PowerPoint - LHD Benefit Advisors
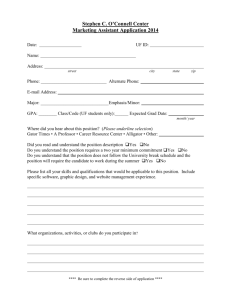
advertisement

This UBA Employer Webinar Series is brought to you by United Benefit Advisors in conjunction with Jackson Lewis For a copy of this presentation, please go to www.UBAbenefits.com. Go to the Wisdom tab and scroll down to HR Webinar Series and click. Under Employer Series click the Registration and Presentation link. Click the red Presentation button to see the slides. LazzarottiJ@jacksonlewis.com 2 Represents management exclusively in every aspect of employment, benefits, labor, and immigration law and related litigation. 750 attorneys in 55 locations nationwide. Current caseload of over 6,500 litigations and approximately 415 class actions. Founding member of L&E Global. 3 4 This presentation provides general information regarding its subject and explicitly may not be construed as providing any individualized advice concerning particular circumstances. Persons needing advice concerning particular circumstances must consult counsel concerning those circumstances. Indeed, health care reform law is highly complicated and it supplements and amends an existing expansive and interconnected body of statutory and case law and regulations (e.g., ERISA, IRC, PHS, COBRA, HIPAA, ADA, GINA, etc.). The solutions to any given business’s health care reform compliance and design issues depend on too many varied factors to list, including but not limited to, the size of the employer (which depends on complex business ownership and employee counting rules), whether the employer has a fully-insured or self-funded group health plan, whether its employees work full time or part time, the importance of group health coverage to the employer’s recruitment and retention goals, whether the employer has a collectively-bargained workforce, whether the employer has leased employees, the cost of the current group health coverage and extent to which employees must pay that cost, where the employer/employees are located, whether the employer is a religious organization, what the current plan covers and whether that coverage meets minimum requirements, and many other factors. 5 What are “voluntary benefits”? Why offer them? They are voluntary, so no issues, right? o Can these benefits really be subject to ERISA? o What about COBRA, HIPAA, FMLA, etc.? o Are there tax implications? o Do I have to think about the ACA? 6 Typically take the form of “individual” policies Designed to “beef-up” core benefit program(s) Generally provide focused coverage “Limited” employer involvement Employees usually pay 100% of the cost of the coverage 7 Examples of possible voluntary benefits o Medical Benefits • Dental, Vision • Critical Illness Insurance • Hospital Confinement, Fixed Indemnity o Individual Disability Insurance o Long-Term Care Insurance o Auto and Home Insurance o Pre-Paid Legal Coverage o Identity Theft Insurance 8 They can offer: o Greater choice with less cost o Reduced administrative burden o Enhance overall benefit structure But some with some practical considerations o Avoid overwhelming employees o Increased negotiating leverage o Implementation needs o Responding to questions/complaints by employees about carriers, benefits, claims, etc. 9 Not really… o These benefits could be “employee welfare benefit plans” under ERISA o Voluntary programs providing health benefits also could be “group health plans,” and subject to the Affordable Care Act o There also are potential COBRA, HIPAA, FMLA, tax and other issues to consider. Practical Tip – A employee welfare benefit plan providing medical benefits could be subject to ERISA, but not also subject key provisions of the ACA. 10 What is an “employee welfare benefit plan” under ERISA? o a plan, fund or program o established or maintained by an employer or by an employee organization, or by both o for the purpose of providing medical, surgical, hospital care, sickness, accident, disability, death, unemployment or vacation benefits, apprenticeship or other training programs, day care centers, scholarship funds, prepaid legal services or severance benefits • Note what is not listed – e.g., identity theft, homeowners insurance, automobile insurance, pet insurance – not ERISA benefits. o for participants or their beneficiaries 11 What is a “plan, fund or program”: o Based on analysis of the surrounding facts and circumstances o Must be an “ongoing” administrative programs o That enables reasonable persons to ascertain • intended benefits • class of beneficiaries • source of financing • procedures for receiving benefits 12 Types of welfare benefit plans o Health insurance – medical, dental, vision, HFSA, on-site clinic/health provider o Group life insurance o Long-term disability income o Business travel insurance o Pre-paid legal services o Short-term disability income only if provided through insurance or a trust fund, and in excess of state mandated disability benefits (CA, HI, NJ, NY, PR, RI) o Severance pay 13 Exclusions from ERISA welfare benefit plans o Payroll practices to the extent paid from general assets – short term disability o On-premises facilities (to the extent of treatment of minor injuries or illness or rendering first aid in case of accidents) o Holiday gifts o Sales to employees o Hiring halls o Remembrance funds o Strike funds o Certain group or group-type insurance programs 14 DOL Safe Harbor - certain insurance programs exempt from ERISA where all of the following are met: o no contributions are made by an employer or employee organization o participation in the program is completely voluntary for employees o the sole functions of the employer or employee organization with respect to the program are, without endorsing the program, to permit the insurer to publicize the program to employees or members, to collect premiums through payroll deductions or dues checkoffs, and to remit them to the insurer o the employer or employee organization receives no consideration in the form of cash or otherwise in connection with the program, other than reasonable compensation, excluding any profit, for administrative services actually rendered 15 DOL Safe Harbor: no contributions are made by an employer or employee organization o Employer paying premiums directly to carrier. o Employer reimburses employees for premiums paid by employee o Pre-tax contributions under Section 125 Plan? • Salary reductions treated as employer contributions. Prop. Treas. Reg. 1.125-1(r)(2). • Employee choice of cash or after-tax contributions toward health coverage is NOT employer payment plan. Notice 2013-54 16 DOL Safe Harbor: permissible employer functions, but no endorsement. o to permit the insurer to publicize the program to employees…, to collect premiums through payroll deductions or dues checkoffs, and to remit them to the insurer o Some related functions also may be permissible as within the normal course of the above enumerated functions: • Setting when policy becomes effective • Tracking which employees are eligible, and sharing with carrier • Coordinate changes in coverage with carrier o Endorsement is very fact specific 17 DOL Safe Harbor: Endorsement risks o Carrier selection o Plan design o Coordinating with existing ERISA benefit plan(s) o Acting like ERISA applies o Involvement in plan administration, claims, etc. o Combination of factors 18 DOL Safe Harbor: Endorsement factors o Did employer play active role in determining who is eligible for benefits or other plan terms? o Is employer named as plan administrator? o Has employer provided plan description that refers to ERISA or is covered by ERISA? o Has employer provided materials suggesting it endorses program? o Does employer participate in claims processing? 19 Examples indicating employer “endorsement”: o ER urges EE participation or engages in activities that would lead an EE reasonably to conclude program is part of ER’s benefit program o ER is designated as plan administrator for purposes that are more than merely ministerial or ancillary to other activities within the safe harbor o ER is substantially involved in the creation or administration of the plan determining employee eligibility, selecting carrier, or negotiating terms of policy or benefits o ER distributed a booklet, embossed with its logo, to all employees, encouraging them to give the policy “careful consideration” as a “valuable supplement to [their] existing coverage,” o ER referred to the plan as “our plan,” and employed a full-time benefits administrator, who accepted claims forms and submitted them to the insurer 20 Examples indicating no employer “endorsement”: o ER files an IRS Form 5500, without more o EE dealt solely and directly with the carrier, paid 100% of the cost of the policy with after-tax dollars, and the ER made clear that participation was completely voluntary 21 DOL Safe Harbor: no consideration to employer – cash or otherwise – in connection with the program, other than reasonable compensation for administrative services actually rendered o No clear standard for what is permissible, reasonable o Tax advantages from payroll deductions themselves will not cause the employer to fail to meet this factor, but see pre-tax contribution issues under 2013-54. 22 Failing to meet DOL Safe Harbor means plan is subject to ERISA. FALSE o The plan may not provide a benefit covered by ERISA – home, auto, identity theft, pet insurance o The organization may not be an organization subject to ERISA – church, government, etc. o Plan may not be “maintained” by employer. 23 What does ERISA coverage mean for us? o Depends on factors such as: type of plan, type of employer, number of employee o ERISA fiduciary duty requirements o ERISA enforcement provisions o ERISA reporting and disclosure requirements o See our “ERISA: Basics and in Context” program June 2014 24 Reporting and Disclosure o Summary plan description • DOL specific content and furnishing requirements • Wraparound document • Practical Tip: Wrap is excellent compliance aid for voluntary plans o Annual reporting requirement • Small employer exception • Schedule A from carriers • DOL Delinquent filer voluntary compliance (DFVC) program 25 ERISA welfare plan that also is group health plan o COBRA o FMLA o USERRA o HIPAA – privacy/security and portability o ADA o GINA 26 In general, ACA (including the PHSA mandates) apply to group health plans. Many ACA (and PHSA) provisions do not apply to “excepted benefits” under HIPAA. o Non-health benefits, limited scope benefits, non-coordinated benefits and supplemental benefits. o Excepted benefits do not constitute minimum essential coverage (MEC) 27 What are excepted benefits? o Non-health benefits. Benefits that do not provide health coverage, such as liability insurance, automobile insurance, workers compensation and accidental death and dismemberment coverage. o Limited-scope benefits. Limited excepted benefits, such as limited-scope vision or dental benefits, long-term care, nursing home care, home health care or community-based care, as well as health FSAs that meet certain requirements. To fall into this category, the benefits must either • be provided under separate policy, certificate contract of insurance or • not be an integral part of a group health plan. 28 What are excepted benefits? o Non-coordinated benefits. Coverage for a specified disease or illness (e.g. cancer-only policies) and hospital indemnity or other fixed indemnity insurance. These benefits must meet the following requirements • Provided under a separate policy, certificate, or contract of insurance; • No coordination between the provision of such benefits and any exclusion of benefits under any group health plan maintained by the same plan sponsor; and • Benefits paid with respect to an event are made without regard to whether benefits are provided under any group health plan maintained by the same plan sponsor. 29 What are excepted benefits? o Supplemental benefits. Supplemental excepted benefits, which is coverage supplemental to Medicare, CHAMPVA or Tricare or to coverage provided under a group health plan, that is provided under a separate policy, certificate or contract of insurance. o Safe Harbor rules • Must be insurance policy, issued by entitled that is not offering the primary coverage • Fill gaps in existing coverage – payments of coinsurance deductibles • Cost must not be more than 15% of the primary coverage using COBRA • Not health factor discrimination. 30 W-2 Reporting o Dental and vision – optional o Hospital indemnity or specified illness, paid on after-tax basis – do not report o Hospital indemnity or specified illness, paid through salary reduction (pretax) or by employer – report o Other typical voluntary benefits disability, LTC, auto/home, workers compensation, supplemental liability, pre-paid legal – do not report Section 6055/6056 Reporting o No reporting required for excepted benefits 31 PCORI and Transitional Reinsurance Fees o Insurance policies and self-insured plans that provide only excepted benefits are not subject to PCORI or the Transitional Reinsurance Fee, including limited-scope dental and vision plans. Summary of Benefits and Coverage o Proposed SBC regulations issued in December 2014 confirm SBCs are not required for excepted benefits. 32 Voluntary benefits can be excellent addition to overall benefit program. Is it better to just tackle ERISA compliance? If not, be careful with “endorsement.” Tax-treatment of employee salary reduction contributions through salary reduction can have significant impact. Watch ACA implications for non-excepted health benefits! 33 Thank you for your participation in the UBA Employer Webinar Series If your question was not answered during the webinar or if you have a follow-up question, you can email the presenters today or tomorrow at: UBAwebinars@jacksonlewis.com www.UBAbenefits.com www.jacksonlewis.com To obtain a recording of this presentation, or to register for future presentations, contact your local UBA Partner Firm.