Comparative Healthcare Systems
advertisement
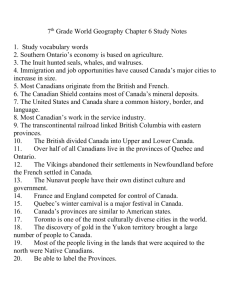
Comparative Healthcare Systems And Health System Reform November 11, 2006 (!!!!!!comparative healthcare systems fall 2006.ppt) Why study different systems? First, many European countries have constructed programs that predate U.S. programs by decades. (There is a wide variation in programs and experiences that is worth discovering in and of itself.) Second, the U.S. system has some huge holes compared with the coverage in many other systems. Understanding the approaches used by other countries may provide important clues to assessing our own system. Many industrialized countries either provide: 1. health care directly through the government 2.publicly funded health insurance with comprehensive coverage. Classifications of Health Care Systems 1. 2. Traditional sickness insurance: fundamentally a private insurance market approach with a state subsidy. (Example: Germany) National health insurance: a nationallevel health insurance system. (Examples: Canada, Finland, Norway, Spain, and Sweden.) Classifications of Health Care Systems (con.) 3. National health services: state provides the health care. (Examples: Denmark, Greece, Italy, New Zealand, Portugal, Turkey, and the United Kingdom.) 4. Mixed systems: contain elements of both traditional sickness insurance and national health coverage. (Examples: Switzerland, and the United States.) The Countries Vary Substantially from the US Other countries (e.g., Denmark, France, Italy, the Netherlands, and Switzerland) spend larger percentages on inpatient care than does the United States. For 1998 the U.S. pharmaceutical expenditures were among the lowest in percentage terms among all of the countries. Several countries have lower rates of infant mortality (deaths per 1,000 live births) than does the United States. Several countries also have higher lifeexpectancies at birth. The United States has the largest expenditure per capita ($5,267). It is also the biggest spender as a share of GDP. Such facts and concerns about access to health care are some indicators causing many to question whether Americans are getting the biggest bang for the buck. Note: High expenditures may have three potential meanings: High average level of services High resource costs for services Inefficient provision of services Keep these points in mind. A high level of services could reflect the possibility that populations have chosen to spend their incomes in this fashion. (Healthcare is a normal good) THE UNITED KINGDOM-THE NATIONAL HEALTH SERVICE National Health Service (NHS) was established in 1948 and provides health care to all British residents. It is financed largely (about 83%) through general revenues, with the capital and current budget filtering from the national level down to the regional, and then to the district level. Services are free to patients at the point of use. It pays general practitioners on a capitation basis and hospital physicians largely on a salaried basis. There is also a private sector health system. (About 10 percent of Britons purchase private health insurance.) Services are not entirely free. --private hospital rooms extra --small surcharge for drug prescriptions filled outside the hospital. --copayments: Dental care & eyeglasses The general practitioner (GP) is the gatekeeper to the health care system. (GPs are not government employees. Rather, they are self-employed and receive about half their incomes from capitation contracts.) approximately 35,000 GPs in 9,000 practices, servicing 90 % of all patients Consultants are specialists, and patients must be referred to them by GPs. (Spending per capita ($2,160) in the United Kingdom in 2002 was just 41 percent of the United States level ($5,267) and a little more than half when expressed as a ratio to GDP (7.7 percent as opposed to about 15 percent). How does the United Kingdom keep its health care expenditures this much lower while providing universal access to health care? Though patients have relatively easy access to primary and emergency care, specialty care is rationed through long waiting lists and a limit on the availability of new technologies. Performance Under the NHS and More Recent Reforms The effect of a system such as the NHS that depends on queuing (waiting lists) for access to care is often to postpone, or simply not provide, certain services. The NHS devotes considerable resources to high-return services as prenatal and infant care. To the populations served, and to the larger public concerned with equitable provision of care, the universal nature of the service is beneficial. Although the United Kingdom has spent considerably less on health care than the United States and many other countries, by most measures of mortality and morbidity the UK does about as well. Certainly, many non-medical factors are involved in determining disease and death rates in a population, and these factors also will vary across countries. Despite universal access to care in the United Kingdom, historically there have been considerable regional disparities in funding and in the use of health care. Evidence shows that upper-class patients have received substantially more care for a given illness than have lower-class patients Conclusion The experience of the NHS in the area of cost containment is fairly clear. Rationed care cuts money costs, and even with increased expenditures from the healthcare reforms, total U.K. expenditures are expected to be well below the European Union and the United States. 45 million uninsured is a limitation of the US system. A wait list of 1 million is a short coming of UK system. GERMANY: Sickness Funds The German health care system is based on programs laid out by Bismarck in 1883. Legislation required workers in various occupations to enroll in sickness insurance funds. The basic approach of mandatory enrollment in autonomous (independent) sickness funds, financed by payroll taxes, lies at the heart of the German social insurance program. The German health care system is characterized by the "three S's"- social solidarity, subsidiarity (decentralization to public and private organizations), and self- governance. Social Solidarity: the sense that all citizens are concerned with the provision of equal access to health care. This is at the heart of the German health system. Structure of the German System All working persons must have health insurance. Costs are divided equally between employer and employee. Employees' shares collected as payroll taxes at rates proportional to their gross wages. (average contribution rate to sickness funds in 2003 was 14.3 percent.) Since the funding is based on wages, if wages fail to grow at the same rate as costs of health care, funding issues will arise. Individuals with income beyond a given ceiling may choose the private health system, which handles from 10% of the population. The social insurance component is organized around about 292 localized sickness funds. These funds are independent and selfregulating. Funds pay providers directly for services provided to their members at rates that they negotiate with individual hospitals - 70% of health spending. It was not always possible for members of the Statutory Health Insurance (SHI) system to choose which sickness fund they wished to join since membership was determined by occupational status. As part of reforms of the late 1990s, however, individuals have been able to change funds. Altenstetter (2002) notes that the bulk of membership changes occurred from the general sickness funds (with the highest number of the elderly) to the "enterprise funds," which offer lower payroll taxes. What concept is illustrated here? The sickness funds are required by law to provide a comprehensive set of benefits. (e.g. physician ambulatory care provided by physicians in private practice, hospital care, home nursing care, and a wide range of preventive services. The funds, like disability insurance in the U.S., also provide additional cash payments to those who are unemployed as a result of illness.) Reimbursement: ambulatory providers are paid on a fee-for-service basis, hospitals on a prospective basis. Doc fees are negotiated between sickness funds and regional Doc associations. Both public and private hospitals exist, public about 50%. Hospitals tend to use salaried physicians. Hospital operating expenses covered by sickness funds and capital expenses covered by the state. Unlike the United States, physicians in private practice generally do not have hospital admitting privileges. Thus, many doctors have invested in well-equipped clinics to compete with hospitals by being able to perform a wide range of procedures. Why is the German experience relevant to the United States? Coverage is provided through a number of relatively small and independent plans. In this sense, the delivery of health care is similar to that found in the United States In the U.S., for the most part, large numbers of employee groups, independent insurers, and providers reach agreements without direct government intervention. Many Americans propose mandated coverage for the working uninsured. Germany relies on a mandated approach where coverage for certain conditions is required by law. Germany also introduced cost controls similar in principle to prospective payment under the DRG mechanism in the U.S. Medicare program. Each level of Government has specific responsibilities. The central government passes legislation on policy and jurisdiction. State governments are responsible for hospital planning, managing state hospitals, and supervising the sickness funds and physician associations. Local governments manage local hospitals and public health programs. Within this framework, decentralization is considerable. As noted, the sickness funds and physician associations have considerable administrative autonomy. Despite this autonomy, government intervention is extensive and has been increasing steadily. Cost Containment Act of 1977 introduced a fixed budget for payments by the sickness funds to the physician associations. (program similar to prospective payment schemes developed in the US.) Hospitals were required to negotiate prospective budgets with sickness funds. Note the incentives here. As sickness fund costs continued to rise at a greater rate than incomes, the call for reform continued, leading to the 1993 Health Care Reform Act. To introduce supply-side competition, the reforms also gave members the freedom to choose among a range of sickness funds whose revenues would be determined by the risks of their members. The reforms further changed the hospital payment system from a perdiem payment to a DRG-styled prospective payment basis. Subsequent legislation in 1997 was aimed at continuing the momentum toward competition. The SHI Modernization Act of 2003: increase efficiency and quality of the system Cost savings achieved by shifting costs to users and the SHI insured. Costs savings also from targeted providers and the pharmaceutical industry. Main elements of savings or costshifts: Exclusion of some benefits: especially overthe-counter drugs. While children under 18, antenatal care, and preventive services are still exempt from copayments, the general exemption of poor people was abolished. Annual co-pays are limited to 1% - 2% of household income. Performance of German System German health system has been relatively successful at controlling costs. Before the period of reforms, 1970 to 1977, spending increased at a 14.4 percent annual rate, but this dropped to 6.5 percent from 1977 to 1983 and to 5.1 percent from 1983 to 1989. German health system has been relatively successful at controlling costs. Although the expenditures as a percentage of GDP have risen over the decade of the 1990s, this was because of German reunification. It has a publicly funded system with virtually universal coverage but has avoided queues and extensive government intrusion. (Both patient and provider have considerable autonomy.) Challenges to German System: The German population is aging rapidly causing a demographic change that will place severe pressure on its social security and health care programs. Rurst (1991) claims that an overemphasis is placed on high-tech medicine at the expense of preventive and long-term care. High unemployment rates has narrowed the base for payroll contributions to the funds. Those with private insurance have more choice than those in the statutory programs, and similarly situated individuals may contribute different amounts to their sickness funds because the membership profiles of their respective funds are different. Co-payments are now an integral part of the German system. The German system has put considerable emphasis on free choice, ready access, high numbers of providers, and technological equipment. Formal waiting lists are virtually unknown. The public has accepted these priorities and they are used to assess the system. They have placed less emphasis on cost containment. Germany has many problems similar to those in the U.S. (e.g. aging population) THE CANADIAN HEALTH CARE SYSTEM: Why the interest? There have been rapid increases in U.S. health care costs and growing concern over the large number of uninsured. Is Canada's health system a possible model for reform in this country? There is a widespread perception in the U.S. is that Canada has successfully developed a comprehensive and universal national health insurance program that is cost effective and highly popular. The extraordinary U.S. interest in Canada's approach is attributable to the fact that Canada and the United States share a long border and similar heritage in terms of language, culture, and economic institutions. Key Facts about Canada & the US 1. 2. 3. Canada is geographically larger than the United States but has slightly more than one-tenth the U.S. population. Although a wealthy country, its GDP per capita is only about 80 percent of the U.S. level. Canada has a relatively high level of social services, with public expenditures representing 42 percent of GDP compared to 34 percent for the United States. 4. 5. With a national health system providing universal coverage, public funds account for more 70% of total health spending while it’s 45% in the U.S. However, not all services are covered (e.g., vision, dental, prescription drugs, semiprivate and private rooms), meaning that private funds account for nearly a one-third share that has grown in recent years. 6. 7. 8. Canada has maintained lower health spending and share of GDP per capita than the United States, despite its higher bedpopulation ratio and longer lengths of stay. Canada's physician-population ratio is 12 percent lower and its nurse staffing level 27 percent higher than the U.S. level. Americans spend 82 percent more per capita on health care ($5,267 vs. $2,931), although about 15 percent of the U.S. population goes without insurance coverage at any time. 9. 10. Despite lower spending, health status indicators-such as life expectancy (about 2 1/2 years longer for both men and women in Canada). Public opinion polls indicate that Canadians support their system more than Americans support theirs and are concerned about any threats to it. BACKGROUND The Canadian system of financing and delivering health care is known as Medicare Each of the 10 provinces and 3 territories administers a comprehensive and universal program that is partially supported by grants from the federal government. Various criteria established by the federal government with respect to coverage must be met. 1. 2. 3. Coverage must be universal, comprehensive, and portable, meaning that individuals can transfer their coverage to other provinces as they migrate across the country. There are no financial barriers to access Patients must have free choice in the selection of providers. (i.e. usually no outof-pocket charges) Differences between Canada's Medicare and Britain's National Health Service. Most Canadian physicians are in private practice and have hospital admitting privileges. They are reimbursed by the provinces on a fee-for-service basis under fee schedules negotiated by the provinces and physician organizations. Hospitals are also private institutions, although their budgets are approved and largely funded by the provinces. The Canadian system originated in the 1930s when compulsory health insurance programs were introduced by some provinces. Since 1972, every province and territory has provided universal coverage for hospital and physician care. Health researchers have focused on the sources of the savings under the Canadian plan. U.S. fees were considerably higher in each category. The net incomes of U.S. doctors were also substantially higher than were their Canadian counterparts. PHYSICIAN FEES AND QUANTITY Fuchs and Hahn (1990) provide a detailed breakdown of Canadian and U.S. expenditures by specific services, while separating their price and quantity components Fuchs and Hahn (1990) disparity in spending on physician services it was 72 percent higher in the United States 178 percent higher for the procedures component. (The relative ratios of Iowa to Manitoba were slightly lower.) Fuchs and Hahn (1990) Because spending is the product of prices and quantities, it seems logical to pursue differences in fees (prices) and utilization per capita (quantities). Overall, fees were 239 percent higher in the United States for 1985. U.S. fees were considerably higher in each category. The net incomes of U.S. doctors were also substantially higher than were their Canadian counterparts. Fuchs and Hahn (1990) Perhaps more surprising than the fee differentials are estimates of the service volume. Despite the much higher spending per capita for physician care, the quantity of care per capita was considerably lower in the United States. Thus, the savings in Canada, at least for physician care, do not come from reduced volume of care. WHY ARE FEES AND HOSPITAL COSTS LOWER IN CANADA? Patients in Canada have longer lengths of stay, in part because of the greater use of Canadian hospitals for chronic long-term care. Nonetheless, after adjusting for differences in case mix between the two countries, the cost per case-mix adjusted unit was roughly 50 percent higher in the United States. Several reasons can be proposed for this phenomenon. Why???? Single purchaser of medical services keeps prices below market rates. In Canada, unlike the United States, physician fees result from negotiation between physicians' organizations and the provincial governments, as well as from other limits on total spending. Physicians cannot evade the fee controls by charging extra (sometimes called balance billing) to patients who can afford it. Hospital costs are similarly regulated by the provinces through approval of hospital budgets. Hospitals and provinces negotiate operating budgets financed by the provincial governments. The capital budget may include other sources of funding, but provinces still must approve capital expenditures. Thus, a centralized mechanism allocates resources to the hospital sector and determines the distribution of resources among hospitals. Occupancy rates are higher in Canadian hospitals. The provinces have limited the capital costs associated with expensive new technologies. One study provides comparisons on the availability of several relatively recent and expensive technologies among Canada, the United States, Germany, and Korea, with some other OECD countries available for comparison. Although analyses from the 1980s indicated that the United States has greater availability of many of the technologies, data for 2002 suggest that other countries are catching up. ADMINISTRATIVE COSTS The centralized system of health care control in Canada has led to theories about the possible economies associated with administrative and other overhead expenses. Administrative costs in the United States increased account for about 31 percent of health care spending. Similar costs in Canada are about 14 percent. (If we could get to this percent, the savings are estimated at about $160 billion.) A COMPARISON Canadian system appears to be more effective than the U.S. system in several respects. Costs are lower, more services are provided, financial barriers do not exist, and health status as measured by mortality rates is superior. Canadians have longer life expectancies and lower infant mortality rates than do U.S. residents. However, the comparisons do not tell necessarily imply that the United States should adopt the Canadian approach. Many Canadians are no longer confident that the provinces will be able to afford their current systems. As a result of unprecedented federal deficits, the Canadian government has reduced substantially its cash transfers to the provinces. The provinces are thus faced with the following options to cope with their increased burdens: find new sources of tax revenue, impose more stringent fee and budgetary controls on health providers, find ways to increase efficiency in health care delivery, scale back on benefits by no longer insuring some previously covered services, and impose user fees. (Similar to the shift we have seen for the U.S., the provinces have forced large reductions in hospital capacity with a corresponding substitution of outpatient care for inpatient care.) Regional boards with budgetary authority have replaced centralized provincial departments. The goals of this reorganization are similar to those expected from managed care: develop an efficient, coordinated, and accountable system for the regional population. Done with planning instead of competition through markets. Rationing of care like in the UK (note: a famous Quebec court case in 2005 has opened up the private health insurance market) The consensus is that the limits on capacity and on new technology result in longer waiting periods for hospital services. Defenders of the U.S. approach claim that: The waiting and queues found in Canada would be unacceptable to many U.S. patients. There is a greater level of amenities in the United States, and the greater availability of specialized care, together with high-tech medicine, often is viewed as an indicator of superior quality. NATIONAL HEALTH INSURANCE Return now to the question of broader social insurance for health care. Should the United States adopt national health insurance? Steps toward cost containment may be more palatable in the current climate. Health system reform is still on the agenda in the United States and many other countries. It is wise to be acquainted with the possible features of such plans. DIFFERENT KINDS OF POSSIBLE NATIONAL HEALTH INSURANCE (NHI) PLANS A national health insurance scheme should possess several desirable aspects. It should: provide a health "safety net" for all residents, irrespective of age or employment status. provide choice for providers and patients. provide market incentives for cost containment. be relatively easy to administer. Policymakers faced a dilemma as to whether to fund national health insurance coverage by individual mandate, employer/employee mandate, or general revenues. What are the additional costs to society from the imposition of NHI? From society's point of view, the incremental cost of NHI in the United States is the extra total expenditure on health care that would be incurred if we switched to national health insurance. Since most people already are insured for almost all hospital care and most physician care, the extra cost of NHI would be much smaller than many people expect. True incremental costs stem from several sources. The major reason for switching to a national health insurance plan is to extend coverage to the uninsured, more than 45 million people. The estimated incremental cost is between $34 and $68 billion, about $459 per person, or about 3 - 6 percent of health care spending. Second, the insured population will incur some incremental cost to the extent that the national health insurance proposal chosen provides greater typical coverage than people already choose to buy or have provided to them by other sources. Third, any tax-supported system of financing care necessarily entails a deadweight loss to society. This is true even if the program is of the employer-mandated type because a law forcing employers to incur expense is really a tax. The deadweight loss of a tax means that some efficiency loss will result, caused by the disincentives to work and invest. ENSURING ACCESS TO CARE Let’s group reforms by their two main motivations: 1. the desire to see that people who are sick get health care 2 the desire to control the rising cost of health care. INDIVIDUAL VERSUS EMPLOYER MANDATES The country that wishes to provide universal coverage for health care must choose one scheme or another to extract tax payments from its households. In the U.S. health debate, two mechanisms were featured in proposals and thus contrasted: Individual versus Employer Mandates. Employer mandates are important to health systems in Europe, Latin America, and Asia. Under the employer mandate, the employer must procure health insurance for its employees and their dependents. Although the employer writes the check, the firm undoubtedly will pass on as much of this cost as it can to customers in the form of higher prices, or to employees in the form of lower wages. Under the individual mandate, workers are obligated to purchase health insurance for themselves and their families, either from private insurance (individually purchased) or through a group such as a work group, professional organization, or religious group. The poor are subsidized in their purchases through government taxation of the relatively well-to-do. SEPARATION OF HEALTH INSURANCE FROM EMPLOYMENT In postwar years, employer contributions to health insurance were and continue to be tax exempt, providing workers with a substantial discount and thus inviting inefficiencies of over-insurance. If you are not employed, you probably will have trouble getting insurance. Health insurance problems also occur when workers change jobs. When leaving their old company's health coverage behind them, workers have little choice but to buy an individual policy or do without insurance entirely. To deal with these and other distortions, some economists recommend radical changes in the tax system to remove the tax subsidy that effectively ties health insurance to the workplace. Fuchs (1994, p. 11) argues: ". ..that if government imposes enough mandates, enough subsidies, enough surcharges, and enough controls and regulations, the tie to employment can be severed.” Fuchs recommends a value-added tax to finance universal coverage of health insurance. It is not without controversy, but it does suggest an alternative system in which health insurance is not tied to the job. Single Payer May reduce administrative costs. May be able to guarantee a minimum level of coverage for everyone (Free marketers would argue that this takes away from choice.) Structure of the Korean System In 1977, South Korea required all firms with more than 500 employees to establish insurance societies to provide health care benefits. (By January 1988 it included firms with fewer than five employees.) A second scheme was phased in for government employees, teachers, dependents of soldiers, and pensioners under another law. Similarly, the self-employed, farmers, fishermen, and other occupational groups were phased in under a third program. Finally, low-income individuals were covered by public insurance similar to Medicaid. The insurance was to be provided by over 350 insurance societies and financed by employer contributions and payroll deductions. (e.g., for the employee program (class I), deductions are taken as percentages of wages or salaries. These are shared equally between employers and employees at rates ranging from 3 to 8 percent.) The insurance societies also determine the benefits and cover a broad range of inpatient and outpatient services. The system is characterized by a relatively high coinsurance rate of 20 percent for hospital inpatient care and 30 to 55 percent for outpatient care. The expansion of insurance and the rapid growth of South Korea's economy has been a rapid increase in utilization and costs. (e.g., annual outpatient visits per person for class I beneficiaries increased from 1.3 in 1977 to 6.2 in 1987; hospital inpatient cases increased from 3.0 to 6.2 per 100 persons. Spending as a share of GDP also rose from 2.8 percent of GDP in 1978 to 3.9 percent by 1990 and 5.0 percent by 1998.) Performance in South Korea's system 1. 2. (SK’s cost-containment policies rely on fee controls & high coinsurance rates.) Under the fee schedules, all providers in each of three categories (comparable to community hospitals, teaching and specialty hospitals, and clinics) are reimbursed a uniform amount for an insured service. In addition to high coinsurance rates, a fixed consultation fee for each outpatient medical and dental visit was introduced in 1986 to help limit spending. It’s difficult to isolate the effects of the cost-containment measures because of the rapid increases in income since the health care plan was put in place. As one would expect, the co-payments reduced the probability of outpatient visits. However, they had no effect on spending because patients and providers reacted rationally by offsetting the reduced contacts with more services per visit. Conclusion: the South Korean experience is a powerful demonstration to emerging industrial countries that it is possible to phase in a mandated employment based insurance system without serious adverse effects on a nation's economy. Transition to a Single Insurer South Korea was able to bring universal coverage to a then less-developed country in a very short time. The pluralistic financing system (350 insurance societies) has ultimately proved to be unworkable. (particular problems in risk pooling, particularly among the smaller societies, and in determining the appropriate worker contributions.) Response: a fundamental change in the structure of the national health insurance system. All health insurance societies were merged into one in July 2000 to improve the ability to engage in risk pooling.