Critical appraisal of opioids
advertisement

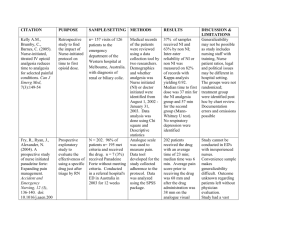
Critical Appraisal Louis Muller October 2009 EBM – Hierarchy of Evidence Prospective Cohort study • Definition: Prospective – a study that collects data after the study begins Cohort – a group of similar individuals A study that follows over time a group of similar individuals who differ with respect to certain factors under study. In order to determine how these factors affect rates of a certain outcome Prospective Cohort study Prospective Cohort Study Outcomes after Intravenous Opioids in Emergency patients: A Prospective Cohort Analysis Acad emerg med – June 2009 Vol 16, No 6 OBJECTIVES • To measure the outcomes following administration of IV opioids • To identify clinical factors that may predict poor analgesic outcomes in these patients METHODS Methods: In this prospective cohort study, emergency patients were enrolled if they were prescribed IV morphine or hydromorphone (the most commonly used IV opioids in the study hospital) as their initial analgesic. Patients were surveyed at the time of opioid administration and 1 to 2 hours after the initial opioid dosage. They scored their pain using a verbal 0–10 pain scale. The following binary analgesic variables were primarily used to identify patients with poor analgesic outcomes: 1) a pain score reduction of less than 50%, 2) a postanalgesic pain score of 7 or greater (using the 0–10 numeric rating scale), 3) the development of opioid-related side effects. Logistic regression analyses were used to study the effects of demographic, clinical, and treatment covariates on the outcome variables RESULTS • Results: A total of 2,414 were approached for enrollment, of whom 1,312 were ineligible (658 were identified more than 2 hours after IV opioid was administered and 341 received another analgesic before or with the IV opioid) and 369 declined to consent. • A total of 691 patients with a median baseline pain score of 9 were included in the final analyses. • Following treatment, 57% of the cohort failed to achieve a 50% pain score reduction, 36% had a pain score of 7 or greater, 48% wanted additional analgesics, and 23%developed opioid-related side effects. • In the logistic regression analyses, the factors associated with poor analgesia (both <50% pain score reduction and postanalgesic pain score of ‡7) were • the use of longacting opioids at home, administration of additional analgesics, provider concern for drug-seeking behavior, and older age. • An initial pain score of 10 was also strongly associated with a postanalgesicpain score of ‡7. • African American patients who were not taking opioids at home were less likely to achieve a 50% pain score reduction than other patients, despite receiving similar initial and total equianalgesic dosages. CONCLUSIONS • Conclusions: Poor analgesic outcomes were common in this cohort of ED patients prescribed IV opioids. • Patients taking long-acting opioids, those thought to be drug-seeking, older patients, those with an • initial pain score of 10, and possibly African American patients are at especially high risk of poor analgesiafollowing IV opioid administration Why was study done? • Over 40% of ED visits related to pain – US • Inadequate pain relief continues to be common • Many studies – documented failings in the processes of ED pain Mx • In Multicenter sample – NY only 60% of pts with mod to severe pain received any analgesia and median delay was 90min. Why was study done? • Use of IV opioids = the provider ID the presence of significant pain and is attempting to reduce pain in the MOST AGGRESSIVE MANNER POSSIBLE • HOWEVER – little is known about the clinical outcomes resulting from the admin of opioids in diverse ED pt population – OBJECTIVE 1 Why was study done? • Several risk factors for poor analgesic prescribing practices have been identified in ED pts. (older age, race, female sex, ED overcrowding) • However little is known about which clinical factors might predict clinical outcomes following IV opioids. – OBJECTIVE 2 Was a control group used? • Is it possible, in this specific study? – Opioid vs placebo ? (unethical) – Opioid vs NSAID ? Changes the objective ? Different design! • Home-opioid vs no home-opioid use – Only retrospective finding Design • Are the aims clearly stated? Yes • Is the design appropriate to the stated aims? – Could these aims have been studied by a different design? Should this study have been done by RCT? – Unethical / impossible / impractical – Paracetamol vs opioid (would change the objective of study) – Also too many variables in patient population ( Renal colic vs fractured limb) – In RCT – strictly speaking – should the groups be identical apart from the intervention Design • Was study ethical? – Yes – doing the study did not change the normal patient management in ED. – Informed consent Design/Method • Was the sample size justified? – Study conducted in ED with 93 000 annual visits. – Study over 29 month period (232 500) – 2414 pts approached (0.01%) – 691 in final analysis ( 0.002%) – How many pts receive opioids/yr ? – Missed many patients ! (diagram) Design/Method • How were subject recruited? Inclusion and exclusion criteria? – Enrollment occurred between July 2004 and November 2006 – Trained ED enrollers present in ED 8 am to midnight ( screened triage diagnoses, alert by nurses and providers) – Eligible for inclusion: >18yrs and received IV opioid within 2hrs of enrollment as initial analgesia. – Exclusion criteria: prior other analgesia received in ED or via EMS, cognitive fx imp, unstable vital signs, unable to communicate in English Methods • What outcomes were measured and how? – Analgesic outcome • Pain score before and after analgesics (1-2hrs post dose) • Standard verbal 0-10 numeric rating scale • Poor outcome – (3) – Development of opioid-related s/effects • Documented in chart/orders for naloxone/vital Sx • Reported by the subject or nurse Methods • Are the measurements likely to be reliable and valid? Was the intervention accurately measured? – verbal pain scoring system – validated/accepted but not as good as written/diagram – pain perception vs personalities, but trend not affected? – timing of post analgesia survey will not be exactly the same for every patient ( within 1-2hrs) – Did use 7 as a cut off. – Probably reliable and valid Design / Analysis • Are the statistical methods described? – Kruskal-Wallis test for continuous variables – the Fisher exact test was used for categorical variables. • Were the basic data adequately described and do the numbers add up? – confusing/don’t think so (table 1) Results • Only 29 % of patients approached, included in final analysis – – – – median age = 40 initial pain score = 9 60% female 32% taken opioids < 48hrs Results • Opioid dosage – Mean initial was 4.0 Mmg or 0.055Mmg/kg when adjusted for weight – Hydromorphone – higher equianalgesic dose of 6.7Mmg or 0.098 Mmg/kg • Postanalgesic pain score – mean of 87 min after initial dose – 57% of pt’s provided preanalgesic pain score AFTER initial dose (comparison revealed no difference) Results • Analgesic outcomes – 57% failed to achieve a 50% pain score reduction – 36% pain score of 7 or greater – 23% developed at least 1 s/effect – 48% wanted additional analgesics Results • Demographic, clinical and treatment characteristics of the cohort according to analgesic outcomes are presented in table 1. – – • difficult to interpret Population not broken down very well? Characteristics substantially associated with poor analgesic outcome. 1. 2. 3. 4. 5. 6. African American race Initial pain score of 10 Home opioid use History of chronic medical disease Provider concern for drug seeking Admin of additional analgesics Results • Comparison of outcomes - based on home opioid status (table 2) pt’s taking long acting opioids received substantially higher doses 0.09 Mmg vs 0.06 Mmg Despite this – poor analgesic outcomes 80% - less than 50% PS reduction 62% - postanalgesic PS more 7 What do the main findings mean? • Most pt’s in this cohort failed to achieve good analgesia, after receiving IV opioids • Several clinical variables were associated with failure to achieve good analgesia. – Should we have a more aggressive approach to patients with these high risk markers? – Needs further study. Limitations • Dosing –inadequate? Morphine - 0.1mg/kg Further studies to identify optimal opioid dosing strategy for ED patients is needed. • Sample size – 29% ( final analysis) – good representation? • Pain scoring system very subjective. (different thresholds and personalities etc.) Is there any other way to evaluate pain? • Should they have done another follow up on pain score? • Can results be generalized? Do ED patients really differ from centre to centre? • Results biased by patient selection factors. (female vs male, type of pain etc.) • Practically very challenging study to do. – enrollers missed many patients – maybe study on specific injuries/type of pain could be considered. Less variables. More focused? Implications for our practice? • Different patient population – HIV/TB vs rest • Do HIV and TB affect bodies response to opioids? • Ritonavir decrease morphine effect. • Opioids – the gold standard. More aggressive use? • Opioids vs combinations? • We probably have a higher rate of analgesia failure. (1ste world study vs our overcrowded, short staffed ED)