File
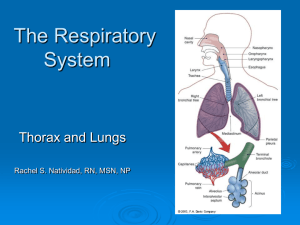
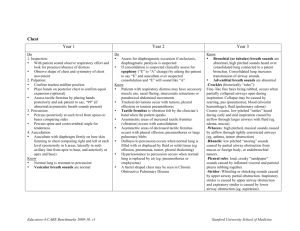
advertisement

Fundamentals of the Chest Physical Exam RESD 60 Bedside Assessment Skills Patient Interview History Taking Physical Examination Medical Record Keeping Respiratory Recap Variables supporting a therapeutic climate Caring Demeanor Competence Eye Contact Judicious use of touch Professional Image Terms used to describe illness Symptom Sign Finding Syndrome Disease Symptom Something felt by an individual as a departure from normal. A subjective abnormality perceived by the patient. Examples: dyspnea chest pain leg swelling Sign An observable or measurable bodily manifestation that serves to indicate the presence of malfunction or disease. Examples: tachypnea dullness to percussion pedal edema Sign or symptom In the investigation of a symptom or sign be quantitative whenever possible. “8 on a scale of 10” “2 to 3 minutes” Finding An observation or manifestation of disease as a result of an investigative procedure. Typical procedures; blood work, radiology. Examples: right lower lobe infiltrate increase white blood cell count. Syndrome A set of symptoms, signs, and/or findings that characteristically occur together which may signify a specific disease process. Examples COPD pneumonia Disease A particular pathologic condition or process whose pathophysiology or cause is known. Examples pneumococcal pneumonia alpha-1-antitrypsin deficiency Cardinal signs and symptoms of Cardiopulmonary Disease Dyspnea Cough Hemoptysis Chest Pain Cardinal signs and symptoms of Cardiopulmonary Disease Wheezing Clubbing Stridor Edema Cyanosis Dyspnea Shortness of breath The subjective sensation that one’s breathing is inadequate or insufficient. An uncomfortable awareness of the act of breathing. Cough A sudden, noisy expulsion of air from the lungs, brought about through a reflex action, for the purpose of clearing the airways. A normal event that becomes a symptom when it is frequent or bothersome. Nonproductive or productive Hemoptysis The coughing up of blood from the respiratory tract below the level of the larynx. This term is usually reserved for fresh blood. Chest Pain Any uncomfortable sensation referable by the patient to the thoracic area. Pleuritic - worsened by breathing or coughing. Wheezing A high-pitched, musical sound produced when the patient breathes, originating in narrowed airways. May occupy either a portion or all of the respiratory cycle. Stridor A harsh, high-pitched sound, usually on inspiration. Associated with partial laryngeal obstruction. Cyanosis A bluish discoloration of the skin and mucous membranes due to the presence of increased quantities of reduced hemoglobin. Cyanosis may be peripheral or central. Cyanosis Clubbing Enlargement of the end of the fingers and toes due to buildup of soft tissue in the nail bed. Occurs in several chronic lung diseases. Clubbing of the fingers Edema Presence of large amts of fluid in the intercellular tissue spaces of the body. Pitting - seen with CHF. Increased fluid due to increased hydrostatic pressure. Non-pitting - seen with infection due to increased capillary permeability. Pitting Edema Present Illness The present illness is the clinical problem of primary concern at the moment. The chief complaint is what caused the patient to seek medical attention. Physical Examination A physical examination is done to detect the the physical signs of disease. The RCP has 3 considerations: Diagnostic Therapeutic Evaluation Components of Physical Examination Inspection Palpation Percussion Auscultation Inspection View from the door Isolation patient position Family equipment Entering the room Introduction Patient’s last name Establish a brief rapport Vital Signs body temperature heart rate respiratory rate blood pressure Sensorium An alert patient is oriented to person, place and time. An abnormal sensorium suggests that a person may have poor oxygenation. Can also occur with drugs and disease states. Physical Inspection - Head to Toe Head facial expression color nose mouth eyes Physical Inspection Neck Tracheal position Jugular venous pressure Accessory muscle use Trachea Tracheal Deviation to the R Jugular Venous Pressure JVD Chest configuration The normal adult thorax is broader for side to side than front to back. An increased anteroposterior (AP) diameter is common with emphysema. Barrel chest. Chest configuration Pectus excavatum - funnel shaped depression of the lower portion of the sternum. Pectus carinatum - sternum protrudes outward. Sternal Abnormalities Increased A-P Diameter Physical examination - spinal column. Scoliosis - abnormal, lateral curvature of the spine. Kyphosis - an increased AP curvature of the spine. Kyphoscoliosis - combination Kyphosis Physical examination breathing pattern Respiratory rate and pattern are always evaluated. Rapid and shallow breathing is associated with restrictive lung disease. Prolonged expiratory time is common with obstructive disease. Physical Examination breathing pattern Note the timing of the inspiratory and expiratory phase of breathing. A prolonged expiratory time is common with obstruction of the intrathoracic airways. Obstruction of the upper airway leads to prolonged inspiratory time. Breathing pattern Assess Look the patient’s effort to breathe. for: retractions paradoxical respirations flail chest chest symmetry Pursed lips Tripoding Pursed Lips Tripod and Pursed Lips Physical examination - digits The digits are inspected for: cyanosis clubbing Palpation Palpation is used to evaluate the symmetry and degree of chest expansion with breathing. Tactile Fremitus Capillary Refill Tracheal position To palpate, percuss and auscultate chest you must know the anatomy. Posterior View Palpating for Lung Expansion Percussion Percussion is performed to help evaluate relative amounts of air and solid material in the underlying lung. Percussion over normal air-filled lung will produce a drum like sound described as normal resonance. Percussion Increased or hyper resonance is a , lower pitched sound. This occurs with emphysema or pneumothorax. Percussion Dull or flat describes a note that is softer and higher-pitched than normal. This sound is heard over areas of pneumonia, atelectasis, lung tumor, or pleural effusion. Tactile Fremitus Auscultation Auscultation is the process of listening to sounds produced within the body with a stethoscope. Whenever possible the patient should be sitting upright. Stethoscope Anterior Auscultation Lateral Auscultation Posterior Auscultation Auscultation Inspiration and expiration should be evaluated for length and adventitious sounds. Auscultate directly on the skin when possible. Auscultate anterior, lateral, and posterior chest wall surfaces. Normal Breath Sounds Normal breath sounds are divided into three different types Bronchial Bronchovesicular Vesicular Bronchial breath sounds Loud and high-pitched equal inspiratory and expiratory heard over trachea also called tracheal, tracheobronchial or tubular Bronchovesicular breath sounds Softer and lower pitched than bronchial breath sounds. Heard on the anterior chest near the mainstem bronchi in the first and second intercostal spaces. Heard on the posterior chest between the scapulae. Vesicular breath sounds Soft, low-pitched sounds, heard during auscultation over the lung. Normal air-filled lung contains millions of alveoli, which act as a sound filter to turbulent flow in the central airways. Vesicular breath sounds Flow in the peripheral airways is laminar and does not contribute significantly to sound production. If the vesicular breath sound is softer than expected, it is describes as diminished, decreased, or even absent. Vesicular breath sounds Breath sounds are decreased with the following: shallow breathing hyperinflation obstructed airways pleural effusion pneumothorax obesity Vesicular breath sounds Louder than expected vesicular breath sounds are described as harsh. Consolidation does not filter sound, but allows them to pass through the lung more directly. Adventitious breath sounds Abnormal sounds heard during auscultation are termed adventitious breath sounds. The can be continuous, musical sounds or discontinuous, non-musical. Continuous/musical Wheeze - low pitched sound resulting from narrowing of the airways. Timing is usually expiratory, but can be inspiratory or both. “louder” wheezes usually mean moderate obstruction. Continuous/musical Low pitched continuous sounds are termed rhonchi. Timing is usually expiratory. Indicative of secretions in the lung. Continuous/musical A high-pitched continuous sound heard over the upper airway is referred to as stridor. Stridor is often audible and can be a sign of a life-threatening disorder. Discontinuous Sounds Sounds described as intermittent, crackling, bubbling, and of short duration. Termed rales or crackles. Crackles Produced by two mechanisms; excessive airway secretions with breathing and sudden opening of the small airways. Sudden opening of the small airways. Crackles Crackles are inspiratory sounds and associated with restrictive disorders such as: atelectasis (late inspiratory) pneumonia pulmonary fibrosis Voice Sounds Normally, air-filled lung filters the voice so that it is heard as low-pitched mumble over the chest wall. When lung tissue becomes dense, vocal resonance increases and the voice is heard more clearly. Voice Sounds Increase in vocal resonance is termed bronchophony. An increase in vocal resonance is heard with the consolidation that occurs with pneumonia. Voice Sounds A decrease in vocal resonance occurs when the lung becomes less dense, as with hyperinflation. Voice Sounds When to voice sound increases in intensity and takes on a nasal or bleating characteristic, it is termed egophony. Ask the patient to say “e” and the “e” will be heard as “a” over the area of consolidation. Voice Sounds When consolidation is present, whispered sounds are transmitted more directly. When whispered sounds are heard with more clarity, they are described as whispered pectoriloquy. Neurological Assessment LOC – Level of Consciousness Glasgow comma scale PERRLA—pupils equal, round, and reactive to light and accommodation Neurologic Assessment Posturing Decerebrate Decorticate