Bupivacaine
advertisement
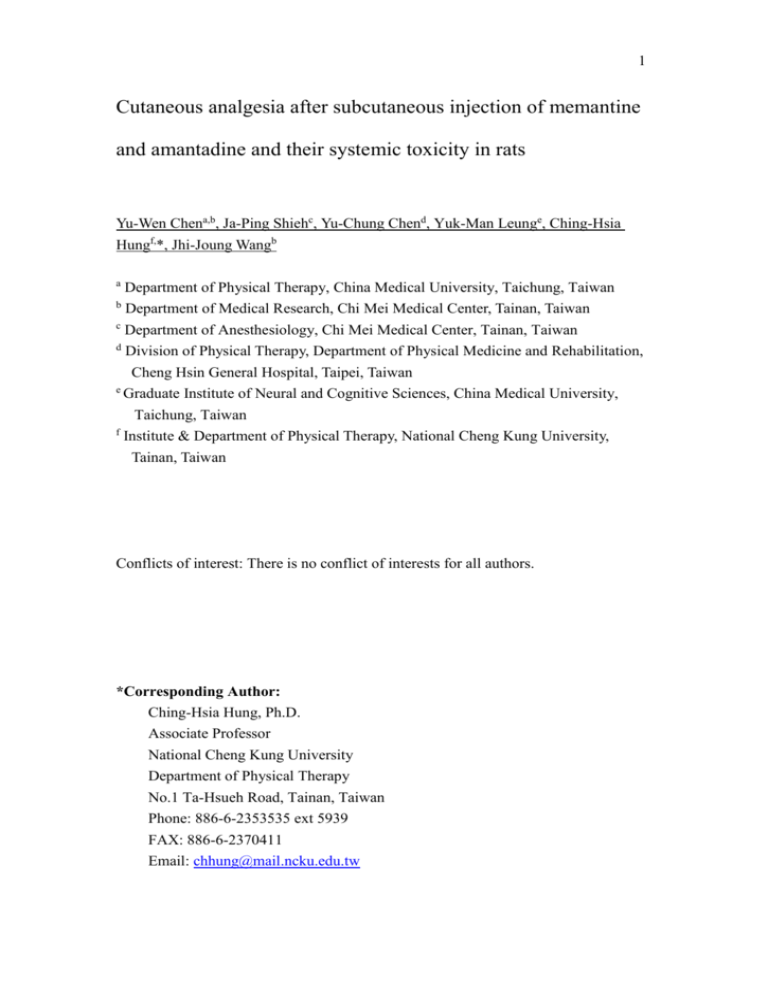
1 Cutaneous analgesia after subcutaneous injection of memantine and amantadine and their systemic toxicity in rats Yu-Wen Chena,b, Ja-Ping Shiehc, Yu-Chung Chend, Yuk-Man Leunge, Ching-Hsia Hungf,*, Jhi-Joung Wangb a Department of Physical Therapy, China Medical University, Taichung, Taiwan b Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan c Department of Anesthesiology, Chi Mei Medical Center, Tainan, Taiwan d Division of Physical Therapy, Department of Physical Medicine and Rehabilitation, Cheng Hsin General Hospital, Taipei, Taiwan e Graduate Institute of Neural and Cognitive Sciences, China Medical University, Taichung, Taiwan f Institute & Department of Physical Therapy, National Cheng Kung University, Tainan, Taiwan Conflicts of interest: There is no conflict of interests for all authors. *Corresponding Author: Ching-Hsia Hung, Ph.D. Associate Professor National Cheng Kung University Department of Physical Therapy No.1 Ta-Hsueh Road, Tainan, Taiwan Phone: 886-6-2353535 ext 5939 FAX: 886-6-2370411 Email: chhung@mail.ncku.edu.tw 2 ABSTRACT The purpose of the study is to find subcutaneous equianalgesic doses of memantine, amantadine and bupivacaine and use these doses to quantify the cardiovascular and central nervous system toxicity of these agents after intravenous administration. Memantine, amantadine and bupivacaine, a local anesthetic, in a dose-related fashion were determined for cutaneous analgesia by a block of the cutaneous trunci muscle reflex in rats, and equipotent doses were calculated. Following rapid intravenous infusion of equianalgesic bupivacaine, memantine, amantadine and saline (vehicle) in rats, we observed the onset time of seizure, apnea and impending death, and monitored mean arterial blood pressure and heart rate. Memantine and amantadine elicited dose-dependent cutaneous analgesia. At the 50% effective dose (ED50), the rank of potencies was bupivacaine [1.8 (1.7 – 2.0)] > memantine [19.1 (17.6 – 21.8)] > amantadine [36.1 (32.0 – 40.3)] (P < 0.05). On ED25, ED50 and ED75 basis, the duration caused by bupivacaine was similar to that caused by memantine or amantadine. At equianalgesic doses, the infusion time of memantine or amantadine required to induce seizure, impending death, and apnea was longer than that of bupivacaine during rapid intravenous infusion (P < 0.01). The decreasing slope in mean arterial blood pressure and heart rate was slower with memantine and amantadine when compared with bupivacaine at equivalent doses (P < 0.01). Our data 3 showed that memantine and amantadine (i) were equal to bupivacaine at producing durations of cutaneous analgesia but (ii) were less likely than bupivacaine to cause cardiovascular and central nervous system toxicity. Key Words: memantine; amantadine; bupivacaine; cutaneous analgesia; cardiovascular toxicity; central nervous system toxicity 4 1. Introduction Memantine, which is the derivative of amantadine (1-adamantanamine), is the first in a novel class of Alzheimer's disease agents whose therapeutic utility is linked to their ability to inhibit N-methyl-D-aspartate glutamate receptors (Otton et al., 2011; Yeh et al., 2010). Amantadine is a drug that has approval for use both as an antiviral and an antiparkinsonian drug by US Food & Drug Administration. Due to memantine reversibly inhibited tetrodotoxin-resistant sodium currents (Brau et al., 2001), memantine have a local anesthetic effect as infiltrative cutaneous analgesia in rats (Chen et al., 2011c). However, cutaneous (local) analgesia following subcutaneous injection of amantadine was not reported. The German chemist, Albert Niemann, was successful in isolating an alkaloid from the coca leaf and named it ‘cocaine’ in 1860 (Dillane and Finucane, 2010). Despite those somewhat physical or chemical differences, they both cause cardiovascular and central nervous system toxicity (Dillane and Finucane, 2010). For instance, bupivacaine induces significant cardiovascular toxicity (Albright, 1979; Khan et al., 2002). After clinical applications of the local anesthetics for more than 150 years, it is the right time to search a brand new local anesthetic whose chemical structure totally differed from traditional local anesthetics. Before considering the clinical use of memantine and amantadine as local 5 anesthetics, the systemic toxicity of these drugs should be examined. In this study, memantine and amantadine were investigated in rats with two main objectives: (i) to compare cutaneous analgesia of memantine and amantadine with that of bupivacaine to obtain the equianalgesic doses and (ii) to investigate their cardiovascular and central nervous system toxicity by rapid infusing equipotent doses of memantine, amantadine and bupivacaine. Bupivacaine, a known and long-lasting local anesthetic, was used as control. 6 2. Materials and methods 2.1.Animals Male Sprague-Dawley rats, 7–9 wk of age, weighting 285-335g, were purchased from the National Laboratory Animal Centre (Taipei, Taiwan), and then housed in a climate controlled room maintained at 21 ℃ with approximately 50% relative humidity in the Animal Center of China Medical University (Taichung, Taiwan). The lights were on a 12-h light/dark cycle (light on at 6:00 AM), with food and water available ad libitum up to time of experiments. The Institutional Animal Care and Use Committee of China Medical University (Taichung, Taiwan) approved this protocol for animal experimentation. 2.2.Drugs Memantine HCl, amantadine HCl, bupivacaine HCl and midazolam HCl were obtained from Sigma-Aldrich Chemical Co. (St. Louis, MO, USA). All drugs were dissolved in 0.9% NaCl (saline) before the subcutaneous and intraperitoneal injections or intravenous infusions. 2.3.Experimental designs The experimental protocol was divided into two parts. In Part 1, cutaneous analgesia of memantine (50.6, 35.0, 26.7, 20.0, 13.3, 6.7, 3.5 μmol/kg), amantadine (120.0, 100.0, 80.0, 40.0, 27.0, 20.0, 13.0 μmol/kg), bupivacaine (9.0, 5.3, 4.0, 2.0, 7 1.3, 1.0, 0.7 μmol/kg) and saline was performed (n = 8 rats for each dose of each drug) to obtain the equivalent potency 95% effective dose (ED95) of drugs; meanwhile, the full recovery time (duration) of bupivacaine, memantine and amantadine was evaluated at equianalgesic doses (ED25, ED50 and ED75) (n = 8 for each dose of each drug). After these above experiments, one control group was added to exclude the possibility of systemic analgesia of drugs. Animals (n = 8 rats for each dose of each drug) received intraperitoneal injections of testing drugs (bupivacaine, memantine and amantadine) at a dose of 2× ED95. In Part 2, time to cause systemic toxicity (seizure, apnea, and cardiac arrest), mean arterial blood pressure and heart rate were monitored after the equipotent dose (ED95) of drugs (bupivacaine, memantine or amantadine) was infused into the rats (n = 8 rats for each dose of each drug). Saline group (n = 8 rats) was used as control. 2.4.Part 1 - Skin Infiltrative analgesia 2.4.1. Subcutaneous Injections An experienced investigator, who was blinded to the identity of the injected drugs, was responsible for handling of animals and assessing the cutaneous analgesic effect. Infiltrative analgesia of the skin was evaluated via the cutaneous trunci muscle reflex (CTMR), characterized by the reflex movement of the skin over the back produced by twitches of the lateral thoracospinal muscle in response to local dorsal 8 cutaneous stimulation after subcutaneous injections of drugs (Chen et al., 2008; Hung et al., 2010). In brief, the hair on the rat's dorsal surface of the thoracolumbar region (10 cm × 6 cm) was mechanically shaved on the day before drug injection, and then each drug solved in 0.6 ml saline was injected subcutaneously using a 30-gauge needle into a naïve area of the shaved back of the un-anesthetized rats. Subcutaneous injection produced a circular skin wheal, approximately 2 cm in diameter. Then the wheal was marked with ink within 1 minute after subcutaneous injection. The cut end of an 18-gauge needle was affixed to a von Frey filament (no. 15; Somedic Sales AB, Stockholm, Sweden) to elicit a standardized noxious mechanical stimulus (191 g) without making tissue damage (acute sharp pain) (Chen et al., 2011a; Chen et al., 2007). In order to decrease the numbers of experimental animals used, the back of the rat was further divided into right and left parts, either of which, after a washout period of 1 week, received one drug injection. 2.4.2. Neurobehavioral Evaluation After observing the animal’s normal reaction to stimuli applied outside the wheal and on the contralateral side, we applied 6 stimuli at 6 different points within each wheal, with a frequency of 0.5-1 Hz, and scored the number to which the rat failed to react. Each drug’s cutaneous analgesia was quantitatively evaluated as the number of times the stimuli failed to elicit a response and was described as the percent of 9 possible effect (% PE). For instance, the absence of any response after 6 stimuli was defined as complete nociceptive/sensory block (100% PE), which was calculated as follows: % PE =100% ((number of stimuli that provoked no response)/6) During the duration of drug action, the maximum value of % PE was presented as percent of maximal possible effect (% MPE). Stimulus testing was applied 5 min before injection of drugs to confirm normal responses of rats, then every 5 min after injection for the first 30 min and every 10-15 min thereafter, until the CTMR fully recovered from the block (no more than 150 min). Each duration (full recovery time) of drug action was defined as the time from drug injection (i.e., time=0) to full recovery of CTMR (no analgesic effect or 0% MPE) (Chen et al., 2011c; Hung et al., 2012). 2.4.5. The effective doses (EDs) Rats were subcutaneously injected with 7 different doses of each drug (n = 8 rats for each dose of each drug), and dose-response curves were constructed from the % MPE of each dose of each drug. The curves were then fitted via SAS nonlinear (NLIN) procedures (version 9.1, SAS Institute, Cary, NC), and this value of ED50, defined as the dose that caused 50% cutaneous analgesia, was obtained (Chen et al., 2008; Leung et al., 2010). The ED25, ED75 and ED95 of drugs were obtained via using the same 10 curve-fitting (SAS NLIN procedures) that was used to derive the ED50 (Chen et al., 2011b; Hung et al., 2011). 2.5. Part 2 - Neurological and cardiovascular effects The rats were anesthetized with pentobarbital sodium at the dose of 50 mg/kg intraperitoneally and the right femoral artery and vein were cannulated with polyethylene catheters (PE-50), which were filled with heparin saline (35 U/mL). The free end of the catheter was threaded through an 18-gauge needle and then tunneled subcutaneously. The catheter was cut with 5 cm protruding from the skin at the midline in the posterior cervical area and sealed via heating it with a match and compressing it with a hemostat (Chen et al., 2011d; Hung et al., 2010). On Day 2, the rats were sedated with midazolam 0.375 mg/kg (1 mg/ml, midazolam HCl) intraperitoneally. Then, animals were placed in a small cage with an open top to allow the lines to reach the animal and prevent the animal from chewing on the lines. After 10 min, the tube in the right femoral vein was connected to an infusion pump (Harvard Model 22 Infusion Pump, Harvard Apparatus Inc., Holliston, MA) for delivery of the drugs. The tube in femoral artery was connected to a transducer, and mean arterial blood pressure and heart rate were recorded using a polygraph (MP36, BIOPAC Systems Inc, Goleta, CA, USA) (Hung et al., 2012; Srinivasa et al., 2003). The investigator (YWC) was blinded to the drugs under the 11 experiment. After rapid intravenous infusions of either 1) bupivacaine at 8 μmol/kg/min, memantine at 34 μmol/kg/min, or amantadine at 112 μmol/kg/min or 2) normal saline at a rate of 400 μL/kg/min, the onset time of seizure, respiratory arrest (apnea), time to cause impending death, mean arterial blood pressure and heart rate were recorded. The onset time of seizures was defined as the time when the first convulsion occurred and respiratory arrest when apnea occurred for 15 seconds by observation of chest movement. The time to impending death was defined as the time it took for the heart rate decreased to 0 per minute (Chen et al., 2011d; Hung et al., 2010). 2.6. Statistical Analysis Data are presented as mean ± S.E.M. or ED25, ED50, and ED75 values with 95% confidence interval (95% CI). The differences in potencies (ED50; Table 1), baseline data, %MPE (Fig. 2), and the time to cause toxicity (Fig. 4) between medications were evaluated using 1-way analysis of variance (ANOVA) and then the pairwise Tukey's honestly significant difference (HSD) test. The differences in duration (Fig. 3) among drugs were evaluated by 2-way ANOVA followed by pairwise Tukey's HSD test. Analysis of variance with repeated measures followed by Duncan’s multiple-range test was used for post hoc multiple comparisons of means on mean arterial blood pressure and heart rate (Fig. 5). SPSS for Windows (version 17.0) was 12 used for all statistical analyses. Statistical significance was set at P < 0.05. 13 3. Results 3.1.Part 1 - Cutaneous analgesia The memantine and amantadine, as well as long-acting local anesthetic bupivacaine elicited dose-dependent cutaneous analgesia in rats (Fig. 1). The ED50s of these drugs are shown in Table 1. On the ED50 basis, the relative potency of these drugs was found to be bupivacaine > memantine > amantadine (P<0.05; Fig. 1 and Table 1). At maximum testing dose of 9 μmol/kg for bupivacaine, 51 μmol/kg for memantine and 120 μmol/kg for amantadine, all these drugs caused 100% nociceptive/sensory blockade with durations of actions of 120±10, 96±11 and 109±8 min, respectively (Fig. 2). At equianalgesic doses (ED25, ED50 and ED75), the block duration caused by memantine or amantadine was similar to that caused by bupivacaine as infiltrative cutaneous analgesic (Fig. 3). Also, neither the subcutaneous injections of saline (Fig. 2) nor the intraperitoneal injections of testing drugs (data not shown) produced cutaneous analgesia. All rats recovered completely after subcutaneous injections of drugs. 3.2.Part 2 – Systemic toxicity Before experiments, we confirmed those baseline data of body weight, mean arterial blood pressure and heart rate demonstrated no significant differences among these four groups (data not shown). At equianalgesic doses (ED95), the infusion time 14 of memantidine and amantidine required to induce seizure, impending death and apnea (respiratory arrest) was longer than that of bupivacaine (Fig. 4; P<0.01). The rats in all drug groups eventually succumbed to seizure, apnea and asystole (impending death). There were no systemic toxicities in any of the animals during the infusion period in the saline group. In all drug groups, the mean arterial blood pressure and heart rate showed a tendency to decrease before cardiovascular collapse (Fig. 5). The declines in mean arterial blood pressure and heart rate were slower in the amantadine (P<0.01) or memantine (P<0.01) group when compared with the bupivacaine group (Fig. 5). The rapidity of decline of the mean arterial blood pressure and heart rate occurred in the following order: bupivacaine > amantadine > memantine (Fig. 5). 15 4. Discussion We found subcutaneous dosages of memantine and amantadine which produced similar durations of skin analgesia as bupivacaine, while continuous intravenous administration of memantine and amantdine appeared to lead to the later onset of serious toxic cardiovascular and central nervous system effects. Local anesthetics block voltage-gated Na+ channels (Borgeat and Aguirre, 2010). Because memantine shows the blockade of tetrodotoxin-resistant sodium currents at 2-Hz stimulation in small dorsal root ganglion neurons (Brau et al., 2001), it has a local anesthetic effect (Chen et al., 2011c). Additionally, the inhibition of Na+ channels is a well precedented mechanism used in therapy epilepsy as well as other hyperexcitability disorders (Large et al., 2011). Furthermore, memantine and amantadine in the case of a systemic administration are capable of blocking the N-methyl-D-aspartate receptors and producing the anticonvulsant effects (Gmiro and Serdiuk, 2000). Although the pharmacological mechanisms of amantadine are largely unclear in this study, inhibiting the voltage-dependent Na+ channel may be one of the principle mechanisms of amantadine to display a local anesthetic effect, which is worth studied in the future. Infiltrative analgesia of skin is an acceptable option for management of surgical analgesia and postoperative pain, because it is relatively free of side effects (Khan et 16 al., 2002). Currently, bupivacaine and lidocaine are commonly used in this field (McLure and Rubin, 2005). It has been known that subcutaneous memantine displayed more potent than lidocaine (Chen et al., 2010), but less potent than bupivacaine as cutaneous analgesia. Besides, we showed for the first time that amantadine produced dose-dependent cutaneous analgesia in rats. Furthermore, on an equianalgesic basis (ED25, ED50 and ED75), the sensory block duration of memantine or amantadine was similar to that long-acting local anesthetic bupivacaine. These findings suggest that there may be a potential for the use of memantine and amantadine as long-action local anesthetics in the clinical setting, provided that the cardiovascular and central nervous system toxicity is investigated. The local anesthetics through accidental intravenous injection may induce cardiovascular and central nervous system toxicity and even result in death (Dony et al., 2000; Srinivasa et al., 2003). Using a local anesthetic animal model, we examined the local anesthetic effects of memantine, amantadine and bupivacaine as infiltrative cutaneous analgesic to estimate the equianalgesic doses of these drugs. Alternatively, we selected the animal model with the spontaneously breathing rats for a clinical scenario when local analgesia is performed on humans. Nevertheless, this model has its own limitations. First, the concomitant administration of midazolam may have influenced the threshold doses of toxic manifestations (e.g., seizure activity). Second, 17 in contrast with bolus injection, the slow infusion rate allows the administration of the large dose of local anesthetics before the toxic symptoms arise. On an equipotent basis, we demonstrated that infusion of memantine and amantadine displayed a delayed onset of cardiovascular and central nervous system toxicity when compared with bupivacaine. However, the grades of toxicities were the same once toxicity occurred (Fig. 4). Furthermore, we also noticed that the declines in mean arterial blood pressure and heart rate were longer in the memantine and amantadine groups when compared with bupivacaine group. Overall, our results suggest that memantine and amantadine are less “toxic” and may feature a safer systemic toxicity profile than bupivacaine following continuous intravenous administration. Ropivacaine has been shown to have less cardiac depression than bupivacaine, although recent investigations reported that ropivacaine is at least 40% less potent than bupivacaine (McDonald et al., 1999; Polley et al., 1999). Ohmura et al. clearly (Ohmura et al., 2001) demonstrated that, at equivalent doses, the cumulative doses of local anesthetic required to cause asystole was 2.7-folds larger in ropivacaine (108 ± 27 mg/ kg) group than in the bupivacaine group (40 ± 9 mg/kg). By contrast, we revealed that the infusion time of memantidine (20.3 ± 6.4 min) and amantidine (12.1 ± 2.9 min) required to induce impending death (asystole) was 5.8- and 3.5-folds greater than that of bupivacaine (3.5 ± 0.1 min) at equianalgesic doses, respectively. 18 In addition, there is also an antidote for local anesthetic toxicity, namely Intralipid, that improves their safety (Espinet and Emmerton, 2009; Weinberg et al., 2008). Toxicities arising from other effects of these agents (N-methyl-D-aspartate block, anticholinergic, noradrenergic, dopaminergic, serotonergic) may be more likely to occur but are difficult to assess in this model. We observed that the molecular structures of memantine and amantadine also contain hydrophilic and hydrophobic groups and do not resemble that of bupivacaine, which holds a benzene ring. Furthermore, the observations that memantine and amantadine have long-acting local anesthetic properties and possibly produce their toxic effects later than bupivacaine may be clinically relevant. We did not evaluate whether memantine and amantadine induce local toxicity in the injected tissues, however, it is noteworthy that in this study we detected no apparent side effects after subcutaneous injection. All rats recovered completely. Our data suggest that memantine and amantadine may have features that make them as a valuable alternative cutaneous analgesic or anesthetic, although further studies on sciatic or spinal nerve block and the possibility of nerve (tissue) damage from drug injection are important issues that need further investigation. The previous experiment reported memantine elicits local analgesia against cutaneous nociceptive stimuli, is more potent than lidocaine, and has a longer duration 19 of action (Chen et al., 2011c). This preclinical study reported that (i) amantadine and memantine produce skin infiltrative analgesia in dose-related manners and their block durations are similar to that of long-lasting local anesthetic bupivacaine. And (ii) intravenous equianalgesic doses of memantine and amantadine are better tolerated to induce central nervous system and cardiovascular system toxicity than bupivacaine. 20 Acknowledgements The authors gratefully acknowledge the financial support provided for this study by the National Science Council (NSC 100-2314-B-039-017-MY3) of Taiwan. 21 References Albright, G.A., 1979. Cardiac arrest following regional anesthesia with etidocaine or bupivacaine. Anesthesiology 51, 285-287. Borgeat, A., Aguirre, J., 2010. Update on local anesthetics. Curr Opin Anaesthesiol 23, 466-471. Brau, M.E., Dreimann, M., Olschewski, A., Vogel, W., Hempelmann, G., 2001. Effect of drugs used for neuropathic pain management on tetrodotoxin-resistant Na(+) currents in rat sensory neurons. Anesthesiology 94, 137-144. Chen, Y.W., Chu, C.C., Chen, Y.C., Hung, C.H., Hsueh, M.I., Wang, J.J., 2011a. Clonidine as adjuvant for oxybuprocaine, bupivacaine or dextrorphan has a significant peripheral action in intensifying and prolonging analgesia in response to local dorsal cutaneous noxious pinprick in rats. Neurosci Lett 496, 186-190. Chen, Y.W., Chu, C.C., Chen, Y.C., Hung, C.H., Wang, J.J., 2011b. Intrathecal propranolol displays long-acting spinal anesthesia with a more sensory-selective action over motor blockade in rats. Eur J Pharmacol 667, 208-214. Chen, Y.W., Chu, C.C., Chen, Y.C., Wang, J.J., Hung, C.H., 2010. Isobolographic analysis of caramiphen and lidocaine on spinal anesthesia in rats. Neurosci Lett 22 469, 174-178. Chen, Y.W., Chu, C.C., Chen, Y.C., Wang, J.J., Hung, C.H., 2011c. The local anesthetic effect of memantine on infiltrative cutaneous analgesia in the rat. Anesthesia and analgesia 113, 191-195. Chen, Y.W., Chu, K.S., Lin, C.N., Tzeng, J.I., Chu, C.C., Lin, M.T., Wang, J.J., 2007. Dextromethorphan or dextrorphan have a local anesthetic effect on infiltrative cutaneous analgesia in rats. Anesth Analg 104, 1251-1255, tables of contents. Chen, Y.W., Liu, K.S., Wang, J.J., Chou, W., Hung, C.H., 2008. Isobolographic analysis of epinephrine with bupivacaine, dextromethorphan, 3-methoxymorphinan, or dextrorphan on infiltrative anesthesia in rats: dose-response studies. Reg Anesth Pain Med 33, 115-121. Chen, Y.W., Wang, J.J., Liu, T.Y., Chen, Y.C., Hung, C.H., 2011d. Systemic dextromethorphan and dextrorphan are less toxic in rats than bupivacaine at equianesthetic doses. Can J Anaesth 58, 55-61. Dillane, D., Finucane, B.T., 2010. Local anesthetic systemic toxicity. Can J Anaesth 57, 368-380. Dony, P., Dewinde, V., Vanderick, B., Cuignet, O., Gautier, P., Legrand, E., Lavand'homme, P., De Kock, M., 2000. The comparative toxicity of ropivacaine and bupivacaine at equipotent doses in rats. Anesth Analg 91, 23 1489-1492. Espinet, A.J., Emmerton, M.T., 2009. The successful use of intralipid for treatment of local anesthetic-induced central nervous system toxicity: Some considerations for administration of intralipid in an emergency. Clin J Pain 25, 808-809. Gmiro, V.E., Serdiuk, S.E., 2000. [Comparative study of the NMDA-blocking activity and safety of mono- and bis-cationic compounds in animals]. Eksperimental'naia i klinicheskaia farmakologiia 63, 3-8. Hung, C.H., Chu, C.C., Chen, Y.C., Chen, Y.W., Hong, H.J., Wang, J.J., 2011. Isoflurane for spinal anesthesia in the rat. Neurosci Lett 501, 138-142. Hung, C.H., Chu, C.C., Chen, Y.C., Liu, K.S., Chen, Y.W., Wang, J.J., 2012. Cutaneous analgesia and systemic toxicity of carbetapentane and caramiphen in rats. Reg Anesth Pain Med 37, 34-39. Hung, C.H., Liu, K.S., Shao, D.Z., Cheng, K.I., Chen, Y.C., Chen, Y.W., 2010. The systemic toxicity of equipotent proxymetacaine, oxybuprocaine, and bupivacaine during continuous intravenous infusion in rats. Anesth Analg 110, 238-242. Khan, M.A., Gerner, P., Kuo Wang, G., 2002. Amitriptyline for prolonged cutaneous analgesia in the rat. Anesthesiology 96, 109-116. Large, C.H., Bison, S., Sartori, I., Read, K.D., Gozzi, A., Quarta, D., Antolini, M., 24 Hollands, E., Gill, C.H., Gunthorpe, M.J., Idris, N., Neill, J.C., Alvaro, G.S., 2011. The efficacy of sodium channel blockers to prevent phencyclidine-induced cognitive dysfunction in the rat: potential for novel treatments for schizophrenia. J Pharmacol Exp Ther 338, 100-113. Leung, Y.M., Wu, B.T., Chen, Y.C., Hung, C.H., Chen, Y.W., 2010. Diphenidol inhibited sodium currents and produced spinal anesthesia. Neuropharmacology 58, 1147-1152. McDonald, S.B., Liu, S.S., Kopacz, D.J., Stephenson, C.A., 1999. Hyperbaric spinal ropivacaine: a comparison to bupivacaine in volunteers. Anesthesiology 90, 971-977. McLure, H.A., Rubin, A.P., 2005. Review of local anaesthetic agents. Minerva Anestesiol 71, 59-74. Ohmura, S., Kawada, M., Ohta, T., Yamamoto, K., Kobayashi, T., 2001. Systemic toxicity and resuscitation in bupivacaine-, levobupivacaine-, or ropivacaine-infused rats. Anesth Analg 93, 743-748. Otton, H.J., Lawson McLean, A., Pannozzo, M.A., Davies, C.H., Wyllie, D.J., 2011. Quantification of the Mg(2+)-induced potency shift of amantadine and memantine voltage-dependent block in human recombinant GluN1/GluN2A NMDARs. Neuropharmacology 60, 388-396. 25 Polley, L.S., Columb, M.O., Naughton, N.N., Wagner, D.S., van de Ven, C.J., 1999. Relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labor: implications for therapeutic indexes. Anesthesiology 90, 944-950. Srinivasa, V., Gerner, P., Haderer, A., Abdi, S., Jarolim, P., Wang, G.K., 2003. The relative toxicity of amitriptyline, bupivacaine, and levobupivacaine administered as rapid infusions in rats. Anesth Analg 97, 91-95, table of contents. Weinberg, G.L., Di Gregorio, G., Ripper, R., Kelly, K., Massad, M., Edelman, L., Schwartz, D., Shah, N., Zheng, S., Feinstein, D.L., 2008. Resuscitation with lipid versus epinephrine in a rat model of bupivacaine overdose. Anesthesiology 108, 907-913. Yeh, H.H., Yang, Y.H., Chen, S.H., 2010. Simultaneous determination of memantine and amantadine in human plasma as fluorescein derivatives by micellar electrokinetic chromatography with laser-induced fluorescence detection and its clinical application. Electrophoresis 31, 1903-1911. 26 Table 1. The 50% effective dose (ED50), ED25 and ED75 of memantine, amantadine and bupivacaine for infiltrative cutaneous analgesia in rats. Drug ED25 ( 95% CI ) ED50 ( 95% CI ) ED75 ( 95% CI ) ED95 Bupivacaine 1.2 (1.1 – 1.4) ab 1.8 (1.7 – 2.0) ab 3.0 (2.9 – 3.2) ab 8 Memantine 9.1 (7.7 – 12.6) a 19.1 (17.6 – 21.8) a 29.5 (27.9 – 32.5) a 34 Amantadine 25.0 (23.1 – 27.9) 36.1 (32.0 – 40.3) 62.4 (59.5 – 67.7) 112 The ED50 of drugs (μmol/kg) were obtained from Fig. 1. CI = confidence interval. Symbols (a,b) indicated P < 0.05 when drugs was compared with amantadine and memantine, respectively, using a one-way ANOVA and pairwise Tukey’s HSD test for paired comparisons. %MPE (maximal possible effect) 27 100 80 60 40 20 Bupivacaine Memantine Amantadine 0 1 10 100 Dose ( mol/kg ) Fig. 1. 28 Bupivacaine (9 mol/kg) Amantadine (120 mol/kg) Memantine (51 mol/kg) Saline %PE (possible effect) 100 80 60 40 20 0 0 15 30 45 60 75 90 105 120 135 150 Time (min) Fig. 2. Full recovery time ( min ) 29 Bupivacaine (B) Memantine (M) Amantadine (A) 50 40 30 20 10 B=M=A 0 25 50 75 ED ( effective dose ) Fig. 3. Time to cause toxicity (min) 30 25 Seizure Apnea Impending death ** 20 ** 15 * * 10 5 0 ND ND ND line caine tadine antine a S a piv Aman Mem u B Fig. 4. Heart rate (bpm) Mean arterial blood pressure (mmHg) 31 160 120 Saline Memantine Amantadine Bupivacaine 80 40 0 0 5 10 15 20 * 25 30 35 40 * Time (min) 400 300 200 100 0 0 5 10 15 20 * 25 30 35 * 40 Time (min) Fig. 5. 32 Figure Legends Fig. 1. The dose—response curves of bupivacaine, memantine and amantadine as infiltrative cutaneous analgesia in rats (n = 8 at each testing point). Data are shown as mean±S.E.M. Fig. 2. Time courses of bupivacaine (9 μmol/kg), amantadine (120 μmol/kg), memantine (51 μmol/kg) and saline (vehicle) as infiltrative cutaneous analgesia in rats. Data are presented as mean±S.E.M.; each group, n=8. Fig. 3. Full recovery time (duration) of cutaneous analgesia of bupivacaine, memantine and amantadine at ED25, ED50 and ED75 (n = 8 at each testing point). Data are mean±S.E.M. The difference in duration was evaluated via using two-way ANOVA followed by pairwise Tukey's HSD test. Fig. 4. Time to cause toxicity with equipotent (ED95) bupivacaine (8 μmol/kg/min), memantine (34 μmol/kg/min) or amantadine (112 μmol/kg/min) at the onset of seizure, respiratory arrest (apnea) and time to cause impending death. Saline group was not detected (ND) the toxicity symptoms. The symbol (*) indicates P < 0.01 when memantine or amantadine compared with bupivacaine. Data are presented as meanS.E.M.; each group, n=8; 95% effective dose, ED95. Fig. 5. Mean arterial blood pressure and heart rate change during infusion of either 1) bupivacaine at 8 μmol/kg/min, memantine at 34 μmol/kg/min, or amantadine at 112 33 μmol/kg/min or 2) normal saline in the volume of 400 μL/kg/min (the same volume given to the animals in the drug group) as infusion; 0 min is the start of infusion. Infusion was stopped when the time to cause impending death was reached. The symbol (*) indicates P < 0.01 for memantine or amantadine compared with bupivacaine. Data are presented as meanS.E.M.; each testing group contained eight rats.