical school
• Academic support for clinical research
• Validated methods of diagnosis
• Validated methods of treatment or a consensus
methodology
• Succession planning
• Forum for communication of developments of practice
and research
Suggestions for the field of Myofascial Medicine
• Construct clinical experiments that control for placebo
•
•
•
•
effects
Lobby for funding of basic science research in myofascial
pain.
Fund professorships and then departments in myofascial
pain
Start medical training in myofascial pain in first year
anatomy class
Incorporate training in myofascial pain in Neurology,
Emergency Room, Internal Medicine, General Practice,
and Anesthesiology Pain fellowship training
Suggestions for the field of Myofascial Medicine 2
• Board certification in Myofascial Medicine (joint boards
between Neurology, ER, GP, IM Pain fellowship
constituencies requiring board certification in the primary
specialty with special competency in Myofascial
Medicine).
• Standard or consensus protocols for treatment of
Myofascial Pain and specific training within the fields of
Physical Therapy, Chiropractic, and other disciplines
• A forum for the discussion of the science and practice of
Myofascial Medicine which will expect academic rigor and
which will put new information in context for the
professional and lay reader.
Journal of Musculoskeletal Pain
Mission
• Official journal of the
International Myopain
Society
• Forum for research and
discussion of muscle pain,
particularly myofascial pain
and fibromyalgia
• Will encourage research and
commentary on muscle pain
• Coming soon by post and by
electronic devise.
Associate and Section Editors
• Scott Mist, PhD, Portland
•
•
•
•
•
OR
Robert Gerwin MD,
Bethesda, MD
Matthew Robbins MD, New
York, NY
Siddhartha Sikdar, PhD,
Fairfax, VA
Daniel Wallace MD, Los
Angeles, CA
Kim Jones, PhD, Portland,
OR
Journal of Musculoskeletal Pain
THE OFFICIAL JOURNAL OF T HE INTERNATIONAL MYOPAIN SOCIETY
• Research Articles
• Editorials
• Literature Summaries
Reviews
Essays
Letters
Thanks for Your Attention