10. Resilience in neurological injury - A. Craig
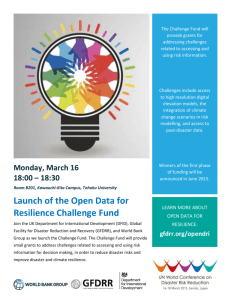
advertisement

Protection against the adversity of neurological injury: The process of learning to be resilient Dr Ashley Craig, Professor, Rehabilitation Studies Unit, Sydney Medical School, The University of Sydney Based on work funded by the ARC and MAA 1 Senior Clinical Psychologist READ Clinic, Hill St Gosford The resilience material presented tonight can also be found in my Chapter 26 “Resilience in People with Physical Disabilities” recently published (2012) by Oxford Press Resilience following injury is an important area of study, and which many of you I am sure have significant ideas about. I hope this talk can challenge those ideas, and provide new insights into helping people who need to develop resilience How resilient do you think you are? The nature of resilience Resilience studies attempt to discover why and how people cope and adjust to adversity Early studies of children in New York who thrived with single mothers who had schizophrenia were the catalyst for the emergence of the study of resilience What is resilience? Luthar et al., (2000) defined resilience as: “.. a dynamic process encompassing positive adaptation within the context of significant adversity.” (p.543) In disability, I have defined resilience as: “the process of maintaining stable psychological, social and physical functioning when adjusting to the effects of a disability or injury and subsequent impairment”. Craig, A. (2012). Resilience in people with physical disabilities. In P. Kennedy (Ed.). The Oxford Handbook of Rehabilitation Psychology. Oxford: Oxford University Press, p.474-491. Resilient behaviour is characterised by: A belief in themselves as effective in self management An ability to form close relationships An ability to achieve positive outcomes in their daily lives A degree of autonomy An ability to problem solve An ability to be optimistic and humerous despite adversity An ability to manage stress and trauma associated with adversity Craig, A. (2012). Resilience in people with physical disabilities. In P. Kennedy (Ed.). The Oxford Handbook of Rehabilitation Psychology. Oxford: Oxford University Press, p.474-491. Rees, R. (2012). Resilience of people with traumatic brain injury and their carers. InPsych, April, 12-13. Resilience research involves assessing protective factors Protective factors Environmental Social and interpersonal Psychological and physical community resources healthy environment secure housing financial resources education opportunities community cohesion recreation facilities stable family support affection employment socially active positive attachments friends support access to social networks robust self esteem a sense of self mastery physically healthy problem solving skills adequate social skills stable mood states adequate coping skills …and risk factors Risk factors Environmental limited resources unhealthy environment insecure housing poor finances lack of education stressful living context Social and interpersonal no family support poor social networks unemployed avoids activities single frequent hospitalization Psychological and physical elevated anxiety sense of helplessness elderly poor insight lack of communication skills depressive mood significant cognitive deficits Factors shown to protect against psychiatric distress Rutter (1985) proposed a number of protective factors that have the potential to modify, alter or cushion a person from the negative consequences of adversity Factors included: a constructive/ realistic understanding of events taking adaptive action a robust self-esteem and a strong sense of mastery or self efficacy being adaptable when faced with change having problem solving skills a sense of humor when faced with stressful events/ optimism dealing successfully with problems in the past accepting responsibility when dealing with problems quality social support Rutter, M. (1985). Resilience in the face of adversity. Protective factors and resistance to psychiatric disorder. British Journal of Psychiatry, 147, 598–611. Some prominent factors shown to protect against injury and distress Self efficacy and resilience Self efficacy: the extent to which a person perceives they can control their behaviour, lives and daily outcomes Maciejewski et al., (2000) showed self efficacy was a very significant predictor of depressive symptom severity Having a higher level of self efficacy resulted in fewer depressive mood symptoms in adults. Self- efficacy mediated around 40% of the effects of stressful life events on depressive mood They concluded that maintaining a healthy self efficacy, that is, a strong sense of control or mastery over one’s life and environment, serves to protect a person from psychopathology, by ameliorating the negative effect of stressful life events Maciejewski, P. K., Prigerson, H. G., & Mazure, C. M. (2000). Self-efficacy as a mediator between stressful life events and depressive symptoms. British Journal of Psychiatry, 174, 373-378 Catastrophic thinking and resilience If a person’s style of thinking is catastrophic or very negative, then resilience is less likely Catastrophic thinking and resilience Thinking realistically and adaptively about adversity helps the resilience process For example, in chronic pain, Sullivan et al (1998) found that catastrophising about pain was significantly associated with reduced capacity to cope, increased pain intensity and perceived disability, and lowered employment status Catastrophising contributed to the prediction of disability over and above the variance accounted for by pain intensity Catastrophising was associated with disability independent of the levels of depression and anxiety. Rumination was the strongest predictor of pain and disability Sullivan, M.J.L., et al., (1998). Catastrophizing, pain, and disability in patients with soft-tissue injuries. Pain, 77, 253–260 Pain Catastrophising Catastrophising involves focusing on pain in a very negative and unhelpful manner Example: “I cant stand it any longer. It’s all hopeless and what’s the point?” If one catastrophises, one has less ability to deal with pain, and catastrophisation is a powerful predictor of poor pain management The reverse is true. If one stops catastrophising then pain decreases Example: “My pain is difficult to manage, but I can cope and deal with it” Catastrophising is not uncommon and will make it more difficult for the injured person to show resilience Social support and resilience Helpful social support protects against adversity Social networks act as a protective factor in a direct manner, for instance, by providing access to information or by enhancing motivation to engage in adaptive behaviors. Social support can also influence a person positively by encouragement to adhere to treatment recommendations, maintain health promoting behaviors such as exercise and a regular and balanced diet, or to provide support such as giving a ride to someone who needs to keep a medical appointment or shop for food What factors are related to resilience in people who have a neurological-based speech disorder, that is, stuttering? First,…. Stuttering imposes a significant mental health burden or adversity 1.4 SCL-90 scores 1.2 1 0.8 Stuttering Controls 0.6 0.4 0.2 0 SOM OC IS DEP ANX HOS PA PI PSY GS Mood states Tran, Y., Blumgart, E., & Craig, A. (2011). Subjective distress associated with chronic stuttering. Journal of Fluency Disorders, 36, 17-26. Further, prevalence of social phobia is high in this population: Our data indicates a social phobia prevalence of 46%, in comparison to 4% in non stuttering control group Blumgart, E., Tran, Y., & Craig, A. (2010). Social anxiety disorder in adults who stutter. Depression and Anxiety, 27, 687-692. So stuttering involves significant adversity! What factors are related to resilience in people who stutter? We studied 200 adult people who had a diagnosed stutter We defined resilience in this study as exhibiting a low level of global psychopathology (measured by the SCL-90-R) Craig, A., Blumgart, E., & Tran. Y. (2011). Resilience and stuttering: factors that protect people from the adversity of chronic stuttering. Journal of Speech, Language, and Hearing Research, 54, 1485-1496. Resilient and non-resilient sub-groups Age (yrs) Mean (SD) Age (yrs) diagnose d Mean (SD) %SS Mean (SD) LAQ I LAQ II Mean (SD) Mean (SD) Resilient (n=76) 47.8 (16) 5.6 (2.6) 3.5 (2.6) 13.4 (6) Non resilient (n=124) 44.3 (16) 5.8 (2.8) 3.8 (2.9) 15.8 (7) NOTE stuttering frequency or %SS (higher scores indicate greater severity), health risks (LAQ1: higher scores indicate higher levels of risk), self-efficacy (LAQ2: higher scores indicate poor self-efficacy), social support (SOS: lower scores indicate poorer social support) global psychopathology score (GSI: higher scores indicate more severe psychopathology) SOS Mean (SD) GSI Mean (SD) 16.8 (9) 25.0 (4.3) .23 (.18) 25.1 (14) 22.6 (5.2) 1.47 (.58) Using regression analysis, resilience factors found in people with a neurologically related speech disorder consisted of: Protective factors Nature of the contribution Minor protective factors Severity of the disorder ……….. Annual income ………………… Vitality ………………………… General health …………………. Physical role …………………… Lower severity: increased resilience Higher income: increased resilience Higher vitality (or low fatigue): increased resilience Better health: increased resilience Greater physical function: increased resilience Major protective factors Self-efficacy …………………… Helpful social support …………. Social integration ……………… High self-efficacy: increased resilience Greater social support: increased resilience Greater social activity: increased resilience I doubt if anyone here would question the assumption that neurological injury is associated with significant adversity!! As an example, people with spinal cord injury face very substantial adverse conditions when dealing with their injury and impairment For instance, our research has shown lowered quality of life in people with SCI… Difference between Australian age and sex standardised norms with people with SCI who have low and high levels of self-efficacy (SE) on the eight SF-36 QOL domains Source: Middleton, Craig & Tran (2007). Archives Phys Med Rehab, 88, 1643-1648 90 80 QOL SF-36 70 60 Low SE SCI group sign. diff to the other two groups in all domains p<.05 50 40 30 20 High SE SCI group only sign. diff to Australian norms in three domains p<.05 phys fn phys role pain Aust norms health vitality low SE SCI social fn emot fn High SE SCI mental health …and elevated risks of depressive mood and anger Almost 50% have risks of depression after many years of living in the community, … …and adults with SCI have over nine times the risk of having increased levels of anger or irritability Chronic fatigue is also a high risk in people with injury Wijesuriya, N., Craig, A., Tran, Y., & Middleton, J. (2012). Fatigue and anger in people with spinal cord injury. Australian Journal of Rehabilitation Counselling, 18, 60-65. Fatigue negatively influences neural activity: this is seen in the impact on brain activity of non injured people. It involves a global reduction in theta and alpha activity, and an increase in beta activity Craig , et al., (2012). Psychophysiology, 49, 574-582. Alert Theta Alpha 1 Alpha 2 Beta fatigue db We estimate that around 50% of adults with SCI (and TBI) have a major problem with fatigue, and that high fatigue levels place one at risk of depressive mood (and vice versa), and thus less likely to be resilient Source: Wijesuriya, Tran, Middleton & Craig (2012). Archives Phys Med Rehab, 93, 319-324 We have also shown that adult people with SCI tire significantly after participating in a 2-3 hour mental task compared to able-bodied matched controls. Those wih elevated depressive mood (and therefore less resilient) will be more likely to fatigue excessively (see below) Craig, A., Tran, Y., Wijesuriya, N., & Middleton, J. (in press). Fatigue and tiredness in people with spinal cord injury. Journal of Psychosomatic Research. What factors contribute to resilience in a large group of newly injured adults with SCI? N=70, mean age 42 years Preliminary results: Major protective factors 1. Self efficacy: stronger self efficacy, greater resilience (explains 14%) 2. Mood: more positive mood , greater resilience (explains 19%) Minor protective factors 1. Age: higher age, better resilience (explains 1-2%) 2. Severity: lower severity, better resilience (explains about 1%) 3. Cognitive capacity: higher capacity, better resilience (explains about .2%) Interventions that enhance resilience Nurturing resilience (Rees, 2012) Develop a rewarding and pleasant events schedule Plan for appropriate work experience options Make sure there is a anchor person who is a constant (eg. family member, caregiver, health professional) Regular professional consultation available that is ongoing (eg. psychologist) Employ helpful and optimistic language Develop a social network with peer support Engage in challenging cognitive activities (eg. writing, reading) Interventions that enhance resilience My feeling is that treatment very likely to enhance resilience should: • • • • • • • • significantly enhance self-efficacy enhance social support and integration result in helpful rational thinking teach adaptive coping skills provide vocation support (eg return to work) teach problem solving enhance family and caregiver support others? The following slides present outcome results from clinical trials we have run with adults with SCI These findings suggest that resilience has been enhanced Treatments used have involved a mix of mental and behavioural skills that address anxiety, poor mood, fatigue, social integration, and so on. 1.9 1.7 1.5 1.3 Treatment 1.1 Control 0.9 0.7 0.5 3-4 weeks 6 months 12 months 2 years Clinical trial outcome for adults with SCI. Chronic pain (0=none, 2= discomfort, 3=distressing) following group CBT. Control SCI participants received usual rehabilitation care 18 16 14 depressive 12 mood Treatment Control 10 8 6 3-4 weeks 6 months 12 months 2 years 6-8 years Clinical trial outcome for adults with SCI. Depressive mood (Beck Depression Inventory where high scores indicate high depressive mood) following group CBT. Control SCI participants received usual rehabilitation care 38 36 34 32 perceived 30 helplessness 28 Treatment Control 26 24 22 20 3-4 6 12 2 years 6-8 weeks months months years Clinical trial outcome for adults with SCI. Perceived control (perceptions of helplessness where high scores indicate helplessness) following group CBT. Control SCI participants received usual rehabilitation care 20 CHALDER FATIGUE TOTAL 19 18 17 16 15 14 13 Pre Post MT GI Controlled randomised clinical trial showing change in levels of fatigue (high scores indicate high fatigue) in adults with SCI who received massage versus visualisation over 5 weeks 14 McGILL PAIN 12 10 8 PRE POST MT GI Controlled randomised clinical trial showing change in levels of chronic pain (high scores indicate high pain) in adults with SCI who received massage versus visualisation over 5 weeks When French impressionist painter Auguste Renoir (1841-1919) was confined to his home during the last decade of his life, Henri Matisse was a close friend and visited him daily. Renoir, almost paralyzed by arthritis, continued to paint in spite of his infirmities. One day as Matisse watched the elder painter work in his studio, fighting torturous pain with each brush stroke, he blurted out: “Auguste, why do you continue to paint when you are in such agony?” Renoir said: “The pain passes but the beauty remains.” So, Renoir continued to put paint to canvas. Below is one of his paintings, Tilla Durieux , completed 5 years before his death, 13 years after he developed the disease. Thank you