PowerPoint 演示文稿
advertisement

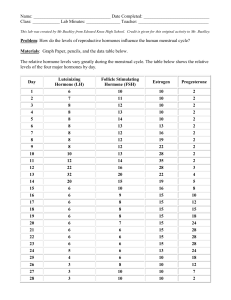
Chapter 12 Reproductive System The term “reproduction” usually means formation of new living entities, which closely resemble to the parent species. In higher animals, reproduction is accomplished by activities of both sexual organs of male and female. The processes are very complex including production of sperms and ova, sexual intercourse, fertilization of ovum, pregnancy, development of fetus and lactation. Section 1 Reproductive and Hormonal Functions of the Male Functions of testes: spermatogenesis in seminiferous tubules secrete hormones (testosterone and inhibin). I. Endocrine Function of Testes 1. Androgens Testes secrete several male sex hormones, which are collectively called androgens, including testosterone, dihydrotesterone and androstenodione. Testosterone is so much more abundant than the others that one can consider it the significant testicular hormone. (1) Functions of testosterone 1) Maintenance of spermatogenesis 2) Stimulation of development of genitalia. 3) Development and maintenance of the male secondary sexual characteristics. 4) Maintenance of libido. 5) Effect on metabolism. Testosterone increases anabolism of protein, especially that in muscle and genitalia, and causes growth of the bones in the thickness, deposition of calcium salts as well enhancement of production of red cells. 2. Inhibin Inhibin, a glycoprotein with a molecular weight of 31,000-32,000, has a potent inhibitory effect on FSH secretion by pituitary gland. The effect of inhibin on hypothalamus is slightly inhibitory in GnRH secretion. II. Regulation of Testis Function 1. Hypothalamic-Pituitary-Testis Axis (1) GnRH (gonadotropin – releasing hormone) GnRH is secreted by hypothalamus and transported to the anterior pituitary gland in portal blood. The function of GnRH is to stimulate the synthesis and release the two gonadotropins, LH and FSH. critinism, no GnRH secreted during the puberty, no development of the sexual organs, no reproductive ability (2) LH (Luteinizing hormone or interstitial cell stimulating hormone) LH and FSH are secreted by cells in the anterior pituitary gland. LH causes interstitial cell of Ldydig to synthesize testosterone by activating the cAMP second message system and to release testosterone. (3) FSH (follicle stimulating hormone) FSH stimulates Sertoil cells to produce ABP (androgen binding protein). ABP binds with testosterone and enters the seminiferous tubule, increasing the androgen concentration in tubule and promoting spermatogenesis. FSH stimulates Sertoil cell to produce and secrete inhibin, which plays a negative feedback mechanism for control of testis function. 2 Inhibin Inhibin has a strong direct effect on the anterior pituitary gland in inhibiting FSH secretion and a light effect on the hypothalamus in inhibiting GnRH secretion. These automatic feedback mechanisms can maintain a normal speed of spermatiogenesis, which is required for male reproduction function. Section 2 Reproductive and Hormonal Functions of the Female Organs and Function Ovaries –2 female sex glands Produce egg cells Produces the hormone, estrogen Uterus or Womb Muscular pear-shaped organ Where baby develops Fallopian Tubes Egg travels through these 2 tubes to the uterus Cervix Opening between the uterus & vagina Vagina Muscular tunnel from cervix to outside I. Menstruation, Ovulation and Hormonal Regulation The normal reproductive years of the female are characterized by monthly rhythmical changes of secretion of the female hormones and corresponding changes in the ovaries and sexual organs. This rhythmical pattern is called the female sexual cycle of menstrual cycle, which may be regarded as periodic preparation for fertilization and pregnancy. Its most conspicuous feature is the periodic vaginal bleeding that occurs with the shedding of the uterine mucosa, which is known as menstruation. The length of a menstrual cycle is about 28 days. Diagrammatic section of the ovary showing various stages in the life of a Graafian follicle: a primary oocyte developing into a fully mature follicle about to ovvlate, then turning into a corpus luteum and finally ending up as a corpus albicans. 1. Ovarian Cycle (1) Follicular phase; (2) Ovulation; (3) Luteal phase Phases of endometrial growth and menstruation during each monthly female sexual cycle. 2. Uterine cycle and menstruation (1) Proliferative phase (estrogen phase) (2) Secretory phase (progesterone phase) (3) Menstruation II. Endocrine Functions of Ovaries 1. Functions of Estrogen (1) On sexual organs. The principle function of estrogen is to cause cellular proliferation and growth of the tissues of the sex organs and other tissues related to production. Estrogen stimulates the development of sexual organs including ovaries, fallopian tubes, uterus, vagina and the external genitalia. (2) On secondary female sexual characteristics. Estrogen stimulates development of the secondary sex characteristics of female such as feminine figure, soft and smooth skin. It cause the breast to grow and to show mature appearance. (3) On metabolism. Estrogen causes a slight increase in total body protein, which result in growth-promoting effect on the sexual organs, the bones, the breasts and a few other tissues. Estrogen has a slight effect on retention of water and sodium by the kidney tubules. 2. Progesterone Functions of progesterone (1) Effect on uterus. By far the most important function of progesterone is to promote secretary changes in the uterine endometrium, thus preparing the uterus for implantation of the fertilized ovum and providing nutrition for the early dividing ovum. Progesterone decreases excitability and sensitivity to oxytocin of myometrium. It decreases the frequency and intensity of uterine contractions, thereby helping to prevent expulsion of the implanted ovum. (2) Effect on breasts. Progesterone promotes development of the tubules and alveoli of the breasts, causing the alveolar cells to proliferate, enlarge, and become secretary nature but not to secrete milk. (3) Thermogenic effect. Progesterone causes thermogenic effect and is responsible for the rise in basal body temperature at the time of ovulation. (4) Progesterone relaxes the smooth muscle of the blood vessels and digestive tracts. III. Hormonal control of the menstrual cycle Menstrual Cycle A woman is born with all the follicles she will have (~400,000). Most will not mature, ~ 400 will LH and FSH influence developing follicle, which produces estrogen (in particular, estradiol). An increase in estrogen results in peak levels of FSH and LH which trigger ovulation (positive feedback loop). Ovulation occurs – ovum ruptures from dominant follicle. High LH levels 12-36 hrs before ovulation mark division of follicular and luteal phases. Menstrual Cycle Luteal phase: follicle changes into a temporary endocrine organ known as corpus luteum Secretes several hormones, including progesterone, which helps prepare the lining of the uterus for implantation should the egg be fertilized In absence of fertilization, the endometrial lining sheds during menstruation. Menstrual Cycle If fertilization occurs, the corpus luteum continues to synthesize and secrete steroid hormones that maintain pregnancy for the first 4-6 weeks. Aided by another hormone, human chorionic gonadotropin (hCG), that is biologically similar to LH. hCG is secreted by cells in the conceptus destined to become the placenta menstrual cycle proliferative phase 1. stimulated by estrogen 2. rebuilds endometrium LH FSH secretory phase 1. stimulated by estrogen and estrogen progesterone 2. endometrium prepares forprogesterone implantation endometrium menstrual phase 1. lack of estrogen/progesterone proliferative 2. removes endometrium uterus secretory uterus Fig. 34-1: Events of the Menstrual Cycle Hypothalamus secretes GnRH Proliferative phase Follicular stage Anterior pituitary secretes LH and FSH Graafian follicle stimulated Ovaries release estrogen High estrogen levels inhibit FSH secretion, stimulate LH production Luteal stage Secretory phase LH makes mature follicle burst: ovulation LH makes corpus luteum secrete progesterone Progesterone inhibits LH secretion Menstrual phase Decreased LH and FSH levels Corpus luteum atrophies, stops making progesterone Decreased estrogen and progesterone levels stimulate GnRH secretion Cyclic changes in ovarian hormones secretion also cause cyclic changes in basal temperature. On the ay of the LH peak, when estrogen secretion begins to decline, there is a slight drop in basal body temperature. Starting about one day after the LH peak, the basal body temperature sharply rises as a result of progesterone secretion and remains elevated throughout the luteal phase of the cycle. The day of ovulation can be accurately determined by this method, making the method useful in increasing fertility if conception is desired. Since the day of the cycle in which ovulation occurs is quite variable in many women, however, the rhythm method is not reliable for contraception by predicting when the next ovulation occur. Section 4 Pregnancy I. Fertilization and Implantation II. Hormones of Placenta The placenta forms large quantities of human chorionic gonadotropin, estrogen, progesterone and human chorionic somatomammotropin, which are all essential to a normal pregnancy 1. Human Chorionic Gonadotropin (HCG) HCG is a glycoprotein with a molecular weight of 39,000. It is secreted by the syncytial trophoblast cells and can be measured in the blood 8 to 9 days after ovulation. The rate of secretion rises rapidly to reach maximum bout 10 to 12 weeks after ovulation and decreases to much lower value by 16 to 20 weeks after ovulation. It continues at this level for the remainder of pregnancy. This hormone is identical to LH in its effect and therefore is able to maintain the corpus letum past the time when it would otherwise regress. The secretion of estradiol and progesterone is thus maintained and menstruation is normally prevented. Diagnosis of the early pregnancy 2. Progesterone and Estrogen At the fifth to sixth week the mother’s corpus luteum begins to regress (even in the presence of hCG), but by this time the placenta is secreting more than sufficient amounts of steroids (estrogen and progesterone) to maintain the endometrium and prevent menstruation. During pregnancy, the extreme quantities of estrogen cause enlargement of uterus, breasts and mother’s female external genitalia, which are convenient t developing of fetus. Progesterone has a specific effect o decreasing the contractility of pregnant uterus, thus preventing uterine contractions from causing abortion. 3. Human Chorionic Somatomammotropin (HCS) HCS is a protein with molecular weight of 38,000. It begins to be secreted by the placenta at the 5th week of pregnancy. Secretion of HCS increases progressively throughout the remainder of pregnancy in direct proportion t the weight of placenta. HCS mainly stimulates growth of fetus and regulates metabolism of carbohydrate, fat and protein in both the fetus and the mother