biosafety. risk assessment.
advertisement

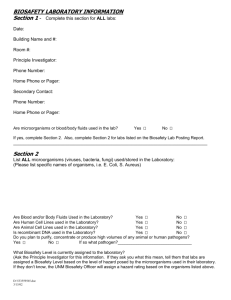
BIOSAFETY. BIORISK ASSESSMENT Dr. Gabriel Ionescu Cantacuzino Institute, “Carol Davila” U.M.Ph. Bucharest Biohazard definition (adapted from ISO/IEC Guide 51:1999) Potential source of harm caused by biological agents or toxins translated into Romanian PERICOL BIOLOGIC NU RISC BIOLOGIC Biorisk definition (adapted from ISO/IEC Guide 51:1999) • combination of the probability of occurrence of harm and the severity of that harm where the source of harm is a biological agent or toxin • NOTE The source of harm may be an unintentional exposure, accidental release or loss, theft, misuse, diversion, unauthorized access or intentional unauthorized release Specific guidelines Available on www.cantacuzino.ro See Section “Biosiguranta – Biosecuritate” Directives, guidelines, standards • • EU DIRECTIVES EU Directive 2000/54/EC of the European Parliament and of the Council of 18 September 2000 on the protection of workers from risks related to exposure to biological agents at work - HG 1092/2006 EC Directive on the Contained Use of Genetically Modified Organisms – OU 77 and 78 / 2007 GUIDELINES • • • • • • Laboratory Safety Manual - WHO Biosafety in Microbiological and Biomedical Laboratories (BMBL) - CDC The Laboratory Biosafety Guidelines - Health Canada Guidelines for Research Involving Recombinant DNA Molecules EC - NIH Biorisk management. Laboratory biosecurity guidance - WHO Biosafety risk assessment methodologies – Sandia Report STANDARDS • • • OHSAS 18001 ISO 15190:2003 - Medical laboratories - Requirements for safety CWA 15793:2008 - Laboratory biorisk management standard Biosafety definition • All measures that prevent accidentally exposure at biological agents (microorganisms and toxins) and infections and their released in environment See WHO Biosafety manual biological agent (adapted from EU Directive 2000/54/EC) any microorganism including those which have been genetically modified, cell cultures and endoparasites, which may be able to provoke any infection, allergy or toxicity in humans, animals or plants 2011 – The Year of Biosafety • EBSA announced 2011 “Year of Biosafety in Europe” as an initiative to support the newly established International Federation of Biosafety Associations (IFBA) • The European Centre for Disease Prevention and Control (ECDC) together with the European Biosafety Association (EBSA), a special session at 14th EBSA Annual Conference (April 13-15th, Portugal) to bring together laboratory and biosafety experts to discuss the development of effective pan-European biosafety networks Declaration of International Federation of Biosafety Association on Advancing Global Biosafety and Biosecurity 2011, the year of building international biosafety communities Longer-term goals • Promoting biosafety education, particularly of the younger generation, involving curriculum development within a common framework and a common methodology for evaluation. • Supporting appropriate and practical legislative framework development. • Developing a strategy to obtain funding for applied biosafety research programs Declaration of International Federation of Biosafety Association on Advancing Global Biosafety and Biosecurity Short term goals • Raising awareness from the political and public perspectives, and encouraging collaboration among the human and animal health communities • Developing sustainable biosafety associations and mapping gaps and needs • Providing advice to the competent national authorities and services for the improvement of efficient waste management (through disseminating knowledge of appropriate systems, tools and technologies for public and veterinary health environments). • Promoting human and laboratory capacity building with proper identification of gaps and needs (using the best available practices) concepts, principles and ECDC • EPIET and EUPHEM training programmes special modules in biosafety practices • exchange of biological materials • testing methods • training of laboratory staff • ECDC BioRisk Initiative for Capacity building and Knowledge base development (BRICK project) Biorisk assessment definition (adapted from OHSAS 18001:2007) Process of evaluating the biorisk(s) arising from a biohazard(s), taking into account the adequacy of any existing controls, and deciding whether or not the biorisk(s) is acceptable As defined by Kaplan and Garrick, risk analysis consists of answering three specific questions: • what can happen? • what is the chance that it will happen? • if it happens, what are the consequences?. Risk assessment strategy Characteristics • risk assessment is CAREFUL judgment • risk assessment is proactive rather than reactive • assessments can be qualitative, semi-quantitative or quantitative • risk assessment methodology should be: – identified – implemented – maintained • risk assessment is first step to control (reduce or eliminate) the hazards • risk assessment will provide a guide for the selection of appropriate - biosafety levels needs - microbiological practices - safety equipment - facility safeguards Assess the capability of the laboratory staff to control hazards - training - technical proficiency - good habits of all members of the laboratory - operational integrity of containment equipment - facility safeguards New risk assessment or review of an existing one when: • the introduction of new biological agents • new work or changes to the programme of work • alterations to work flow or volume • new construction / modifications to laboratories, equipment or its operation • introduction of altered and unplanned staffing arrangements New risk assessment or review of an existing one when: • significant alterations to Standard Operating Procedures (SOPs) or working practices (e.g. disinfection/waste management methodologies, PPE provision / usage entry/exit protocols, etc.); • unexpected events that may have relevance for the management of biorisks are observed New risk assessment or review of an existing one when: • actual or potential non-conformity with internal / external rules and regulations is identified • as part of the existing management system review process (e.g. annually or at another appropriate and predetermined frequency) Biorisk definition Biosafety risks are defined as a function of the likelihood of infection by the agent and the likelihood of exposure through an infectious route based on the procedures and work practices and the consequences of disease assuming infection Biosafety risks is a function of: • likelihood of – infection by the agent – exposure through an infectious route • consequences 4 scenarios • Risk to individuals in the laboratory • Risk to an individual outside the laboratory (the human community) • Risk to animals outside the laboratory (the animal community) • Risks to humans and animals resulting from a secondary exposure Routes of exposure • droplets or droplet nuclei (upper or lower respiratory tract) • compromised skin or direct injection into the blood stream • the mucosal membranes • the gastrointestinal tract Consequences of disease in humans assuming infection (1) • Does this agent or one of its by-products cause a carcinogenic or mutagenic reaction in a human host? • Does this agent have toxin or enzyme production which has a negative impact in a healthy human host? • Does this agent suppress a human host’s immune system? (E.g. cause dramatic suppression which renders the host susceptible other infections) • Does this agent have the ability to mutate once in a host or in the natural environment to become infectious through new route or new hosts, or to cause increased consequences? • What is the duration of illness (the average length of time of clinical signs of infection) in a normally healthy human host? • What is the severity of illness (the average severity of illness, ranging from no signs of illness to hospitalize in critical condition) in a normal health human host? • What is the duration of infection (the length of time the host is infected with the organism) in a normal healthy human host? Consequences of disease in humans assuming infection (2) • Does this disease cause any long-term conditions (sequelae) in a normal healthy human host? • What is the frequency of death in humans caused by this disease in a defined population during a specified interval of time (Mortality Rate)? • What level of national / international reporting is required for outbreaks of this disease? • Do effective diagnostic tests exist for humans? • Do post exposure treatments (including immuno-globulin, vaccines and antimicrobials) exist for humans? • Do preventative measures (vaccines) exist for humans? Consequences of disease in animals assuming infection • If the agent infects animals, what is the expected morbidity rate to a naive but otherwise healthy animal population? • What level of national or international reporting is required for outbreaks of this disease? • What species of animals can this agent infect? • Do effective diagnostic tests exist for animals? • Do post exposure treatments (including immunoglobulin, vaccines and antimicrobials) exist for animals? • o Do preventative measures (vaccines) exist for animals? The risk assessment should categorize risks • the use of a risk matrix identifying likelihood and consequence categories – e.g. high, moderate and low zones • the acceptability of risk levels should be defined • the inherent risk from the biological agents and toxins – e.g. from risk grouping descriptions, material safety data sheets etc. Risk assessment CAREFUL judgment biosafety levels ≠ risk group Ideally, a risk assessment should be conducted in a manner which is standardized and systematic allowing it to be repeatable and comparable. A risk assessment will determine the degree of correlation between an agent’s risk group classification and biosafety level Classification of infective microorganisms by risk groups • Risk Group 1 (no or very low individual and community risk) A microorganism that is unlikely to cause human or animal disease . • Risk Group 2 (moderate individual risk, low community risk) A pathogen that can cause human or animal disease but is unlikely to be a serious hazard to laboratory workers, the community, livestock or the environment. Laboratory exposures may cause serious infection, Effective treatment and preventive measures are available and the risk of spread of infection is limited. • Risk Group 3 (high individual risk, low community risk) A pathogen that usually causes serious human or animal disease but does not ordinarily spread from one infected individual to another. Effective treatment and preventive measures are available. • Risk Group 4 (high individual and community risk) A pathogen that usually causes serious human or animal disease and that can be readily transmitted from one individual to another, directly or indirectly. Effective treatment and preventive measures are not usually available. Relation of risk groups to biosafety levels, practices and equipment Risk group Biosafety level 1 Basic – Biosafety Level 1 2 Basic – Biosafety Level 2 3 Containment Biosafety Level 3 4 Maximum Biosafety Level 4 Laboratory type Laboratory practices Basic teaching, GMT research Safety equipment None; open bench work Primary health services;diagn. research GMT plus protective Open bench plus clothing, biohazard BSC for potential aerosols sign Special diagnostic, research As Level 2 plus special clothing, controlled access, directional air flow BSC and/or other primary devices for all activities Dangerous pathogens unit As level 3 plus airlock entry, shower exit, special waste disposal Class III BSC Positive presure suit + BSC II Double door autoclave Filtered air Biorisk Assessment Sheet Material Safety Data Sheet (MSDS) FINAL REMARKS Train and RETRAIN and RETRAIN and .. until good microbiological techniques and safety precautions become second nature Inadequate training on : - PPE use - correct use and maintenance of equipment FALSE sense of security