Chemistry PPT Flashcards Unit 1
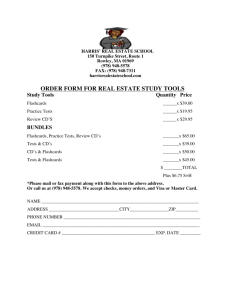
advertisement

Chem PPT Flashcards, Unit 1 Hospital laboratory providing all high-volume and emergency testing is ___. Laboratory medicine is a component of Laboratory medicine is involved in the selection, provision and interpretation of ___ and ___. Laboratory testing is a process conducted in a ___. Laboratory testing is used for the following purposes: Core laboratory Laboratory Science Diagnostic testing and individual specimens. Clinical laboratory Rule a diagnosis in or out, select and monitor disease treatment, provide a prognosis, screen for a disease, determine the severity of and monitor a physiological disturbance. Molecular diagnostics is the use Prevention, diagnosis, follow-up or prognosis of a disease and of molecular biology selection, optimization, monitoring of therapies. techniques for the following reasons: In the clinical laboratory, the Proficiency testing, auditing, Benchmarking, Clinical governance purpose of quality control is: Which 3 facets of laboratory 1. analytical testing medicine can be attained with 2. use of clinical decision making informatics the use of telemedicine and tele-healthcare? What are some of the tools and - chemical testing methods in clinical chemistry - genetic testing that are now used in other areas - molecular testing of laboratory medicine? - cancer diagnostics - infectious disease testing - identity testing What is the purpose of For prevention, diagnosis, prognosis, follow-up of disease. molecular diagnostics? What does PCR stand for? Polymerase chain reaction What are ethics? Are the rules or standards governing the conduct of an individual or the members of a profession. What are ethical issues in Confidentiality of genetic information laboratory medicine? Confidentiality of patient medical information Allocation of resources Code of conduct Publishing issues Conflict of interest What are confidentialities? Genetic information Patients’ medical information What is allocation of healthcare Best use of time resources? Cost vs. quality What are publishing issues? Fraud 1 Chem PPT Flashcards, Unit 1 Plagiarism Falsification/fabrication of data Conflicts of interest What is the future of laboratory medicines? What are the role of guidelines in method evaluation? What are the medical usefulness criteria? What are the analytical performance criteria? Other practical criteria are: What is a Frequency Distribution What is a Histogram What is a Nonparametric Approach to statistics What is a Population What is a Sample How many pieces of data are needed to begin developing reference ranges. True or False Probability and Probability Distributions do not require a large sample size to be accurate. Full of promise but also challenges Explosion of insight into disease and treatment Responsibility to stay up to date and behave ethically Clinical and Laboratory Standard Institute. International Organization for Standardization (ISO) Meeting laboratory accreditation requirements. Turnaround time. Clinical utility. Sensitivity. Specificity. Precision. Accuracy (trueness). Analytical range. Detection limit. Analytical specificity. Instrumentation. Principle of the assay and protocol for performing the test. Composition and stability of reagents and reference materials. Technologist time and required skills. Possible hazards and appropriate safety precautions. Specimen / instrument requirement and limitations. a table that displays the frequency of various outcomes in a sample, these entries on the table contain the count of occurrences of what is being measured within a particular group, displaying the distribution of values in the sample. a graphical device for displaying a large set of data. Statistics not based on parameterized distributions. in other words this type of statistics has no dependence on a specific set of parameters. is the complete set of all observations that might occur as a result of performing a particular procedure according to specified conditions. group of observations that has actually been selected from the population. There is a need for proper selection of sample 20 False, a large sample size is required for accuracy of probability and probability distribution. A large sample size will provide many data in which to form different conclusive statements. 2 Chem PPT Flashcards, Unit 1 What are Parameters? What is a median? What is a population mean? What is population variance? What is population standard deviation? What are statistics? What is random sampling? What is the Gaussian Probability Distribution? What is an example of the Gaussian Probability Distribution? -What is required for Gaussian distributions and is randomly used in significance tests. -What is the relationship between instrument signal vs. concentration of analyte? The precision depends on stability of instrument response for given analyte. -Closeness of agreement between large-series average and true values. -Evaluated by comparison of measurements given (field) method and a reference method. -This s caused by instrument or 1) Descriptive measures of a population It is a constant that describes some particular characteristics of a population. An alternative parameter that indicates the central tendency of a population, defined as the 50th percentile. The parameter most commonly used to describe the central location of a population A parameter describing the dispersion of values about the population mean. The positive square root of the population variance, frequently used to describe the population dispersion in the same units as the population value 1) Descriptive measures of the sample. Values calculated from the observations in sample 1) Each member of the population has an equal chance of selection throughout the population. Precaution to ensure random sampling 1) Symmetrical distribution of errors Parametric approach Student t Probability Distribution Calibration Trueness and Accuracy Drift 3 Chem PPT Flashcards, Unit 1 reagent instability overtime so hat calibration becomes biased. -Must be closed to zero top ensure unbiased results. Referring to qualitative concept, define closeness of agreement of mean value with “true value”. Referring to quantitative measurement, define a measure of the systematic error. Referring to qualitative concept, what term defines repeatability (within run), intermediate precision (long term) and reproducibility (interlaboratory)? Referring to quantitative measurement, define a measure of the dispersion of random errors. Define closeness of agreement of a single measurement with “true value”. Definition for comprising both random and systematic influences. What is caused by instrument or reagent instability overtime so that calibration becomes biased? What must be ensured in a carryover to ensure unbiased results? True or False: Trueness is a qualitative concept. Trueness is defined as closeness of agreement of _____ value with “true value”. True or False: Precision is a quantitative measure. Precision is associated with ___________ and __________ Define Accuracy. Carryover Trueness Bias Precision Imprecision Accuracy Error of Measurement Drift Assay carryover must be close to zero. True Mean False Repeatability and reproducibility. Accuracy is a qualitative concept that is closeness of 4 Chem PPT Flashcards, Unit 1 A measure of the systematic error is _________. A measure of the dispersion of random errors is defined as? Error of measurement is defined as a quantitative measure that comprises both ________ and systematic influences. Define Precision. agreement of a single measurement with “true value”. Bias Imprecision Random Closeness of agreement between independent results under set conditions True True or False: Imprecision of measurements is solely related to the random error of measurements and has no relation to the trueness of measurements. Closeness of agreement Repeatability between results of successive measurements carried out under the same conditions is defined as? Define Reproducibility. Closeness of agreement between results of measurements performed under changed conditions of measurements. ______ refers to the Linearity relationship between measured and expected values over the range of analytical measurements. Presence of linearity is a Trueness prerequisite for a high degree of ________. What does analytical sensitivity Capacity of a method to detect small variations in the mean? concentration of analyte True or False: Analytical True sensitivity is often expressed as the slope of the calibration curve. Analytical sensitivity depends SD ; slope on the ratio between the _____ of the calibration function and the ______. What does analytical sensitivity Precision of method depend on? What are two other names for measuring interval, reportable range 5 Chem PPT Flashcards, Unit 1 Analytical Measurement Range and Limits of Quantification? What is Analytical Measurement Range and Limits of Quantification? What is Analytical specificity and interference? Give 3 examples of Analytical specificity and interference? What are 4 analytical goals? What are qualitative methods? How is comparison of measurements obtained? What are Parallel measurements? What is a Basic error model? What are examples of basic error model? What is the method comparison data model? How is the planning a method comparison study? analyte concentration range over which measurements are within declared tolerance for imprecision and bias of the method Capacity of procedure to determine specifically the concentration of target analyte despite interferences hyperlipemia, hemolysis, bilirubin, anticoagulants, antibodies, degradation products Based on principles and a hierarchy Based on biological variation Goals for bias Relation of goals to limits set by professional bodies Use in point-of-care testing Clinical sensitivity Clinical specificity Gold standard Independent reference method yielded by two different methods a set of optimal patient samples Distinguishes pure, random errors from those related to incorrect calibration and nonspecificity of the assay Sample-related random bias Calibration bias (changed in lot number) and random bias (sample specific interferences) Mistakes or clerical errors It is comparison of a routine method with a reference method, and comparison of two routine methods -Distribution of analyte concentrations -Representativeness of samples •Samples from different patients categories •Storage and treatment of samples -Comparisons of measurements taken over days -Ethical aspects Plot of differences against average results of methods What is the difference (BlandAltman) plot? What is the difference (BlandPlot of differences in relation to existing method located Altman) plot with specified within given specified limits limits? What is the regression analysis? Applied in comparing results of analytical method comparisons What are 3 examples of 1. Deming Regression Analysis Regression analysis? 2. Ordinary Least-Square Regression Analysis (OLR) 6 Chem PPT Flashcards, Unit 1 3. Nonparametric Regression Analysis (Passing-Bablok) What is Traceability? - Means of ensuring agreement between measurements from routine methods - Based on an unbroken chain of comparison measurements leading to a known reference value Reference measurement procedure selected measurement procedure routine measurement procedure What are some considerations - Pre-analytical variation for the Uncertainty Concept? - Method imprecision - Sample-related random interferences - Calibration uncertainties Bias corrections What is Sensitivity? Percentage of people with a disease correctly predicted by the test What is the formula to calculate Sensitivity = True Positive / (True positive + False negative) sensitivity? ______ is the diseased True Positive individuals who are correctly classified by the test ______ is the diseased False Negative individuals who are misclassified by the test What does specificity mean? Percentage of people without a disease correctly predicted by the test. What is formula of specificity? TN Specificity = ---------------TN + FP TN (True Negative) stands for: nondiseased individuals who are correctly classified by the test FP (False Positive) stands for: nondiseased individuals who are misclassified by the test Following are description of Dichotomous tests what type of tests? - ) Having only positive or negative results and provide qualitative results. -) Have a single sensitivity and specificity pair for a designated assay cutoff Following are description of Continuous tests what type of tests? - ) produce quantitative results. - ) Have an infinite number of sensitivity and specificity pairs, as the cutoff varies from lowest to highest decision value. Name the test that is generated Receiver-Operating Characteristic Plots by plotting sensitivity (y-axis) 7 Chem PPT Flashcards, Unit 1 versus specificity (x-axis)? When using this test, plot displays same information graphically? Following are description of what type of tests? - ) Relative measure of test performance. - ) Test performance depends on region of curve (sensitivity vs. specificity) selected for analysis. Base on probabilistic reasoning, how ROC test should be interpreted? -) Necessity of viewing results through prism of the clinical setting, and - ) Interpretation tempered by knowledge of the prevalence of the disease should be considered in ROC curve according-----------------? What does prevalence mean? -------------Obtained with the use of several techniques? What are the two types of predictive values? What are predictive tests used to for? What are the three functions used in a predictive value equation? What is the equation for the predictive value of a positive test (PV+)? Receiver-Operating Characteristic Plots Receiver-Operating Characteristic Plots Result should not be interpreted in isolation. Probabilistic reasoning Frequency of a disease in the population under scrutiny. Prevalence Fraction of subjects with positive result having the disease in question; fraction of subjects with a negative result who do not have the disease They are used to interpret dichotomous tests and continuous tests used in dichotomous manner Functions of sensitivity, specificity, and prevalence What is the equation for the predictive value of a negative test (PV-)? What is the Odds Ratio (OR)? The probability of the presence of a particular disease divided by probability of its absence. 8 Chem PPT Flashcards, Unit 1 What does the Odds Ratio reflect? What is the Likelihood Ratio (LR)? It reflects the prevalence of the disease in the population. The probability of occurrence of a specific test value given that disease is present divided by the probability of same test value if disease were absent What does LR stand for? Likelihood Ratio What is the formula to calculate Sensitivity/ 1- specificity Positive likelihood ratio (LR+)? What is the formulat to Specificity/ 1- sensitivity calculate Negative likelihood ratio (LR-)? What is the LR for quantitative The tangent slope of ROC curve tests? When calculating LR, what is Disease prevalence and other prior information not considered? What adjustment is required For best estimate of probability of disease before result is obtained? What is Bayes’ Theorem? Permits calculation of disease probability after new information is added to existing data How is Bayes’ Theorem With the use of the likelihood ratio and odds ratio applied to yield an odds ratio? What assumption does Bayes’ Test independence Theorem rest on? What is the formula for Bayes’ P(D/R) = Sensitivity x Prevalence/ Sensitivity x Prevalence + (1 Theorem? Specificity) x (1 – Prevalence) What is combination testing? Use of test panels to increase sensitivity and specificity or to decrease costs Why is calculation of There is a need for test independence performance difficult with combination testing? Why is it not beneficial to add False positive rate is expected to rise tests to a panel? What is Combination Testing? Increased value of sensitivity over specificity if curable disease with low-cost therapy is diagnosed Strategies for manipulating the order of testing Order of testing does not affect performance but may affect costs What is Sensitivity? Result with disease. What is Specificity? Result without disease. What are 2 Methods for QUADAS Assessing Diagnostic STARD Accuracy? What is QUADAS? Quality Assessment of Diagnostic Accuracy Studies Standards for Reporting of Diagnostic Accuracy. What is STARD? 1. A project designed to improve the quality of reporting of the results of diagnostic accuracy studies. 9 Chem PPT Flashcards, Unit 1 What is Evidence-Based Medicine? What is evidence-based medicine (EBM)? What is Evidence-Based Medicine and Laboratory Medicine? What are the roles of diagnostics tests? Will the diagnostic test leads to change in probability the presence of a disease? What will be the intervention after the primary diagnostic test? How does the diagnostic test impact? Is diagnostic test safe? What is the outcome? How many types are there in evidence-based laboratory medicine? How is the first type in evidence-based laboratory studied? What is the outcome in evidence-based laboratory type 2? How accuracy of diagnostic studies in evidence-based laboratory type 3 are? How does the type 4 in evidence-based laboratory be evaluated? What is included in evidence- Term introduced in 1991 Conscientious, judicious, and explicit use of best evidence Justifications for evidence-based approach Encourages innovation and change Application to laboratory medicine of the principles and techniques of EBM and clinical epidemiology Ensures that the best evidence obtained is made available to assist clinician in making the best decisions for the patient, leading to increase probability of improved health outcomes Roles of diagnostic tests Scenarios of decision-making process, each involving a question, a decision, and an action. For, example: Seeking a diagnosis Ruling out a diagnosis Making a prognosis Treatment selection and optimization Treatment monitoring Useful diagnostic test leads to change in probability of presence of a disease, but the change alone does not prompt the decision. Follow-up of testing with an appropriate intervention Value of test based on impact on patient’s health Harm done by restriction of research “Test and act” Five types of studies in evidence-based laboratory medicine Characterization of the diagnostic accuracy of tests by studying groups of patient Determination of the value of testing for people who are tested (outcome) Systematic review of studies of diagnostic accuracy or outcome of tests to answer a specific clinical question Economic evaluation of test to assess the economic value of using the test Audit of performance of tests during use to answer questions 10 Chem PPT Flashcards, Unit 1 based laboratory type 5? What other technique is used in evidence-based laboratory medicine? What is the alternative design? How many types of verification bias? What are the verification bias’ types? What is the outcome studies? What is patient outcomes? What is examples of patient outcomes? What is the usage of outcome study? What is the importance of outcome studies in medicine? How do randomized control trials (RCT) work? What are RCTs? How are RCTs regulated? What is the optimal design of RCTs? What are the several defining features of systematic reviews of diagnostic testing? What do systematic reviews of diagnostic tests require? What elements of protocol are there for diagnostic tests? What are some systematic reviews of diagnostic tests? about their use Use of computerized modeling techniques to assess costeffectiveness of tests and impact of process changes on resource utilization It is results of patients known to have the disease are contrasted with a control group. Two Differential verification bias and Spectrum bias It is the results of medical interventions in terms of health or cost (clinical, operational, economic) It is the outcomes associated with patient’s condition and experience. Mortality, morbidity, complication rates, length of stay in the hospital, waiting time, costs of care, patient satisfaction with care - Improvement of outcomes with improved test - Test as surrogate outcome marker - Value of operational and economic outcomes to care providers, purchasers, and policy makers - Differentiation of outcome studies from studies of prognosis Test attributes and studies of outcomes The requirement of proven effectiveness for drugs and the demand for effectiveness of diagnostic testing as well as to prove high quality care and show improved outcomes. Patients are randomly assigned to receive either the intervention to be tested or an alternative and an outcome is measured. A standard for studies of health effects of medical interventions. CONSORT (Consolidated Standards for Reporting Trials). It includes the evaluation of applicability of an outcome study. The explicit methodology helps ensure reproducibility with multiple objectives, to answer strictly defined clinical questions in a way that minimizes bias. Time, multiple people with multiple skills and database searches for previous studies? Title, background information, composition of the review group, a timetable, the clinical question(s) to be addressed in the review and a search strategy. 1) Inclusion and exclusion criteria for selection of studies 2)Methodology of data extraction and data extraction forms 3)Methodology of and checklist for critical appraisal of studies 11 Chem PPT Flashcards, Unit 1 What are some key steps in a systematic review of a diagnostic test? What are some strategies for search of primary literature? What is essential to do with quality review and data extraction? Who should the data be summarized and presented? What are some benefits of using meta-analysis for multiple studies? What is the Influence of laboratory testing on healthcare costs? How to work on Hierarchy of evidence ? What is the definition of Costminimization analysis? What is the definition of Costbenefit analysis? What is the definition of Costeffectiveness analysis? What is the definition of Costutility analysis? What are the Perspectives of Economic Evaluations? 4)Methodology of study synthesis 1) Identify the clinical question. 2) Define inclusion and exclusion criteria. 3) Search the literature. 4) Identify relevant studies. 5) Select studies against explicit quality criteria. 6) Extract data and assess quality. 7) Analyze and interpret data. 8) Present and summarize findings. 1) An electronic search of literature databases 2) Hand searching of key journals 3) Review of the references of key review articles Identified papers should be read independently by two persons and data extracted according to a template 1) Presented in tables 2) Data should include sensitivities, specificities and likelihood ratios 3) Summarized in plots that provides an indication of the variation among studies 4) Should also include an assessment of the quality of each study using a scoring system such as QUADAS (Quality Assessment of Diagnostic Accuracy) 1) Statistical way of analyzing data from multiple studies 2) Explore sources of variability in the results of clinical studies 3) Increase confidence in the data and conclusions 4) Signal when no further studies are necessary Costs of laboratory testing have a profound effect on medical decisions technical performance → clinical performance → clinical effectiveness → economic sense Simplest type of economic evaluation that compares the costs of alternative approaches that produce the same outcome Determines whether the value of the benefit exceeds the cost of the intervention and therefore whether the intervention is worthwhile. Looks at the most efficient way of spending a fixed budget to achieve a certain goal Focuses on the quality and the quantity of the health outcome -Patient -Provider -Payer (government health agency or health insurance company) 12 Chem PPT Flashcards, Unit 1 What is the definition of silo budgeting? What are the clinical practice guidelines? What are the Steps in developing guidelines? What is the definition of Audit? What is Clinical Audit? What are the advantages of Audit cycle? How do you apply the principle of Evidence-Based Laboratory Medicine in Routine Practice? What do reference values mean? What are the mandatory conditions in the establishment of Reference Values? What are the mandatory conditiions in the establishment of Reference Values? Society The laboratory budget is usually “controlled” independently of the other costs of healthcare Tool for facilitating implementation of findings of primary studies and systematic reviews To assists practitioner and patient decisions about appropriate healthcare for specific clinical circumstances Need for transparency to ensure integrity -Topic selection -Establishment of target group and development team -Identification and assessment of evidence -Transformation of evidence into guideline -External review and updates to guidelines Refers to the review of case histories of patients against the benchmark of current best practice Benchmarking of performance with performance indicators against performance of peers -Problem-solving -Monitoring of workload and demand -Monitoring of new tests -Monitoring variation between providers and adherence to best practices • Principles support manner in which laboratory medicine is practiced • Principles provide logic • Means of providing high-quality service Use is more complex for laboratory than for clinical medicine but still critical Results of certain type of quantity obtained from a single individual or group of individuals corresponding to a stated description, which must be spelled out and made available for use by others. Also referred to as observed values, reference interval, reference limit All groups of reference individuals should be clearly defined. The patient examined should resemble sufficiently the reference individuals in all respects other than those under investigation. The conditions under which the samples were obtained and processed for analysis should be known • All quantities compared should be of the same type. • All laboratory results should be produced with the use of adequate standardized methods under sufficient analytical quality control • The clinical sensitivity, clinical specificity and prevalence in the populations tested should be known. 13 Chem PPT Flashcards, Unit 1 What are the criteria of selection of reference individuals? What type of procedures are recommended taking into account the requirements that will enable all the constituents under study to be measured accurately? What requires preanalytical standardization? A total of twenty (20) samples from reference individuals should be analyzed and ensuring that no more than how many values for the QC fall outside the proposed limit. Considerations will include what? What are the Statistical Treatment of Reference Values? Partitioning of the reference values into appropriate groups is also known as? Reference values can be partitioned according to what? Statistical Treatment of Reference Values will give rise to narrower and more appropriate ______? Examples of Partitioning Criteria for Possible Subgrouping of the Reference Group are? What is important to do have an accurate presentation of an • Criteria should include: • Statements describing the source population • Should be randomly selected • Specifications of criteria for health • The disease of interest Standardized 1. Preparation of individuals before sample collection 2. The sample collection itself 3. Handling of the sample before analysis 2 a)Analysis method Equipment, reagents, calibrators, types of raw data, calculation method b)Quality control c)Reliability criteria I. Partitioning of the reference values into appropriate groups II. Inspection of the distribution of each group III. Identification of outliers Determination of reference limits stratification (strata), categorization (category), or subgrouping (subgroup or partition) Sex, age, and other characteristics reference intervals Age, Gender, Genetic Factor, Physiological Factor, and other factors like socioeconomic, environmental and chronobiological To have as much information provided as is possible. 14 Chem PPT Flashcards, Unit 1 observed value in relation to reference values? What observed values are recorded in relation to reference values? What mathematical equation that measures distance is used in reference ranges? Give 2 examples of a subjectbased reference value problem. Name 5 things that are true of transferability reference values. What is clinical sensitivity? What is clinical specificity? What is Predictive value? What is Prevalance? What are examples of s Subject-Based reference values be used as a reference value? Usage of reference values generated by other laboratories is an example of what kind of reference values? The Use of Transferability of reference values can be any of the followings except: a. Steps to ensure comparable analytical methods (identical calibration, quality control results b. Importance of verifying “borrowed” values before use c. Expressing observed value by a mathematical Low, usual, and high Standard deviation Inherent to population-based (Fig. 5-3) Use of subject’s own previous healthy values as reference for future values Determination of reference values beyond the scope of many laboratories; transfer solves problem Must be comparable populations Steps to ensure comparable analytical methods Use of pooled multicenter data 1. Importance of verifying “borrowed” values before use Fraction of subjects without the disease that assay correctly predicts Fraction of subjects with disease that assay correctly predicts Combination of disease prevalence with sensitivity and specificity The proportion of study population with disease The use of subject’s own previous healthy values as reference for future values. Problems inherent to population-based reference values are encountered. A Transferability of reference values C 15 Chem PPT Flashcards, Unit 1 distance measure (e.g., standard deviation) d. Use of pooled multicenter data What is Clinical sensitivity? A fraction of subjects without the disease that assay correctly predicts is a clinical: a. Clinical sensitivity b. Clinical specificity c. Predictive value d. Prevalence What is the difference between Predictive value and Prevalence? Name the six types of body fluids that may tested in the lab: In addition to whole blood, what are the five types of biological specimens collected for lab testing: The agency responsible for publishing and procedures for standardized specimen collection is: The liquid portion of clotted blood is: Serum contains fibrinogen: True or False? The liquid portion of anticoagulated blood is: Plasma contains fibrinogen: True or False? What are the 3 layers of centrifuged plasma: What does K3EDTA stand for? What does K2EDTA stand for? What are K3EDTA and K2EDTA? How does K3EDTA and K2EDTA prevent coagulation? What is this process called? What is the color code for EDTA? What is the most commonly used anticoagulant in A fraction of subjects with disease that assay correctly predicts B A Predictive value is a combination of disease prevalence with sensitivity and specificity while a Prevalence is a proportion of study population with disease Cerebrospinal, synovial, pleural, amniotic, ascitic and pericardial fluids. Serum, plasma, urine, feces, saliva. The Clinical and laboratory Standards Institute (CLSI) Serum False Plasma True Bottom is RBCs, Top is plasma and slim middle buffy layer is WBCs and platelets Tripotassium ethylenediaminetetraacetate Dipotassium ethylenediaminetetraacetate Anticoagulants By removing ionized calcium Chelation Lavender, occasionally pink or white EDTA 16 Chem PPT Flashcards, Unit 1 hematology for complete blood count or any of its component tests? Complete blood count What does CBC stand for? What are the component tests Hemoglobin, packed cell volume, total leukocyte count, for CBC? leukocyte differential count, platelet count Erythrocyte sedimentation rat What does ESR stand for? Blood grouping, rH typing, and antibody screening What is EDTA used for in blood banking? EDTA is useful for isolation of True genomic DNA and qualitative and quantitative virus determinations by molecular techniques. EDTA inhibits certain enzymes TRUE like alkaline phosphotase, CK and leucine aminopeptidase. EDTA is unsuitable for calcium TRUE and iron analyses using photometric or titrimetric techniques. By removing calcium and precipitating it into an unusable form How does sodium citrate prevent coagulation? Light blue What color is the tube for sodium citrate? Which tests use sodium citrate? APTT, PT, Westergren ESR 1 part anticoagulant to 9 parts blood What is the ratio of sodium citrate to blood? Acid citrate dextrose What is ACD? Its ability to preserve both form and function of the cellular components Why is ACD ideal for molecular diagnostic and cytogenic testing? Oxalate Which anticoagulant forms insoluble complexes with calcium ions? Greater than 3g oxalate/liter of blood At what concentration will oxalate cause hemolysis? anti-thrombin What substance inactivates blood-clotting factor thrombin and factor Xa? What is the recommended form Lithium heparin of heparin? Green What is the color code for heparin? Heparin What is the only anticoagulant that should be used for the 17 Chem PPT Flashcards, Unit 1 determination of pH, blood gases, electrolytes, and ionized calcium? Which enzyme converts fibrinogen to fibrin? Why is thrombin used in “stat” serum testing? Which dry additive is a weak anticoagulant and is primarily used in preventing glycolysis? Which 2 substances are effective at 2g/L of blood concentration? What is a potent inhibitor of urease? What are the methods of specimen collection? What are supplies and equipment of venipuncture by syringe method? What are supplies and equipment of venipuncture by vacutainer method? What are the sites of venous blood collection? What are the sites of Venous Blood Collection? What are the recommended order of draw for multiple specimen collection? Thrombin Its short clotting time Sodium fluoride Sodium fluoride and potassium oxalate Sodium fluoride 1. Venous Blood Collection (Phlebotomy or Venipuncture) Syringe Method Vacutainer or Evacuated Tube Method 2. Capillary or Peripheral Blood Collection (Skin Puncture) 3. Arterial Blood Collection (Arterial Puncture) Test requisition Tourniquet and disposable gloves Sterile disposable syringe with needle Alcohol swabs (70%) and gauge square pads Adhesive plastic strips Test requisition Tourniquet and disposable gloves Sterile disposable needles and needle holder Various evacuated blood tubes Alcohol swabs (70%) and gauge square pads Adhesive plastic strips Veins on the anticubital fossa region: 1. Cephalic vein 2. Basilic vein 3. Medial cubital vein Median vein of the arm Cephalic vein. Basilic vein. Medical cubital vein. Median vein of the arm. Yellow Royal Blue Clear/Red Light Blue Gold/Red Red/red, orange/yellow, royal blue 18 Chem PPT Flashcards, Unit 1 What are the methods of blood collection? What are the methods of capillary or peripheral blood collection? True or False Skin punctured blood is more like arterial blood than venous blood A.True B.False Possible times when one would perform the skin puncture technique for a blood sample rather than filling a tube might include: A.Sample volume is limited (eg. pediatric patients) B.Severe vein damage due to repeated puncture C.Burn patients D.All of the above Which of the following is not a proper site for skin puncture? A. earlobe B. plantar or lateral surfaces of the infant’s heel C. thumb D. big toe of infants If a phlebotomist is performing a skin puncture on a finger and the fingers are cold and white due to low blood circulation, Green Royal blue Lavender, pearl white, pink/pink, tan (plastic) Gray Yellow (glass) Patient identification. Personal protective equipment. Queries regarding fasting, medication. Proper positioning and vein and site selection. Appropriate needle, tubes, and other equipment. Timing of collection. Effects of tourniquet and stress. Test requisition. Disposable gloves and sterile small gauze squares. Sterile disposable lancets. Alcohol swabs (70%) and gauge square pads. Equipment specific for the test ordered (glass slides, micropipette, and diluent, hematocrit tubes) A D C D 19 Chem PPT Flashcards, Unit 1 what is the proper method for increasing blood flow? A. Massaging finger by gently squeezing between thumb and forefinger. B. Rubbing finger briskly between hands. C. Warm the hand by holding it under very hot hot water for 10 minutes D. Warm the area with a warm, wet washcloth or heel warmer for 3 minutes Why should a heel stick never be performed on the center of the heel? A. Because the baby may cry. B. The heel bone may be injured. C. The parents may become upset. D. It's ok to perform a heel stick in the center of the heel. Blood collected from the radial artery of the wrist, brachial artery of the elbow, and femoral artery in the groin is called.. A. Venous blood B. Arterial blood C. Capillary blood D. None of these Which type of blood vessel is used for blood gas analysis? A. Vein B. Capillary C. Artery D. B and C True or False Anybody is allowed to perform an arterial puncture to obtain blood for blood gas analysis. A. True B. False True or False Skin puncture is more like B B D B B 20 Chem PPT Flashcards, Unit 1 venous blood than arterial blood. A. True B. False PCO2 of venous blood is about _____ higher than in arterial blood. A. 1-2 mm Hg B. 11-12 mm Hg C. 6-7 mm Hg D. 5-6 mm Hg Glucose of venous blood is about 7 mg/L ____than skin punctured blood A. more B. less Skin punctured blood is more prone to contamination by.. A. bacteria B. interstitial and intracellular fluids C. dirt D. all of the above. What is Hemolysis? What is in vivo hemolysis? What is in vitro hemolysis? What are the causes of in vitro hemolysis? What are the effects of hemolysis? What is Urine used for? C B B 1) Disruption of the red cell membrane, resulting in the release of hemoglobin. Hemoglobin concentration exceeds 50mg/dL Consequence of intravascular events Subsequent to or during blood collection 1) Alcohol left on the skin 2) Use of small bore needles 3) Underlying red cell disorders 4) Extreme temperature during transport Other causes 1. False increase in the concentration of plasma lactate dehydrogenase, potassium, magnesium, phosphate and serum inorganic phosphate 2. Additional band caused by hemoglobin may be seen on serum protein electrophoresis (SPE) 3. Interferes with colorimetric methodologies 4. Interferes with the amplification reaction of reverse transcriptase in molecular diagnostic testing 1) Aside from routine urinalysis, can be used for bladder cancer screening and monitoring of therapy for bladder cancer 2) Used for molecular testing for infectious agents 21 Chem PPT Flashcards, Unit 1 (Chlamydia) or BK virus. What is part of taking a urine sample? What are the types of urine specimens? Necessity of cleaning patient’s genitalia before each voiding to minimize transfer of surface bacteria to the urine. 1) Type of specimen depends on test 2) Untimed urine specimen (random) 3) Clean, early morning, fasting specimen is most concentrated and ideal for microscopic examination and detection of abnormal quantities of constituents (e.g. chorionic gonadotropin) 4) Double-voided specimen – excreted during a timed period after complete emptying of the bladder (glucose tolerance test) 5) Forensic studies specimen – testing for the presence of alcohol or drugs of abuse collected under rigorous conditions requiring chain of custody documentation 6) Catheter urine specimens – for microbiological examinations 7) Suprapubic tap specimen – sterile specimen for microbiological examination (culture) on infants 8) Timed specimen (4-, 12- or 24 hours) -Need for prolonged collection period to minimize the influence of short-term biological variations -Importance of adherence to instructions (diet restrictions, first urine is discarded, avoid fecal contamination) What is another part of taking a urine sample? Need for mixing of specimen because of variations in specific gravity, volume, and composition throughout the collection period -The purpose for this in urine is to reduce bacterial action, reduces chemical decomposition and solubilize constituents that might precipitate out. -Immediately after collection, this is the most acceptable way of storage. -The act or process of making something sour (acidifying), or changing into an acid. This can cause precipitation of urates (unsuitable for uric acid determination). Urine Preservatives Refrigeration. Acidification 22 Chem PPT Flashcards, Unit 1 -In urine preservatives, what is used to reduce pH level? -What causes precipitation of urates? -What two preservatives are used to preserve porphyrins, urobolinogen and uric acid? -What type of sample is used to detect “parasites and ova” and “Occult blood” or presence of hidden blood for discovering the presence of a bleeding ulcer or malignant disease in the gastrointestinal tract (GIT). This type of sample is also used for meconium testing in the newborn’s feces to detect from maternal drug use during the gestational period. -This type of specimen is used for the screening for trypsin activity from infants to detect cystic fibrosis, used to characterized the a type of porphyria and also used to determine nitrogen and fat in a 72 hour specimen used to assess the severity of malabsorption. -This specimen is obtain from the lumbar region of the spine, and occasionally from cervical region, or from the cistern or ventricle of the brain. Used to rule out meningitis and demyelinating disease. -What lumbar locations is the CSF obtained from? -Who is authorized for the collection of cerebrospinal fluid? -What departments do the fallowing sterile CSF tubes belong to: Tube #1, #2, and #3 CSF glucose is simultaneously Sulfamic asid (10 g/L urine) Boric acid (5 mg/L of urine) Sodium bicarbonate or sodium hydroxide Feces Feces Cerebrospinal fluid (CSF) L3, L4 and L5 A physician Tube #1-Chemistry and Serology Tube #2-Microbiology Tube #3-Hematolgy A blood glucose test 23 Chem PPT Flashcards, Unit 1 ran with what kind of test? True or false? Antoglycolytic agents are added to CSF What can CSF give rapid identification of ? In molecular diagnostics CSF can also be used for what kind of cells (2) rearrangement associated with hematologic malignancies? What is synovial fluid? What is arthrocentesis? True or False? The technique of arthrocentesis depends on location and size of joint What can synovial fluid be used for? What kind of tube should be used for synovial fluid? What kind of tubes should be used for synovial fluid for culture, glucose and protein? What kind of tube should be used for total leukocyte, differential and erythrocyte counts for synovial fluid? Synovial fluid can be used to detect the presence of ________ ___________. What is a causative agent of Lyme disease? Staphylococcus aureus is a causative of what kind of infection? What kind of bacteria is Salmonella, Pasteruella and Pseudomonas? What is amniotic fluid? What term is used to describe the collection of amniotic fluid? True or false? Amniotic fluid can be used to indicate prenatal diagnosis of congenital disorders False Infectious agents T-cell and B-cell Joint fluid that lubricates a joint, tendon sheath or bursa Surgical puncture to remove synovial fluid True To indicate and aid characterization of the type of arthritis A sterile tube with or without preservative (depending on test to be performed) Sterile plain tubes EDTA tubes Infectious microorganisms Borrelia burgdorferi Staphylococcal infections Aerobid Gram-negative bacilli Liquid contained by the amniotic sac of a pregnant woman Amniocentesis True 24 Chem PPT Flashcards, Unit 1 True or False? Amniotic fluid can be used to indicate and asses in fetal lung maturity True or False? Amniotic fluid can’t be used to look for RH isoimmunization of intrauterine infection What kinds of disorders can amniotic fluid diagnose? How is chorionic villi removed? When is chorionic villus usually removed? How is chorionic villus observed? What kind of characteristics are you looking for in chorionic villi? True or False? Chorionic villi has the same chromosomal and genetic makeup identical as the fetus What is chorionic villi used to test for? What is serous fluid? What may an accumulation of serous fluids indicate? What can be differentiated using serous fluid? What is the method of collection for serous fluids called? Chorionic villi has the same chromosomal and genetic makeup identical to what? What is chorionic villi used to test for? What is serous fluid? Accumulation of serous fluid may signify what? How to differentiation whether fluid is an transudate (effusion) or exudate? True False Cystic fibrosis, sickle cell anemia, Tay-Sach’s disease, and thalassemia With a catheter or needle During gestation (early pregnancy) Under the microscope for quality, quantity, and integrity The quality of branching, budding, veining, and evaluation of maternal cell contamination True Inherited genetic disorders Fluid that lubricates the opposing parietal and visceral membrane surfaces Inflammation or infection Whether fluid is an transudate or exudate using protein or enzyme content analysis Paracentesis as the fetus inherited genetic disorders Fluid that lubricates the opposing parietal and visceral membrane surfaces inflammation or infection using protein or enzyme content analysis 25 Chem PPT Flashcards, Unit 1 What is the general method of collection? What cavities contain serous fluid? The fluid contained between the visceral and parietal membrane is known as what? Pleural fluid is contained between what? Pericardial fluid is located where? What is thoracentesis? What is Peritoneocentesis? What is Pericardiocentesis? How is the method testing of saliva? What are buccal cells? paracentesis Peritoneal cavity, Pleural cavity, Pericardial cavity the Peritoneal Fluid Visceral space and pleural space Around the heart Collection of pleural fluid Collection of peritoneal fluid Collection of pericardial fluid Measure of blood group substances to determine secretor status and genotype Are cells of the oral cavity, excellent source of DNA. Collected by rinsing with mouthwash and using swabs or cytobrushes. What is the solid tissue? Breast cancer tissue, testing for estrogen and progesterone receptors and have to keep freezing. How to analysis toxicologic? It means all materials used for collection or handing should be made of plastic and free of contaminating trace elements What is somatic gene analysis Detection of mutation. The tissues are usually formalin-fixed for? and paraffin-embedded (FFPE). The specimens in optimal cutting temperature (OCT) compound- mixture of polyvinyl alcohol and polyethylene glycol. The method of testing hair and They are used currently limited genomic identification, and nails also used for drug and trace metal analysis but poor standardization of assays What are procedures of Identification, preservation, separation and storage, and specimens for analysis? transport. How to maintenance of All specimens treated as if infectious; no special labeling. specimen identification? They need for adequate labeling, regardless of size or treatment of container. Preservation of specimens are Proper container and labeling, careful transport Temperature constraints Separation of serum and plasma, hemolysis Challenges of RNA recovery Remote facilities. Separation of plasma and - As soon as possible but not prematurely serum: - Room temperature storage if centrifugation not possible in normal window Freezer or cold storage after centrifugation Centrifugation with a stopper in - Prevents evaporation or aerosolization place: - Absolutely necessary for volatiles 26 Chem PPT Flashcards, Unit 1 Cryopreservation: Requirements for referring specimens to a CAP accredited referral laboratory: Controllable Pre-analytical variables include: Uncontrollable Pre-analytical variables include: What are effects of changes in posture: - Maintains anaerobic conditions pH changes induced by removal of stopper before centrifugation - Useful in preserving WBCs and DNA - Preventing shearing of DNA Thorough mixing after thawing For CAP accredited laboratories, it is a requirement that the referring laboratory validate that the referral laboratory is CLIA certified before specimens are shipped. - Physiological Variables Posture Exercise and Physical training Circadian variation Menstrual cycle Travel Diet Food ingestion Vegetarianism Malnutrition Fasting and Starvation Lifestyle Smoking Alcohol Drug Administration Prescribed medication Recreational drug ingestion Herbal preparations Biological influences Age Sex Race Environmental factors Altitude Ambient temperature Geographical location of residence Seasonal influences Underlying medical conditions Obesity Blindness Pregnancy Stress Fever Shock and trauma Transfusion and Infusion - Changes in posture result to hydrostatic efflux of water and filterable substances from the intravascular space to the 27 Chem PPT Flashcards, Unit 1 What type of physical variation causes Shifts of fluid between intravascular and interstitial compartments? Name one of the variations can cause Changes in hormone concentration in analyte? Loss of fluid due to sweating can be due to what type of variables? What does Circadian Variation refer to? What factors contributes to Circadian Variation? Give some examples of Circadian Variation? Why Menstrual Cycle is considered one of the preanalytical controllable variable? How does Travel across several time zones affect the normal circadian rhythm? How many days is required to establish a new stable diurnal rhythm after travel across 10 time zones? How does Synthetic diets affect the amount of protein in the plasma? Which plasma constituents will be increased when Diet mainly consists of starch or sucrose? Which plasma constituents will be reduced when sucrose intake is decreased? Which plasma constituents will be reduced in high carbohydrate diet? Individuals who eat many small meals throughout the day give…………….? How food ingestion is affected dependent interstitial fluid of the extracellular space Increase in potassium (0.2-0.3 mmol/L) occurs after an individual stands for 30 minutes Exercise and Physical Training Exercise and Physical Training Exercise and Physical Training The pattern of production, excretion and concentration of analytes each 24 hours posture, activity, food ingestion, stress, daylight or darkness and sleep or wakefulness Cortisol and Iron higher at 8AM and lower at 4PM Potassium higher in AM than PM Because the concentrations of plasma female sex hormones and other hormones are affected by the menstrual cycle. Due to altered pituitary and adrenal functions Five (5) days Day to day changes ALP and LD Plasma triglyceride concentration the VLDL cholesterol concentration, triglycerides and protein lower the VLDL cholesterol concentration, triglycerides and protein With the time between ingestion of a meal and collection of blood. 28 Chem PPT Flashcards, Unit 1 the concentration of certain plasma constituents? What plasma constituent are reduced in individuals who have been vegetarians for a long time? Does Vegetarianism affect both HDL and LDL cholesterol concentrations? What are some causes of malnutrition? In a fasting/starving state, what occurs to the concentration of glucose? In a fasting/starving state, what occurs to the secretion of insulin and glucagon? What is stimulated by a fasting/starving state? In a fasting/starving state, what does the body use for energy? What is the impact of nicotine on the body? Does smoking increase or decrease glucose concentrations? Does smoking increase or decrease plasma growth hormone concentrations? How are immunoglobulins affected with smoking? How does smoking affect sperm count and activity? How does alcohol ingestion affect blood glucose concentrations? What is used as a marker of persistent drinking? What is chronic alcoholism associated with? How can intramuscular drugs alter blood serum? What is recreational drug ingestion? What are some examples of LDL cholesterol, total lipids, and phospholipids Yes, In strict vegetarians, the LDL concentration may be 37% less and the HDL cholesterol concentration 12% less done in nonvegetarians Malnutrition causes reduction of total serum protein, albumin, beta globulin, complement C3, retinol binding globulin, transferrin, and prealbumin Glucose concentration decreases by as much as 18 mg/dL Insulin secretion is greatly reduced whereas glucagon secretion may double Lipolysis and hepatic ketogenesis our stimulated Keto acids and fatty acids become the principal sources of energy for muscle Nicotine increases the concentration of epinephrine in the plasma and the urinary excretion of catecholamines and their metabolites Glucose concentration increases by 10 mg/dL within 10 minutes of smoking a cigarette Plasma growth hormone concentration may increase tenfold within 30 minutes IgA, IgG, and IgM levels are generally lower in smokers, whereas IgE concentration is higher Sperm count of male smokers is reduced compared to non-smokers; number of abnormal forms is greater and sperm motility is less It increases blood glucose concentration by 20 to 50% Increased activity of gamma glutamyltransferase (GGT) enzyme is often used as a marker of persistent drinking Chronic alcoholism is associated with abnormal pituitary, adrenocortical, and medullary function Drugs administered intramuscularly can cause increased amounts of CK and LD into the serum. It refers to the ingestion of compounds for mood-altering purposes. Amphetamines increase the concentration of free fatty acids, 29 Chem PPT Flashcards, Unit 1 recreational drugs and their side-effects on the body? morphine increases the activity of amylase, lipase, ALT, AST, ALP and serum bilirubin, and cannabis increases plasma concentrations of sodium, potassium, urea, chloride and insulin but decreases those of creatinine, glucose and uric acid What types of herbs can cause Long-term use of aloe vera, sandalwood, cascara sagrda may cause hematuria and albuminuria over hematuria and albuminuria. time? Green tea has been reported to Microcytic anemia cause what? What are tonka beans known to Reversible liver damage cause? What is an uncontrollable Age; Newborn, the older child to puberty, the sexually mature adult, variable? and the elderly adult What does age have a notable Age has a notable effect on reference intervals particularly hormones effect on? What sort of changes are Characteristic usually seen after puberty between young female and male humans? What type of hormones, such as Sex hormones prolactin, become apparent? Certain biological Higher enzyme readings characteristics, such as greater muscle mass in men, can produce what type of differences in men and women? After menopause, activity of ALP what enzyme increases in women until it is higher than in men? Is total serum protein Black concentration known to be higher in people that are black or white? Is serum albumin typically less Black in people that are black or white? In_____ men, serum IgG is Black, white 40% higher, and serum IgA may be 20% higher than in ____ men One type of environmental Altitude factor? Why is it that in individuals because of reduced atmospheric PO2. living at a high altitude, blood hemoglobin and hematocrit are 30 Chem PPT Flashcards, Unit 1 greatly increased? The fasting basal concentration of ______ is high in individuals living at the high altitude, but concentrations of renin and aldosterone are decreased. What takes longer? Complete adaption to higher or lower altitudes? What can ambient temperature have an effect on? Acute exposure to heat may decrease plasma protein concentration by up to what percent? When you sweat, what is being lost? Ambient temperature may cause a decrease in plasma potassium by as much as what percent? What can you expect to see an increase in serum concentrations of in people who live in areas with hard water? In areas where there is much heavier automobile traffic, what can you expect to see an increase in? Individuals who work indoors, as opposed to those who work outdoors, will likely have a higher concentration of what? Serum concentration of cholesterol, triglycerides and beta lipoproteins are positively correlated with what underlying medical condition? Serum LD activity and glucose concentration increase in both sexes with an increase of what? In men, with increasing body weight, what else can you expect to see an increase in? In women, with increasing body weight, what else can you Growth hormone Higher Body fluids 10% Salt and water 10% Cholesterol, triglycerides, and magnesium Carboxy hemoglobin Vitamin D Obesity Weight Serum AST, creatinine, total protein and blood hemoglobin concentration Serum calcium 31 Chem PPT Flashcards, Unit 1 expect to see an increase in? Normal stimulation of what body part is reduced with blindness? In people with blindness, The normal diurnal variation of what hormone may or may not persist? As a result of reduced aldosterone secretion, plasma levels of what compounds are also reduced? In individuals with blindness, plasma glucose may be _____ and insulin tolerance is ____. During pregnancy, what type of lipids can you see an increase in? Urine volume ___ during pregnancy The glomerular filtration rate increases by what percent during the third trimester. The erythrocyte sedimentation rate increases by what fold during pregnancy. What types of stress can influence concentration of plasma constituents? What plasma constituents can anxiety stimulate increased secretion? The hypothalamic pituitary axis Cortisol Sodium and chloride Reduced, less Cholesterol, triglycerides Increases 50% Fivefold Physical and mental stress. aldosterone, angiotensin, catecholamines, cortisol prolactin renin somatotropin, TSH Vasopressin Albumin Cholesterol Fibrinogen Glucose Insulin lactate. 32 Chem PPT Flashcards, Unit 1 What is reduced in secretion during fever? T4 Which hormones are increased in excretion during fever? free cortisol 17-hydroxycorticosteroids 17-ketosteroids Corticotropin secretion is stimulated to produce a threefold to fivefold increase in the serum cortisol concentration During shock and trauma, what stimulates increase in serum cortisol concentration, and by how much? During shock and trauma, what increases excretion and secretion, respectively? 17-hydroxycorticosteroid and catecholamines Which activities are increased during shock and trauma? Aldosterone and renin activity are increased What is increased and decreased during transfusions of whole blood or plasma? What is a delta check and what is it used for? What is the reference change value? Which population is the reference change value generally higher? What are other terms for Total Quality Management (TQM)? When implementing TQM, the framework for quality management emphasizes establishment of: What is Quality Laboratory Transfusion of whole blood or plasma raises the plasma protein concentration. Serum LD activity, primarily LD-1 and LD-2 isoenzymes, and bilirubin are increased. Transfusions may reduce levels of sodium chloride and water retention but may increase potassium concentration. It is the difference between two successive results, regardless of interval between, and it is used to identify a clinically significant change in values. The reference change value is the value that must be exceeded before a change in consecutive test results is statistically significant. The reference change value is generally higher in hospitalized people than in healthy ones Total Quality Control Total Quality Leadership Continuous Quality Improvement Quality Management Science Industrial Quality Management. 1. Quality Laboratory Processes (QLPs) 2. Quality Control (QC) 3. Quality Assessment (QA) 4. Quality Systems (QSs) QLPs include analytical processes, general policies, practices, and 33 Chem PPT Flashcards, Unit 1 Processes (QLPs)? What is Implementing TQM? What is QC? What is QA? What is Turnaround Time (TAT)? What is QI? What is QP? What is Total Quality Management? What is QS What is Personnel Competency and Training? procedures that define how all aspects of the work are done. Completion of Total Quality Management, for example, QLP, QC, QA, QI, QP. Quality Control emphasizes statistical control procedures but also includes non-statistical check procedures such as linearity checks, reagent and standard checks, and temperature monitors. Quality Assessment concerned primarily with broader measures and monitors of laboratory performance such as turnaround time, specimen identification, patient identification, and test utility. The time between when a test is orders or a specimen is submitted for analysis and when the test results are reported. Quality Improvement provides a mechanism through which one can act on those measures. Quality Planning provides the planning step. Is considered a quality system that is implemented to ensure quality. It is a set of key quality elements that must be in place for other organization's work operations to function in a manner to meet the organization's stated quality objectives. Quality System include the following: Documents and records Organization Personnel Equipment Purchasing and Inventory Process control Information and Occurrence Management Assessment: external and internal Process Improvement 3. Customer service Importance of people, training, and education A key factor for successful training and assessment of laboratory staff is the planning and implementation of targeted education programs. Assessment of competence in job tasks as required by CLIA must be conducted semiannually the first year of employment and annually thereafter, and upon implementation of new test methodology before reporting of patient test results. Detailed directions on how to develop and implement a training and competency assessment program that meets regulatory requirements, and provides example of forms for documentation and record keeping should be made available. Design of an in-service training program. 34 Chem PPT Flashcards, Unit 1 How many phases are presence in a clinical testing process? What method is considered in analytical method? What should be monitored in a laboratory-wide basis? What are the documentation of analytical protocols? What are the procedures involved in monitoring of technical competency? What are the Statistical control of analytical methods? What does the unit identify? What does the number indicate? How is reagent-grade water prepared? What is ion exchange? What is the process of reverse osmosis? How effective is reverse Internet education programs provide an effective, costefficient way to implement in-service training. Web-based training programs in quality control concepts are available. Phases of total testing process: 1. Pre-analytical (Pre-Examination) 2. Analytical (Examination) 3. Post analytical (Post-Examination) Components of a reliable analytical method has to be considered Variables should be monitored on a laboratory-wide basis Documentation of analytical protocols a) Procedure document b) Laboratory manual Monitoring of technical competency a) Written list of objectives b) Incident reports, internal and external QC checks c) In-service and continuing education Employee conferences to detect nontechnical issues Statistical control of analytical methods a) Comparison of observed and known values b) Use of control limits to detect problems c) Need for control materials d) Selection of control products e) Use of control charts f) Calculation of control limits g) Interpretation of control data h) Reducing the risk of false alarms i) Levey-Jennings chart j) Westgard multirule procedure k) Identifying sources of analytical errors Combined use of liquid controls and moving averages of patient values for quality control monitoring The unit identifies the dimension - mass, volume, or concentration - of a measured property The number indicates how many units are contained in the property It’s prepared by distillation through the process of vaporizing and condensing liquid to purify or concentrate a substance. The process that removes ions to produce mineral free deionized water. Water is forced through a semipermeable membrane that acts as a molecular filter. It removes 95-99% of organic compounds and bacteria; 9035 Chem PPT Flashcards, Unit 1 osmosis? Why do we us ultraviolet oxidation? Whose specifications must reagent grade or analytical reagent grade chemicals meet? What are ultrapure reagents? What are reference materials? What are primary reference materials? What are secondary reference materials? Where are standard reference materials (SRMs) available? Where are certified reference materials (CRMs) available? What glassware should be used for accurate work? What are pipettes used for? What are two kinds of pipettes? What does a transfer pipette consist of? What are some characteristics of a transfer pipette? What are 2 types of transfer pipettes? What is a volumetric transfer pipette used for? What is an Ostwald-Folin pipette used for? What are some characteristics of the Ostwald-Folin pipette? What do measuring or 97% of all ionized and dissolved minerals. Using ultraviolet radiation eliminates many bacteria and cleaves many ionizing organics. American Chemical Society (ACS). Reagents that exceed purity specifications ex. “spectrograde”, “nanograde”, “HPLC pure”. Any material or substance, one or more physical or chemical properties of which are sufficiently well established for it to be used for calibration of instruments, validation of methods, assignment of values to materials, and evaluation of the comparability of results. Highly purified chemicals that are directly weighed or measured to produce a solution whose concentration is exactly known, 99.98% purity. Solutions whose concentrations cannot be prepared by weighing the solute and dissolving a known amount into a volume of solution. NIST for clinical and molecular laboratories. Examples are pure crystalline standards, human-based standards, animal blood standards, standards containing drugs of abuse in urine and human hair, and SRMs used for DNA profiling/crime scene investigations. At the Institute for Reference Materials and Measurements (IRRM) for clinical and molecular laboratories. Only class A glassware They are used for the transfer of a volume of liquid from one container to another. 1) To contain (TC) a specific volume of liquid 2) To deliver (TD) a specific volume Consist of a cylindrical bulb joined at both ends to a narrower glass tubing. A calibration mark is etched around the upper suction tube, and the lower delivery tube is drawn out to a gradual taper. 1) Volumetric transfer pipette 2) Ostwald-Folin pipette Calibrated to deliver (TD) accurately a fixed volume of a dilute aqueous solution. Used for accurate measurement of viscous fluids, such as blood or serum. 1) The bulb is closer to the delivery tip 2) Has an etched ring near the mouthpiece indicating that it is a blow-out pipette. A piece of glass tubing that is drawn out to a tip, and is 36 Chem PPT Flashcards, Unit 1 graduated pipettes look like? What are measuring or graduated pipettes used for? What are 2 measuring or graduated pipettes? How does a Serological pipette look like? How does a Mohr pipette look like? What are some pipetting techniques? graduated uniformly along its length. Principally used for the measurement of reagents and generally are not considered sufficiently accurate for measuring samples and calibrators. 1) Serological Pipette 2) Mohr Pipette 1) Has graduation marks down to the tip, visible or not visible 2) Must be blown out to deliver the entire volume of the pipette 3) Has an etched ring near the bulb end of the pipette signifying that it is a blowout pipette It is calibrated between two marks. 1) Pipetting bulbs should always be used 2) Pipettes must be held in the vertical position when the liquid level is adjusted to the calibration line and during delivery 3) When sighted at eye level, use lower meniscus for readings 4) Flow of liquid should be unrestricted, and the tapes should be touching the inclined surface of the receiving container. 5) The pipette is allowed to drain, and then the remaining liquid is blown out with a pipetting bulb What is a micropipettes ? A hallow glass tube used for measuring small volumes of liquid in microliters and transfer of liquid from one source to anothere Pipettes come in different Yes from single piece glass pipettes to more complex sizes? adjustable or electronic pipettes for various purposes with differing levels of accuracy and precision What is the purpose of a pipette To draw up liquid for the purpose of measuring and ? transferring a specific volume of liquid What is the mouthpiece of the The end of the pipette to which suction is applied to draw up pipette? liquid into the pipette What is the calibration lines of Marks on the stem of the pipette to show the point where a pipette? liquid must be drawn to give a specific volume What is Volume of the pipette ? Stated in millimeters example inscription may read 10ml in 1/10 ml and the pipette is graduated in 1/10 ml increments allowing it to be used to measure volumes up to 10 ml What is the T.D of the pipette? “To deliver “pipettes designed to deliver a specific volume of fluid What is the T. C of the pipette “To contain “ pipettes designed to contain a certain volume of fluid Why must a distinction Because there may be a difference between the volume a between T.D and T.C pipettes pipette will contain and a volume it will deliver be made ? What is T.D calibrated with ? Distilled or deionized water What is T.C glassware Mercury 37 Chem PPT Flashcards, Unit 1 calibrated with ? What is the meniscus ? What is centrifugation ? What is gravimetric ? What is a Double-pan, singlepan and electronic balances Define Thermometry. What are the two models of thermometers? Define Dilution. Define Evaporation. Define Lyophilization. Define Filtration. Which agencies and organizations address issues on safety? What are the key elements to ensure safety in the clinical laboratory? A crescent shaped structure appearing at the surface of a liquid column it has the appearance of a contact lens The process of using centrifugal force to separate the lighter portion of a solution mixture or suspension from heavier portions. The process used to measure the mass of a substance Types of balances Refers to the measurement of temperature to verify that devices measure within their prescribed temperature limits. liquid-in-glass thermometer and thermistor probe decreasing the concentration or activity of a given solution by adding solvent conversion of a liquid or volatile solid to vapor better known as freeze drying is used in laboratory medicine for the preparation of calibrators, control materials, reagents, and individual specimens for analysis. passage of a liquid through a filter by means of gravity, pressure, or a vacuum -Occupational Safety and Health Administration (OSHA) -Centers for Disease Control and Prevention (CDC) -The Joint Commission (TJC) -College of American Pathologists (CAP) -A formal safety program -Documented policies and effective use of mandated plans and/or programs -Identification of significant occupational hazards such as biological, chemical, fire and electrical hazards The person who is given the responsibility to implement and maintain a safety program. Who is the “Safety Officer” or “Chair of the Safety Committee? Who will provide technical -chemical hygiene officer guidance in the development of the chemical hygiene plan (CHP)? What are the safety standard for proper labeling of chemicals, types and locations of fire laboratory environments? extinguishers, hoods that are in good working order, proper grounding of electrical equipment, ergonomic issues and means for the proper handling and disposal of biohazardous materials. What does PPE stand for? Personal protective equipment. What are the primary Clothing such as laboratory coats, gowns or scrubs, gloves and requirements for PPE? eye protection (face shields) 38 Chem PPT Flashcards, Unit 1 What are the safety equipments used in camical laboratory? What does OSHA stand for? What does CMC stand for? Which agencies used for safety inspection? What does MSDS stand for? How to used MSDS in chemical hygine plan? How to used Exposure control plan? How to used Tuberculosis control plan? How to work Ergonomics program? What type of hazards encountered in the laboratory? What is the principle of the Universal Precautions? The purpose of barrier protection and other Personal Protection Equipment is to? Proper storage and use of chemicals is necessary to prevent dangers such as: What is the proper way of diluting acids? How should hazardous chemicals be dispensed? To avoid chemical hazards, how should organic solvents be handled? List all the ways electrical hazards can be prevented in the -Personal protective equipment (PPE) -Eye washers or face washers -Heat-resistant (non-asbestos) gloves -Eye safety devices such as safety goggles, glasses and visors -Desiccator guards -Chemical fume hood Occupational Safety and Health Administration Center for Medicare and Medicaid Services -Occupational Safety and Health Administration (OSHA) -Commission on Inspection and Accreditation of the CAP -The Joint Commission (TJC) -Center for Medicare and Medicaid Services (CMS) Material Safety Data Sheet The need for Material Safety Data Sheet (MSDS) which defines each chemical is toxic, carcinogenic or dangerous Ensures the protection of laboratory workers against potential exposure to blood-borne pathogens and ensures that the medical wastes produced by the laboratory are managed and handled in a safe and effective manner. Prevent the transmission of tuberculosis by early identification and isolation of patients at risk, environmental controls, appropriate use of respiratory protection equipment, education of laboratory employees and early initiation of therapy. Designed to prevent work-related musculoskeletal disorders through prevention and engineering controls -Biological -Chemical -Electrical -Fire hazards To treat all human blood and other potentially infectious materials as infectious prevent the skin and mucous membrane contamination from specimens Burns, explosions, fires and toxic fumes By slowly adding them to water while mixing With a commercially available automatic dispensing device Under a fume hood Prohibit use of all extension cords Worn wires on all electrical equipment should be 39 Chem PPT Flashcards, Unit 1 lab: Class A fire is caused by? Class B fire is caused by? Class C fire is caused by? Class D fire is caused by? Class E fire is classified as? Define Photometry Define Spectrophotometry What is Photometric measurement ? What is wavelength? What does Beer’s Law state? What is a tungsten light bulb? What is the function of a mercury vapor lamp Name the 10 parts that are in a Single-beam spectrophotometer. Name the 2 types of Light source. Name the 3 types of Filters. Spectrophotometers are classified as a What are the 2 choices of replaced immediately All equipment should be grounded with the use of three-prong plugs Ordinary Combustibles Flammable liquids and gases Electrical equipment Powdered metal (combustible) material A fire that cannot be extinguished -measurement of luminous intensity of light or amount of luminous light falling on a surface from such a source -Uses filter to isolate a narrow wavelength range of the spectrum for measurements -measurement of intensity of light at selected wavelengths -Use prisms or gratings to isolate a narrow wavelength range of the spectrum for measurements The process use to measure light intensity independent of wavelength A characteristic of electromagnetic radiation; the distance between two wave crests that is measured in nanometers (nm) The concentration of a substance is directly proportional to the amount of light absorbed or is inversely proportional to the logarithm of the transmitted light. A light source in the visible range of spectra. An example is a quartz halogen lamp. Supplies the needed energy in the UV region. It is used for calibration purposes but is not practical for absorbance measurements because it is used only at certain wavelengths Manual operation procedure Types of light sources Filters Monochromators Fiber optics Cuvets Photodetectors Readout devices Digital hardware and software Recorders • Incandescent and laser • • Glass, Prisms, Gratings Single- or Double-beam • Bandwidth and Turbidity 40 Chem PPT Flashcards, Unit 1 monochromators. What does a cuvet do? What does a photodetector do? Name the 4 Performance parameters of an instrument. What does NIST stand for? What does SRMS stand for? What does IRMM stand for? What is reflectance photometry? What transformation/equation is used for converting data into a linear format in reflectance photometry What is used in dry film chemistry systems? What is Atomic Absorption spectrophotometry? What are the 2 limitations of atomic absorption spectrophotometry? What is another name for flameless method in atomic absorption spectrophotometry? Name the 7 components of an Atomic Absorption spectrophotometry. • • • • • • • • Absorbs a portion of radiant energy. Converts light into an electrical signal that is proportional to the number of photons. Comparison of unknown with calibrator(s) Comparison with published/previously determined values NIST-provided SRMS for comparison IRMM-provided reference materials National Institute if Standards and Technology Standard Reference Materials Institute for Reference Material and Measurements A spectrophotometric technique in which diffused light illuminates a reaction mixture in a carrier Kubelka-Munk equation or Clapper-Williams transformation • Reflectance photometry • • An optical technique in which an element in the sample is excited and the radiant energy produced is measured. Spectral interferences Non-spectral interferences • Zeeman correction What is Fluorometry? Hollow cathode Chopper Flame Entrance Slit Monochromator Exit Slit • Detector Measurement of emitted fluorescent light When does Fluorescence occur? Fluorescence occurs when a molecule absorbs light at one wavelength and re-emits light at a longer wavelength. What is an atom or molecule that fluoresces called? What is the best way to describe Flow Cytometry? Flow Cytometry is: a. Able to measure A fluorophore The process in which measurement of physical and/or chemical characteristics of cells or particles are made, while cells or particles pass, preferably in single file, through the measuring apparatus in a fluid stream. D 41 Chem PPT Flashcards, Unit 1 multiple parameters including cell size, granularity, DNA and RNA content, DNA nucleotide ratios, chromatin structure, antigens, total protein content, cell receptor, membrane potential and calcium ion concentration. b. It combines laserinduced fluorometry and particle light scattering analysis c. Is the process in which measurement of physical and/or chemical characteristics of cells or particles are made, while cells or particles pass, preferably in single file, through the measuring apparatus in a fluid stream. All of the above. What is a single-channel front surface photofluorometer dedicated to the analyses of zinc protoporphyrin in whole blood called? Hematofluorometer How does Phosphorescence differ from fluorescence ? What is Phosphorimetry ? Phosphorescence continues even after radiation causing it has ceased. Luminometry is all of these except: a. Chemiluminescence, bioluminescence, electrochemiluminescen ce Are types of B Measurement of phosphorescence, a type of luminescence produce by certain substances after radiant energy or other types of energy are absorbed, with a longer decay time of emission. 42 Chem PPT Flashcards, Unit 1 luminescence in which the excitation event is caused by a chemical, biochemical or electrochemical reaction, and not by photo illumination. b. It has longer decay time of emission c. Instruments for measuring this type of light emission are generally known as luminometers. Nephelometry and Turbidimetry are: Factors influencing light scatter include: a. Effect of particle size b. wavelength dependence c. concentration of the particles d. distance of observation e. All of the above. What are the 5 types of electrochemistry used in the clinical laboratory? Which electrochemical technique measures the difference in electrical potential between two electrodes (halfcells) in an electrochemical cell? What are the three types of potentiometric electrodes? Analytical techniques of measuring scattered light E Potentiometry Voltammetry Amperometry Conductometry Coulometry Potentiometry Redox electrodes Ion-selective membrane electrodes (glass and polymer) PCO2 glass-sensing electrodes Potentiometry is usually applied for? What is Voltammetry? What process in voltammetry pH monitoring Electrolyte determination (ISE) Electrodes for PCO2 An electrolytic electrochemical process in which a specific oxidation or reduction reaction occurs at the surface of the working electrode. The charge transfer (current flow) at the surface of the working electrode. 43 Chem PPT Flashcards, Unit 1 provides the analytical information required? Name 2 applications in which voltammetry is used? What method of voltammetry is used to quantify dopamine in brain tissue of freely moving animals? What method of voltammetry is used for detecting trace concentrations of toxic metal ions? Which electrochemical process monitors current at the fixed (controlled) voltage between working and reference electrodes in an electrochemical cell? Amperometry is applied for? Conductometry is used in order to determine what? Name 2 purposes for which conductometry is used? An electrochemical technique that measures the electrical charge passing between two electrodes in an electrochemical cell, with the amount of charge passing between the electrodes being directly proportional to oxidation or reduction of an electroactive substance at one of the electrodes is called____________. Coulometry is applied in _________ An optical sensor used in analytical instruments to measure pH, blood gases and electrolytes What specific type of chemical sensor that consist of a biological recognition element and physicochemical transducer, and often an electrochemical or optical Anodic stripping voltammetry Rapid scan cyclic voltammetry Rapid scan cyclic voltammetry Anodic stripping voltammetry Amperometry Clark amperometric PO2 The quantity of an analyte present in a mixture; by measuring its effect on the electrical conductivity of the mixture. Conductivity-based hematocrit measurements Coulter principle - electronic counting of blood cells Coulometry Coulometric titration of chloride Optodes Biosensors 44 Chem PPT Flashcards, Unit 1 device? What special class of biosensors in which the immobilized biological recognition element is a binding protein? The migration of charge solutes or particles within a liquid medium under the influence of an electric field. What is Isoelectric point (pl) An ampholyte is _____________ What molecule behaves as an ampholyte in a solution and are considered amphoteric? It also contains many ionizable amino and carboxyl groups. A measuring technique that uses an optical system to scan and quantify electrophoretic fractions separated on the gel or other medium. In electrophoresis, after the support is removed from the electrophoresis cell, dried and fixed to prevent diffusion of sample components, it is then ________ in order to visualize the individual protein zones. An electrophoresis technique that produces zones of proteins, which are heterogeneous and physically separated from one another. What are the factors affecting electrophoresis? Affinity sensors Electrophoresis The pH at which a molecule has no net charge and will not migrate during electrophoresis A molecule that is positively or negatively charge on the basis of the pH of the solution in which it resides; Protein Densitometry Stained Zone electrophoresis The net electrical charge of the molecule The size and shape of the molecule Electric field strength Properties of the supporting medium Temperature of operation According to the theory of electrophoresis, anions move through the solutions toward the______. Anode 45 Chem PPT Flashcards, Unit 1 Cathode According to the theory of electrophoresis, cations move through the solutions toward the __________. A Negative A cathode is a________ electrode. Choose one only. a. Negative b. Positive c. Polarized d. Neutral B Positive A anode contains delivers a continuous _______ charge to the solution. Select one option. a. Negative b. Positive c. Polar d. Bipolar A new MLT lab requires a new C. Isolectric Focusing Power Supply power supply for electrophoresis procedures. Select the correct one from the catalog below: a. Trans-ductor Pulse Generator b. Inductive Power Supply c. Isolectric Focusing Power Supply d. Car Battery Yes The buffer establishes the pH at which electrophoresis is performed. Does it impact the solute as well? (Yes or No) Evaluate the statement (True or False False) Trans-barbital and barbital buffers have identical pH. C,D,E Which gels are compatible with electrophoresis? Choose 3 out of 5. a. SBA gel b. Triptic Soy Agarose Gel c. Starch gel and cellulose acetate d. Agarose gel e. Polyacrylamide gel 46 Chem PPT Flashcards, Unit 1 If mobile phase is a liquid, the technique is called_____________ a. Spectrum Chromatography b. Reverse Phase-Flow Cytometry c. Liquid chromatography d. Acid Reduction Chromatography If mobile phase is a gas, the technique is called_____________ a. Spectrum Chromatography b. Reverse Phase-Flow Cytometry c. Acid Reduction Chromatography d. gas chromatography c. liquid chromatography d. gas chromatography In Column Chromotagraphy the b. Silicon, polymer stationary phase may consist of a particle of pure ______or _______, or it may be coated onto or chemically bonded to support particles. Select the correct media. a. Silicon dioxide, sapphire bonded glass b. Silicon, polymer c. Agarose Gel, Thayers McConkey Media d. SBA agar, plastic Planar Chromotography has a. sheet of paper two options for media. Identify b. solid surface the correct two. a. sheet of paper (paper chromatography) b. solid surface (thin-layer chromatography [TLC]) c. Silicon d. Polymer Chromatography is a physical a. Stationary, mobile phases process whereby the components (solutes/analytes) 47 Chem PPT Flashcards, Unit 1 of a sample mixture are separated as a result of their differential distribution between the ________ and _______ phases. a. Stationary, mobile phases b. Gas, Solid Phases c. Plasma, Superfluidic d. Liquid, Stationary What is Planar Chromatography? What is the reference value in planar chromatography? What is Gas chromotography? What is Liquid Chromatography? What are the different chromatophric separation • • Paper Chromatography The stationary phase consists of a layer of water or a polar solvent coated onto the fibers of the sheet of paper • Thin Layer Chromatography (TLC) The stationary phase is a thin layer of particles of a material such as silica gel that is spread uniformly on a glass plate or a plastic or aluminum sheet • Rf value • Expression of solute's migration in TLC or PC • the ratio of solute migration to solvent front migration Distance from application point to solute center Rf = -----------------------------------------Distance from application point to mobile phase front • Gas chromatography • A gas mobile phase, or carrier gas, is used to carry a mixture of volatility solutes through a column containing the stationary phase, which usually is a nonvolatile liquid coated or bonded to particles or the inner surface of a capillary • the mobile phase, or carrier gas, is typically an inert gas such as nitrogen, helium, or argon • separation of analytes is based on differential partitioning into the stationary phase • Liquid chromatography • Separation is based on the differential distribution of the solutes between a liquid mobile phase and a stationary phase • When particles of small diameter are used as the stationary phase support, the technique is referred to as High Performance Liquid Chromatography (HPLC) or High Pressure Liquid Chromatography (HPLC) • Ion exchange chromatography • Partition chromatography 48 Chem PPT Flashcards, Unit 1 mechanisms? What is ion exchange chromatography? What is partition Chromatography? What is absorption chromatohraphy? What is size exclusion chromatography known as and what does it mean? • • • Adsorption chromatography Size exclusion chromatography Affinity chromatography • Ion exchange chromatography • Based on exchange of ions between charged stationary phase and ions of opposite charge in mobile phase • Cationic or anionic exchange resin Used for the separation of amino acids, glycated hemoglobin, hemoglobin variants and oligonucleotides • Partition chromatography • Basis of separation is the differential distribution of solutes between two immiscible liquids with one of the immiscible liquids serving as the stationary phase • separation is based on differences in the relative solubility of solute molecules between stationary and mobile faces • Classification of partition chromatography: 1. Gas liquid chromatography (GLC) 2. Liquid-liquid chromatography (LLC) • Adsorption chromatography • The basis of separation is differential adsorption of solutes on the surface of the stationary phase • Hydrogen bonding and hydrophobic interactions are the forces that mediate separations • Size exclusion chromatography • Also known as: • 1. Gel filtration chromatography • 2. Gel permeation chromatography • 3. Steric exclusion chromatography • 4. Molecular exclusion chromatography • 5. Molecular Sieve chromatography • Basis of separation are the differences in their molecular sizes 49