Evaluation Techniques
advertisement

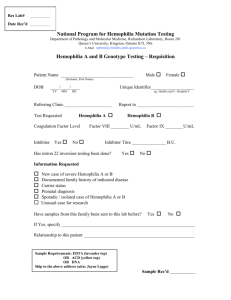
Elizabeth Bell Julene Clarke Sierra Perez Nicole Williams HSC 440 Evaluation Techniques Goal: Provide accurate and helpful information to the parents of children that are affected by blood disorders. Unit I: Anemia Unit Objective: By the end of the unit, the parents will be able to interpret their child’s condition of anemia. Instructional Objectives (Enabling Objectives): By the end of the lesson, the parents will be able to: 1.1 Know what the definition of anemia. 1.2 List the symptoms of anemia. 1.3 Interpret the diagnosis of anemia. 1.4 Identify risk factors of anemia. 1.5 Identify two complications of anemia. 1.6 List two methods to treat anemia. 1.7 Identify three foods that are good for anemic children. 1.8 List three foods that affect the body’s consumption of iron. Unit II: Sickle Cell Disease Unit Objective: By the end of the unit the parents will be able to interpret their child’s sickle cell disease (SCD). Instructional Objectives: By the end of the lesson, the parents will be able to: 2.1 Interpret the different types of SCD. 2.2 List why SCD is problematic. 2.3 Identify three symptoms of SCD. 2.4 Determine how SCD is tested. 2.5 Determine what treatments are available for SCD. Unit III: von Willebrand Disease Unit Objective: By the end of the unit, the parents will be able to interpret the diagnosis of von Willebrand disease (vWD). Instructional Objectives (Enabling Objectives): By the end of the lesson, the parents will be able to: 3.1 Define vWD. 3.2 Identify two possible complications of vWD. 3.3 Interpret the von Willebrand factor (i.e. factor VIII). 3.4 Distinguish between the three major types of vWD (Types 1, 2, and 3). 1 3.5 Prepare medical history to report to the doctor. 3.6 Appraise diagnostic tests. 3.7 Critique the different treatment options. 3.8 Select the best treatment option for your individual case. Unit IV: Leukemia Unit Objective: By the end of the unit the parents will be able to identify how to care for the child with leukemia. Instructional Objectives (Enabling Objectives): By the end of the lesson, the parents will be able to: 4.1 Define leukemia. 4.2 Determine the main types of leukemia. 4.3 Explain the causes of leukemia. 4.4 Explain the symptoms of leukemia. 4.5 Assess leukemia treatments. 4.6 Assess what happens after leukemia treatment. Unit V: Hemophilia Unit Objective: By the end of the unit, the parents will be able to analyze the blood disorder Hemophilia. Instructional Objectives (Enabling Objectives): By the end of the lesson, the parents will be able to: 5.1 Define hemophilia. 5.2 Determine how hemophilia is “inherited”. 5.3 Describe what platelets are. 5.4 Schedule physical exams and blood tests. 5.5 Compare the two types of hemophilia (Types A or B). 5.6 Distinguish the difference between the severities of hemophilia. 5.7 Plan for a pregnant woman (that is a carrier) to be diagnosed as early as 12 weeks into pregnancy. 5.8 Assess a “preimplantation diagnosis”. 5.9 Critique the different treatment options. 5.10 Select the best form of treatment for you. 5.11 Assess immunization options for children that have hemophilia. Unit VI: Alpha Thalassemia Unit Objective: By the end of the unit, the parents will be able to comprehend the blood disorder alpha thalassemia. Instructional Objectives (Enabling Objectives): By the end of the lesson, the parents will be able to: 6.1 Define thalassemia. 6.2 Define alpha thalassemia. 6.3 Select 5 symptoms of alpha thalassemia in children. 2 6.4 List 5 complications of alpha thalassemia in children. 6.5 Differentiate among the various forms of alpha thalassemia. 6.6 Interpret how alpha thalassemia is diagnosed. 6.7 Recall the types of treatment for alpha thalassemia. MULTIPLE CHOICE: Please select the best answer for each question. 1. (6.1) Thalassemia is a blood disorder that: A. B. C. D. Is an inherited. Is a disorder that affects the way the body makes hemoglobin. Causes RBCs to be destroyed at a faster rate. All of the above 2. (6.2) What is alpha thalassemia? A. Alpha thalassemia is when the body has a problem producing alpha globin. B. Alpha thalassemia is when the body is missing the four genes that make alpha globin protein chains. C. Both A and B. D. None of the above. 3. (6.3) Select the symptoms of alpha thalassemia in children. A. B. C. D. E. Anemia Fatigue, weakness, or shortness of breath Pale appearance or jaundice Swollen abdomen All of the above 4. (6.4) Select the possible complication of alpha thalassemia in children. A. B. C. D. E. Slower growth rates Infections Enlarged spleen Excess iron All of the above 3 5. (6.5) Which of the following is NOT a form of alpha thalassemia? A. B. C. D. E. Alpha thalassemia silent carrier Alpha thalassemia major (hydrops fetalis) Alpha thalassemia minor (alpha thalassemia trait) Alpha thalassemia medious (alpha thalassemia transitional) Hemoglobin H disease 6. (6.6) Which of the following is NOT a used to diagnose alpha thalassemia? A. B. C. D. Urine test Chorionic vilius sampling Amniocentesis Blood tests 7. (6.7) Which of the following is NOT a treatment for alpha thalassemia? A. B. C. D. Blood transfusions Bone marrow transplant Iron chelation therapy Folic acid supplements 8. (1.1) Anemia is a condition in which your blood has a lower than normal number of red blood cells. A. True B. False 9. (1.3) Anemia can be diagnosed by: medical and family history a physical exam a blood test. A. True B. False 10. (1.4) All of the following are risk factors of anemia except A. B. C. D. E. A diet that is low in iron Blood loss from surgery Communicable illness Long-term infections Family history of inherited anemia 4 11. (1.5) What are the two complications of Anemia? A. B. C. D. Headache and ringing in the ears Mood swings and pale skin Impair growth and short attention span Increased alertness and common cold 12. (1.7) Food that are good source of iron for anemic children are: A. B. C. D. E. Liver Fortified cereals Spinach Eggs All of the above 13. (1.8) Foods that affect the body’s consumption of iron: A. B. C. D. E. Fish Antacids Milk Both b and c None of the above 14. (1.6) List two common methods to treat anemia: A. _________________ B. _________________ 15. (1.2) List four common symptoms of anemia: A. B. C. D. E. _________________ _________________ _________________ _________________ _________________ 5 (2.1) Match the types of SCD, common and rare. 16. HbSS ____________ 17. HbSE ____________ 18. HbSD ____________ 19. HbSS ____________ 20. HbSC ____________ 21. HbSO ____________ 22. (2.2) List the reasons why SCD is problematic. A. B. C. D. E. _________________ _________________ _________________ _________________ _________________ 23. (2.3) SCD Symptoms are: A. B. C. D. E. Chest pain Stomach pain Fatigue and Shortness of breath Bone Pain All of the above 24. How is SCD tested? A. B. C. D. E. A blood test Family history Blood oxygen saturation Complete blood count (CBC) All of the above 25. (2.5) All of the treatments are used of SCD, except for A. B. C. D. Blood transfusions Folic acid Supplements Pain medicines Plenty of fluids 6 26. (3.1) Von Willebrand Disease A. B. C. D. E. Is a disease of the Willebrand factor Is a man with a disease Has nothing to do with blood Can kill you Both A and D 27. (3.2) Von Willebrand Disease A. B. C. D. E. Can mean your Willebrand factor is missing Can mean your blood is too thick Can mean your blood is missing Can mean your Willebrand factor is damaged Both A and D 28. (3.3) The Von Willebrand factor is involved in homeostasis and causes von Willebrand Disease A. True B. False 29. (3.7) For women it is bad to use contraceptives to help treat this blood disorder A. True B. False Fill in the blank 30. (3.4) People who have ____________ have low levels of von Willebrand factor 31. (3.4) People who have ____________ the Willebrand factor doesn’t work well 32. (3.4) People who have ____________ there is no Willebrand factor in them 33. (4.1) Leukemia is a cancer in the bone marrow and lymphatic system A. True B. False 7 34. (4.1) Leukemia forms abnormal A. B. C. D. White blood cells Red blood cells Palates None of the above 35. (4.4) Swollen lymph nodes are not a symptom of leukemia A. True B. False 36. (4.2) The most common type of leukemia in children is A. B. C. D. Acute lymphocytic. Acute myelogenous Chronic lymphocytic Chronic myelogenous 37. (4.2) This type of leukemia mainly affects adults A. B. C. D. Acute lymphocytic Acute myelogenous Chronic lymphocytic Chronic myelogenous 38. (4.5) Which of these is NOT a treatment for Leukemia A. B. C. D. E. Medication Meditation Chemotherapy Radiation therapy Transplant Fill in the blank 39. (4.3) Leukemia can be caused by both ________ factors and _______ factors. 40. (4.2) _________ leukemia occurs over time and almost never affects children. 41. (4.2) _________ leukemia occurs suddenly and mostly occurs in adults. 42. (5.1) A rare bleeding disorder that occurs when the blood doesn’t clot normally is called ____________ 43. (5.3) ____________ are small blood fragments that form in the bone marrow 8 (5.4) Match the Blood Test to its description 44. Prolonged Partial Thromboplastin Time (APTT) 45. Normal Prothrombin Time (PT) 46. Platelet Count 47. Bleeding Time 48. Reduced factor VIII activity 49. Factor VIII mutation analysis A. Tests how long it takes for a blood to clot. B. Tests how long it takes for the plasma portion of your blood to clot. C. Tests the small blood vessels in your skin to see how fast they close to stop the bleeding. D. A test that counts the amount of platelets in your blood. E. This test consists of a gene sequencing; taking a look at the affected/mutated factor VIII gene. F. This test measures the activity level of the factor VII Fill in the blank. 50. (5.5)_________Considered to be missing or have low levels of factor VIII. 51. (5.5)_________Considered to be missing or have low levels of factor IX. 52. (5.7) Women who are carriers for the ___________gene can be tested at the 12-week mark. 53. (5.8)______________is a procedure that takes the sperm from the dad and the egg from the mom; then fertilize in a lab where the embryos are tested for hemophilia 54. (5.2) Is Hemophilia “inherited” form a parent through an abnormal gene? A. True B. False 55. (5.9) Involves a concentration of vWF and factor VIII that is administered into your arm via a vein A. B. C. D. E. Replacement Therapy Desmopressin Antifibrinolytic Medicines Gene Therapy Treatment of Specific Bleeding Sites 9 56. (5.9) Is a man- made hormone that treats people with mild cases of hemophilia A. B. C. D. E. Replacement Therapy Desmopressin Antifibrinolytic Medicines Gene Therapy Treatment of Specific Bleeding Sites 57. (5.9) Aminocaproic acid or tranexamic acid. A. B. C. D. E. Replacement Therapy Desmopressin Antifibrinolytic Medicines Gene Therapy Treatment of Specific Bleeding Sites 58. (5.9) Not an accepted treatment option, it is still in the research stages, but is being used in clinical trials. A. B. C. D. E. Replacement Therapy Desmopressin Antifibrinolytic Medicines Gene Therapy Treatment of Specific Bleeding Sites 59. (5.9) Pain medicines, steroids, and physical therapy can all be used to reduce pain in affected joints A. B. C. D. E. Replacement Therapy Desmopressin Antifibrinolytic Medicines Gene Therapy Treatment of Specific Bleeding Sites 60. (5.10) Desmopressin is given to raise the body’s factor VIII hormone levels A. Mild hemophilia B. Moderate hemophilia C. Severe hemophilia 10 61. (5.10) Replacement therapy will be needed only when bleeding is present or there is a possibility that bleeding will occur (physical activities A. Mild hemophilia B. Moderate hemophilia C. Severe hemophilia 62. (5.10) Need replacement therapy to prevent bleeding in the joints, muscles, or other parts of the body. (Started in patients at a young age and most likely lasts through their entire life). A. Mild hemophilia B. Moderate hemophilia C. Severe hemophilia Essay Question 63. (5.11) What are immunizations options for children with hemophilia? 64. (5.6) Compare the differences between the severities of hemophilia. 11 65. (4.6) Describe the problems that can happen after treatment for leukemia 66. (3.8) Compare the treatment options for Type 1, 2, 3 vWD. 67. (3.6) Describe what medical history and observations should be reported to a doctor when your child has vWD. 68. (3.5) Compare and contrast between the three major types of vWD. 12