Cost-containment and Access to care
advertisement

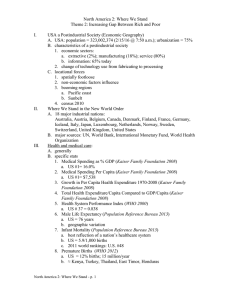
Cost-Containment, Medical Technology and Access to Care: A Comparative Analysis of Health Policy in the United States, the United Kingdom And Canada Emily Adrion Economics 2003 Health System Structure • Goals: Universal and equal access, cost-containment, efficiency. • Financing: determines the budget constraint and the resource distribution/ allocation within the system. • All industrialized nations, excluding the U.S., have national health services or compulsory insurance coverage. Purpose of Research • Exploding costs have been a major issue faced by U.S. health policy makers • Overuse of new medical technology is often cited as one of the primary factors responsible for cost growth. • Have the more stringent cost-containment strategies of nations with lower per-capita spending inhibited the introduction and diffusion of new medical technology? • Greater control of costs neither limits the introduction of medical technology nor results in lower health outcomes. Health Care in the United States • Private health insurance • Traditional Insurance • Managed Care: HMOs; PPOs • Medicare, Medicaid • 16% of the U.S. population remains uninsured (44 million Americans) Why the U.S. system suffers from inefficiency and rising costs • Market failures of health care: • Information failures - Gov’t regulation • Uncertainty- health insurance • Problems with health insurance: • Risk pooling => gaps in coverage • Moral Hazard=> exploding costs – The third party payment problem • Managed Care as a Solution: • LT effects on cost growth? • Slower diffusion of new technology? – RAND study (1981) The Third Party Payment Problem and Health Insurance Traditional health insurance and the consumption of health care in the United States Canada: National Health Insurance • Universal coverage • Single-payer plan financed through general taxation • Reimbursement: global budgets to hospitals; negotiated fee-for-service to physicians • Private production of health services • With virtually no role for the market to set prices, health care expenditure growth becomes almost entirely a political decision made independently in each province. United Kingdom: National Health Service • Model of socialized health care • Nearly universal coverage: small market for private health insurance • Single-payer plan financed through general taxation • Reimbursement: global budgets to hospitals; Salaries and per-patient payments to physicians • Public production of health services Prices and quantities in a controlled market The Supply and Demand for health care in the UK Theory: Technological Change and Health Care Cost Growth • Health insurance and the bias towards costincreasing technological change – The Goddeeris Model • Diffusion of new medical technology – Impact of regulation and cost control – Baker and Spetz (1997) Analysis: Overview of the Concepts and Statistics • Basic concepts: • health vs. health care • Outcome benefits vs. utility benefits • Statistical problems: • Data not available for every year for every country • For many variables no data could be found • Differences in definitions of variables Regression Analysis Quality of Health Care= f(total HC, R&D, age, income, lifestyle, tech access) • Regression Analysis 79 78.5 life expect • Quality of Care represented by: infant mortality, death rate, life expectancy and patient satisfaction • Heteroscedasticity; Multicollinearity 79.5 78 77.5 life expect 77 76.5 76 75.5 0 20 40 r&d per cap 60 80 The Raw Data Canada United Kingdom United States Total Health Spending (% GDP) 1999 Total per capita (US$ PPP): 1999 9.31 6.91 12.87 2428 1666 4373 30.857 11.03 61.5 1.7 3.4 7.7 8.1 6.3 13.4 1999 5.3 5.8 7.1 1999 79 77.4 76.7 Technology health R&D per capita (US$): 1999 MRIs per million pop: 1999 CT scanners per million pop: 1999 Health Outcomes Infant Mortality: Life expectancy: Analysis: Data from 10 Developed Nations life expectancy life expect 80 79 78 77 76 75 74 73 72 71 70 life expect 0 100 200 300 400 angioplasty per 100000 pop Plot of life expectancy and Angioplasty Procedures per 100,000 pop. Data from 10 Developed Nations, (continued) 80 life expectancy 79 78 77 76 75 74 life expect 73 72 71 70 0 1000 2000 3000 4000 5000 HC spending per capita Plot of life expectancy and health care spending per capita. Conclusions • Theory: high costs and worse outcomes of US system may be the result of insurance • Without adequate control over total spending or total quantity supplied the system may have inefficient levels of cost-increasing technologies • The raw data suggests the US may have inefficient levels of high tech equipment (CT scanners, MRIs) • Equally troublesome is that higher spending has not resulted in greater health outcomes • However, the effects of R&D are long term • Outcome vs. Utility Benefits Ways Forward • Premium regulation • Development of standardized treatment guidelines and protocols • Medical Technology Assessment • To ensure costeffectiveness, safety and efficacy of medical innovations