Cases in Primary Care - Christiana Care Health System
advertisement
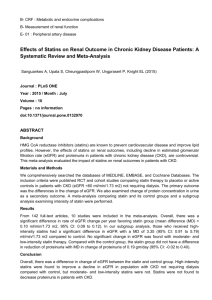
* Lauren Foy, D.O. APN Pharmacology Update March 28, 2014 * Identify the appropriate treatment for hypothyroidism, including appropriate medication dosing & monitoring * Appropriately prescribe & monitor statins, including differentiating between moderate & high intensity statins according to the 2013 ACC/AHA hyperlipidemia guidelines * Appropriately prescribe and manage antiviral treatment for shingles, including length of treatment and choice of agent * * 45 year old female presents to the office * CC: “I want my thyroid checked” * ROS: +fatigue, constipation, dry skin, steady weight gain over last few years * FHx: +thyroid disorder (mom, MGM) * PE: unremarkable, no thyromegaly or nodules palpated * Labs: TSH 7.5, FT4 <0.01 * * Dx: Hypothyroidism * Treatment: start thyroid replacement medication & monitor response * What dose of levothyroxine do I start? * How frequently do I need to recheck the thyroid? And which labs do I need to monitor? * What are the adverse effects? * * Thyroid hormone synthesis and secretion is regulated by the hypothalamic-pituitary-thyroid axis. * Thyrotropin-releasing hormone (TRH) released from the hypothalamus stimulates secretion of thyrotropinstimulating hormone, TSH, from the anterior pituitary. * TSH, in turn, is the physiologic stimulus for the synthesis and secretion of thyroid hormones, Lthyroxine (T4) and L-triiodothyronine (T3), by the thyroid gland. * Circulating serum T3 and T4 levels exert a feedback effect on both TRH and TSH secretion. * When serum T3 and T4 levels increase, TRH and TSH secretion decrease. * When thyroid hormone levels decrease, TRH and TSH secretion increase. * * * * Active ingredient: synthetic crystalline L3,3’,5,5’-tetraiodothyronine sodium salt [Levothyroxine (T4) sodium] * Synthetic T4 is identical to that produced in the human thyroid gland * * Synthetic form of thyroxine (T4), an endogenous hormone secreted by the thyroid gland * T4 converted to its active metabolite, Ltriiodothyronine (T3) * Thyroid hormones (T4 and T3) then bind to thyroid receptor proteins in the cell nucleus and exert metabolic effects: * control of DNA transcription and protein synthesis * involved in normal metabolism, growth, and development * promotes gluconeogenesis, increases utilization and mobilization of glycogen stores * stimulates protein synthesis * increases basal metabolic rate * * Repletion of T4 via daily levothyroxine dose exerts feedback to hypothalamus, restores homeostasis Via oral replacement with synthetic T4 * Decreased T4 secretion in hypothyroidism * Absorption of orally administered T4 from the gastrointestinal (GI) tract ranges from 40% to 80% * Majority of the levothyroxine dose is absorbed from the jejunum and upper ileum * T4 absorption is increased by fasting * T4 absorption is decreased in malabsorption syndromes, and by certain foods such as soybean infant formula. Absorption may also decrease with age. * Dietary fiber decreases bioavailability of T4. * * T4 is slowly eliminated * The major pathway of thyroid hormone metabolism is through sequential deiodination. * Approximately 80% of circulating T3 is derived from peripheral T4 by monodeiodination. * The liver is the major site of degradation for both T4 and T3, with T4 deiodination also occurring at a number of additional sites, including the kidney and other tissues. * Approximately 80% of the daily dose of T4 is deiodinated to yield equal amounts of T3 and reverse T3, which are are further deiodinated to diiodothyronine. * Thyroid hormones are also metabolized via conjugation with glucuronides and sulfates and excreted directly into the bile and gut where they undergo enterohepatic recirculation. * * Thyroid hormones are primarily eliminated by the kidneys. * A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. * Approximately 20% of T4 is eliminated in the stool. * Urinary excretion of T4 decreases with age. * * Adults: ~1.7 mcg/kg/day * usual doses are ≤200 mcg/day (range: 100-125 mcg/day [70 kg adult]) * doses ≥300 mcg/day are rare * consider poor compliance, malabsorption, and/or drug interactions * Elderly patients may require <1 mcg/kg/day * >50 years without cardiac disease or <50 years with cardiac disease: Initial: 25-50 mcg/day * adjust dose by 12.5-25 mcg increments at 6- to 8-week intervals as needed * >50 years with cardiac disease: Initial: 12.5-25 mcg/day * adjust dose by 12.5-25 mcg increments at 4- to 6-week intervals (many clinicians prefer to adjust at 6- to 8-week intervals) * * Walmart $4 list & Walgreens (Prescription Savings Club; $10 for #30) * Levothyroxine 25mcg tab * Levothyroxine 50mcg tab * Levothyroxine 75mcg tab * Levothyroxine 88mcg tab * Levothyroxine 100mcg tab * Levothyroxine 112mcg tab * Levothyroxine 125mcg tab * Levothyroxine 137mcg tab * Levothyroxine 150mcg tab * Levothyroxine 175mcg tab* * Levothyroxine 200mcg tab* * * No dose adjustment provided in manufacturer’s labeling * * Hypersensitivity to levothyroxine sodium or any component of the formulation * Acute MI * Thyrotoxicosis of any etiology * Uncorrected adrenal insufficiency * * Elderly do not have a change in serum thyroxine (T4) associated with aging; however, plasma T3 concentrations are decreased 25% to 40% in the elderly. * There is not a compensatory rise in thyrotropin (TSH) suggesting that lower T3 is not reacted upon as a deficiency by the pituitary * This indicates a slightly lower than normal dosage of thyroid hormone replacement is usually sufficient in elderly patients than in younger adult patients * TSH must be monitored closely: * insufficient thyroid replacement (elevated TSH) is a risk for coronary artery disease * excessive replacement (low TSH) may cause signs of hyperthyroidism and excessive bone loss * * Pregnancy category A * Endogenous thyroid hormones minimally cross the placenta * Levothyroxine has not been shown to increase the risk of congenital abnormalities. * Uncontrolled maternal hypothyroidism may result in adverse neonatal outcomes (eg, premature birth, low birth weight, and respiratory distress) and adverse maternal outcomes (eg, spontaneous abortion, pre-eclampsia, stillbirth, and premature delivery) * To prevent adverse events, normal maternal thyroid function should be maintained prior to conception and throughout pregnancy. * Levothyroxine is considered the treatment of choice for the control of hypothyroidism during pregnancy. * Due to alterations of endogenous maternal thyroid hormones, the levothyroxine dose may need to be increased during pregnancy and the dose usually needs to be decreased after delivery. * * * * * * * * * * * * Cardiovascular: Angina pectoris, cardiac arrest, cardiac arrhythmia, congestive heart failure, flushing, hypertension, increased pulse, myocardial infarction, palpitations, tachycardia Central nervous system: Anxiety, choking sensation (Levoxyl), emotional lability, fatigue, headache, heat intolerance, hyperactivity, insomnia, irritability, myasthenia, nervousness, pseudotumor cerebri (children), seizure (rare) Dermatologic: Alopecia, diaphoresis Endocrine & metabolic: Menstrual disease, weight loss Gastrointestinal: Abdominal cramps, diarrhea, dysphagia (Levoxyl), gag reflex (Levoxyl), increased appetite, vomiting Genitourinary: Infertility Hepatic: Increased liver enzymes Hypersensitivity: Hypersensitivity (to inactive ingredients; symptoms include urticaria, pruritus, rash, flushing, angioedema, GI symptoms, fever, arthralgia, serum sickness, wheezing) Neuromuscular & skeletal: Decreased bone mineral density, slipped capital femoral epiphysis (children), tremor Respiratory: Dyspnea Miscellaneous: Fever * In adult patients with primary hypothyroidism: * Serum TSH levels alone may be used to monitor therapy * Frequency of TSH monitoring during levothyroxine dose titration depends on the clinical situation but it is generally recommended at 6-8 week intervals until normalization. * For patients who have recently initiated levothyroxine therapy and whose serum TSH has normalized or in patients who have had their dosage of levothyroxine changed: * Serum TSH concentration should be measured after 8-12 weeks. * When the optimum replacement dose has been attained: * Clinical and biochemical monitoring may be performed every 6-12 months, depending on the clinical situation, and whenever there is a change in the patient’s status * Physical examination and a serum TSH measurement be performed at least annually * * The Levothyroxine in Levothyroxine sodium tablets, USP is intended to replace a hormone that is normally produced by your thyroid gland. Generally, replacement therapy is to be taken for life, except in cases of transient hypothyroidism, which is usually associated with an inflammation of the thyroid gland (thyroiditis). * Take Levothyroxine sodium tablets, USP as a single dose, preferably on an empty stomach, one-half to one hour before breakfast. Levothyroxine absorption is increased on an empty stomach. * Levothyroxine sodium tablets, USP may rapidly disintegrate. It is very important that you take the tablet with a full glass of water. * It may take several weeks before you notice an improvement in your symptoms. * Notify your physician if you experience any of the following symptoms: rapid or irregular heartbeat, chest pain, shortness of breath, leg cramps, headache, nervousness, irritability, sleeplessness, tremors, change in appetite, weight gain or loss, vomiting, diarrhea, excessive sweating, heat intolerance, fever, changes in menstrual periods, hives or skin rash, or any other unusual medical event. * Notify your physician if you become pregnant while taking Levothyroxine sodium tablets, USP. It is likely that your dose of Levothyroxine sodium tablets, USP will need to be increased while you are pregnant. * * TSH is the most reliable guide for evaluating adequacy of thyroid replacement dosage * Monitor TSH every 6-8 weeks until normalized; 8-12 weeks after dosage changes; every 6-12 months throughout therapy * Decreased dosing recommended in elderly/cardiac patients * Start low, go slow! * * 53 year old male * CC: “annual exam” * ROS: 10-point negative * FHx: CAD, father (MI @67); HLD, mother * PE: unremarkable * Labs: FLP, AST/ALT, FBS ordered * * FLP * LDL: 190 * HDL: 35 * TG: 175 * AST/ALT: WNL * FBS: 88 * * Dx: hyperlipidemia * Treatment: start statin, diet/exercise * What medication do I start? And at which dose? * What labs do I need to monitor? * What are the side effects? * Are there important interactions to worry about? * * * * Beneficial in patients with dyslipidemias for both primary and secondary prevention of coronary heart disease * * * Mechanisms by which lipid-lowering therapy (particularly with statins) is beneficial are incompletely understood * Lowering of low density lipoprotein (LDL) concentration is associated with regression of atherosclerosis * Observed benefit of (particularly statin) therapy begins within months after its initiation * Makes regression an unlikely cause at this early stage * Other mechanisms thought to be involved include: * plaque stabilization * reduction of inflammation * reversal of endothelial dysfunction * decreased thrombogenicity * Reduction in monocyte adhesion to the endothelium, reduced oxidative modification of LDL, and increases in mobilization and differentiation of endothelial progenitor cells * potential benefits from lipid lowering * * HMG CoA reductase (hydroxymethylglutaryl CoA reductase) inhibitors * competitive inhibitors of HMG CoA reductase, the rate-limiting step in cholesterol biosynthesis * occupy a portion of the binding site of HMG CoA, blocking access of this substrate to the active site on the enzyme * * (Livalo) * (Crestor) * * Chronic kidney disease presents an additional challenge for the selection of a statin * Atorvastatin and fluvastatin do NOT require dose adjustment * statins of choice in patients with severe renal impairment * If statins other than atorvastatin or fluvastatin are used, pravastatin may be safer than other statins * Dose adjustment is warranted with other statins in patients with severe kidney disease (CrCl less than 30 mL/min) * * Patients with chronic liver disease who require a statin because of high cardiovascular risk, suggest complete abstinence from alcohol and the use of pravastatin at a low dose. * If the LDL-C remains elevated, combined therapy with a bile acid sequestrant may allow such patients to achieve their LDL-C target * Statins are contraindicated in patients with progressive liver disease * Patients who simply have baseline elevations in aminotransferases do not appear to be at increased risk when prescribed a statin * * In 2012, the US FDA revised its labeling information on statins to only recommend liver function testing prior to initiation of statin therapy and to only repeat such testing for clinical indications * check baseline aminotransferase levels prior to initiating statin therapy * do NOT routinely monitor these levels in patients on statins * recommend changing medications or lowering the statin dose in patients who are found to have an alanine aminotransferase (ALT) level more than three times the upper limit of normal that is confirmed on a second occasion * 2013 ACC/AHA Blood Cholesterol Guideline recommendations (Stone, 2013): * Lipid panel (total cholesterol, HDL, LDL, triglycerides): Baseline lipid panel; fasting lipid profile within 4-12 weeks after initiation or dose adjustment and every 3-12 months (as clinically indicated) thereafter. If 2 consecutive LDL levels are <40 mg/dL, consider decreasing the dose. * Hepatic transaminase levels: Baseline measurement of hepatic transaminase levels (ie, ALT); measure hepatic function if symptoms suggest hepatotoxicity (eg, unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine or yellowing of skin or sclera) during therapy. * CPK: CPK should not be routinely measured. Baseline CPK measurement is reasonable for some individuals (eg, family history of statin intolerance or muscle disease, clinical presentation, concomitant drug therapy that may increase risk of myopathy). May measure CPK in any patient with symptoms suggestive of myopathy (pain, tenderness, stiffness, cramping, weakness, or generalized fatigue). * Evaluate for new-onset diabetes mellitus during therapy; if diabetes develops, continue statin therapy and encourage adherence to a heart-healthy diet, physical activity, a healthy body weight, and tobacco cessation. * If patient develops a confusional state or memory impairment, may evaluate patient for nonstatin causes (eg, exposure to other drugs), systemic and neuropsychiatric causes, and the possibility of adverse effects associated with statin therapy. Manufacturer recommendations: * Liver enzyme tests at baseline and repeated when clinically indicated. Upon initiation or titration, lipid panel should be analyzed at intervals of 4 weeks or more. * * Hypothyroidism as potential cause of dyslipidemia * Suggest checking a TSH level prior to initiating statin therapy * Hypothyroidism may predispose patients to statin-induced myopathy * Concerns have been raised that Asians may have greater responses to low doses of statins than Caucasians * Prescribing information for rosuvastatin recommends starting therapy at a lower initial dose in Asians than in other groups, given observed differences in pharmacokinetics * There is no strong evidence supporting such an approach with other statins. * 1% to 10%: * Cardiovascular: Chest pain (4%) * Central nervous system: Headache (2% to 6%), fatigue (4%), dizziness (1% to 3%) * Dermatologic: Rash (4%) * Gastrointestinal: Nausea/vomiting (7%), diarrhea (6%), heartburn (3%) * Hepatic: Transaminases increased (>3x normal on two occasions: 1%) * Neuromuscular & skeletal: Myalgia (2%) * Respiratory: Cough (3%) * Miscellaneous: Influenza (2%) <1%: * Allergy, alopecia, appetite decreased, dermatitis, dry skin, edema, fever, flushing, insomnia, lens opacity, libido change, muscle weakness, neuropathy, paresthesia, pruritus, sexual dysfunction, taste disturbance, tremor, urticaria, vertigo Postmarketing and/or case reports: * Amnesia (reversible), anaphylaxis, angioedema, cholestatic jaundice, cirrhosis, cognitive impairment (reversible), confusion (reversible), cranial nerve dysfunction, dermatomyositis, erythema multiforme, ESR increase, fulminant hepatic necrosis, gynecomastia, hemolytic anemia, hepatitis, hepatoma, lupus erythematosus-like syndrome, memory disturbance (reversible), memory impairment (reversible), myopathy, pancreatitis, peripheral nerve palsy, polymyalgia rheumatica, positive ANA, purpura, rhabdomyolysis, StevensJohnson syndrome, vasculitis Additional class-related events or case reports: * Angioedema, blood glucose increased, cataracts, depression, diabetes mellitus (new onset), dyspnea, eosinophilia, erectile dysfunction, facial paresis, glycosylated hemoglobin (Hb A1c) increased, hypersensitivity reaction, immune-mediated necrotizing myopathy (IMNM), impaired extraocular muscle movement, impotence, interstitial lung disease, leukopenia, malaise, memory loss, ophthalmoplegia, paresthesia, peripheral neuropathy, photosensitivity, psychic disturbance, skin discoloration, thrombocytopenia, thyroid dysfunction, toxic epidermal necrolysis, transaminases increased, vomiting * * Hepatic Dysfunction * Muscle Injury * Renal Dysfunction * Behavioral & Cognitive * Cancer * DM * * Clinical studies of statins have demonstrated a 0.5 to 3.0 percent occurrence of persistent elevations in aminotransferases in patients receiving statins * Primarily occurred during the first three months of therapy and is dose-dependent * * Options in patients with aminotransferase elevations (more than three times the upper limit of normal; confirmed on repeat testing) * Use of a different statin (particularly pravastatin) * Dose reduction * Alternate day therapy * * * * * * * Development of muscle toxicity remains a concern with the use of the statins Myopathic syndromes associated with statins span a spectrum of complaints ranging from myalgias to myositis to overt rhabdomyolysis, which may be associated with acute renal failure from myoglobinuria Muscle injury is uncommon with statin therapy alone * Frequency of 2 to 11 percent for myalgias, 0.5 percent for myositis, and less than 0.1 percent for rhabdomyolysis Muscle symptoms usually begin within weeks to months after starting statins * Myalgias, weakness, and serum CK concentrations usually return to normal over days to weeks after drug discontinuation * Pravastatin and fluvastatin appear to have less intrinsic muscle toxicity. Enhanced susceptibility to statin-associated myopathy occurs in patients with acute or chronic renal failure, obstructive liver disease, and hypothyroidism. Patients can experience statin-induced myalgias without an elevation in serum creatine kinase (CK) concentration * Clinical judgment is necessary in interpreting elevated CK levels in patients on statins * In the absence of clinical symptoms, a CK level >10 times the ULN that is felt to be due to a statin indication for discontinuing the medication * Patients should drink large quantities of fluids to facilitate renal excretion of myoglobin. After the CK and/or myoglobin have returned to baseline, patients may be tried on a statin less likely to cause muscle toxicity (as above) with careful monitoring. * * If a patient requires a statin and experiences muscle toxicity (other than rhabdomyolysis) with a statin other than pravastatin or fluvastatin, once symptoms have resolved off statin therapy, it is reasonable to consider a trial of pravastatin or fluvastatin with careful monitoring * Patients with a history of statin-induced rhabdomyolysis should generally NOT be treated with another statin (including pravastatin and fluvastatin), because of the risk of recurrence * * In some cases, it may be reasonable to retry statin therapy after the resolution of an acute reversible event that contributed to muscle toxicity (eg, undetected hypothyroidism, acute renal failure, biliary obstruction, use of other medications that increase statin levels) * Statins appear to be able to cause proteinuria through tubular inhibition of active transport of small molecular weight proteins * Have been a number of reports to the FDA about proteinuria with statins, particularly in patients receiving rosuvastatin or simvastatin * it is believed that proteinuria with statins is a benign finding * * Case reports of patients developing severe irritability and aggression associated with the use of statins * not known whether the statin use caused these symptoms * very rare idiosyncratic reactions of this sort could be missed in controlled trials * Concerns have been raised about cognitive dysfunction and memory loss associated with statin use * Review of adverse events reported to the FDA between November 1997 - February 2002 found 60 reports of patients who had memory loss associated with statins * apparently high rate of reports with lipophilic statins (simvastatin and atorvastatin; 36 & 23 patients affected respectively) compared with hydrophilic statins (pravastatin; 1 patient) does suggest a possible biologic effect * If an individual patient appears to have memory loss associated with lipophilic statin therapy (simvastatin, lovastatin, atorvastatin, or fluvastatin) and has a strong indication for lipid lowering therapy, it would be reasonable to attempt treatment with a more hydrophilic statin (pravastatin or rosuvastatin) * * Preclinical studies found that very high-dose statin therapy increased the risk of liver tumors in rodents * Meta-analyses of randomized trials have shown no effect of statins on cancer incidence or cancer mortality * * Experimental evidence has been conflicting about whether statins as a group improve glucose metabolism or whether some statins show beneficial effects while others show harmful effects * A 2011 meta-analysis of five randomized trials (N = 32,752) found an increased risk of incident diabetes with intensive statin therapy compared with moderate statin therapy (OR 1.12, CI 1.04-1.22) * Translates into approximately one additional case of diabetes for every 500 patients treated with intensive rather than moderate statin therapy. * Appears likely that statin therapy confers a small increased risk of developing diabetes * Risk is slightly greater with intensive statin therapy than moderate statin therapy. As would be expected, given the evidence from clinical trials that statins reduce CV events in patient with diabetes both randomized trials and observational studies suggest that the beneficial effects of statins on CV events and mortality outweigh any increased risk conferred by promoting the development of diabetes * * Rated category X in pregnancy * Recommendation is to discontinue their use prior to conception if possible * Animal studies indicate that at maternally toxic doses statins are associated with adverse fetal outcomes, but limited human data suggest that statins are not major human teratogens * analysis of an FDA surveillance database suggests possible increase in congenital central nervous system and limb abnormalities with exposure to lipophilic statins during the first trimester * Data on statin safety in breastfeeding are very limited * In absence of adequate safety data, use of statins by breastfeeding mothers is discouraged * * Lovastatin, atorvastatin, rosuvastatin, and simvastatin potentiate effect of warfarin * This interaction is not seen with pravastatin, fluvastatin, or pitavastatin * Most statins can also affect digoxin metabolism and levels * Rosuvastatin levels are increased by the protease inhibitor combinations lopinavir/ritonavir and atazanavir/ritonavir * Pravastatin is the statin of choice in patients on cyclosporine or gemfibrozil (or other fibric acid derivatives) * Increased rick of myositis and rhabdomyolysis with other statins * Should be used cautiously and only if the benefit is likely to outweigh the low risk of muscle toxicity. * Fenofibrate is the preferred fibrate in patients who require combined therapy with a statin. * In patients taking amlodipine, the dose of simvastatin should be no more than 20 mg daily. * * Risk of statin-induced muscle injury is substantially increased for most statins extensively metabolized by cytochrome P-450 3A4 (lovastatin, simvastatin and, to a lesser extent, atorvastatin) with concurrent therapy with drugs that interfere with CYP3A4 * Pravastatin, fluvastatin, rosuvastatin, and pitavastatin are preferred when concurrent therapy with a strong inhibitor of CYP3A4 cannot be avoided. * Grapefruit juice inhibits CYP3A4, however daily consumption of eight ounces or less of grapefruit juice, or one half of a grapefruit or less, is unlikely to increase the risk of an adverse interaction or muscle injury * * Typically recommended that the statins with shorter half-lives be administered in the evening or at bedtime * majority of cholesterol synthesis appears to occur at night presumably reflecting the effects of a fasting state * Lovastatin absorption is increased by food, and it should be administered with the morning and evening meals * Patients treated with statins should be alerted to report the new onset of myalgias or weakness * Limit consumption to eight ounces or less of grapefruit juice, or one half of a grapefruit or less daily * * Walmart/Target ($4 for 30-day supply) * Lovastatin 10mg, 20mg * Walgreens (Prescription Savings Club; $5-15 for 30-day supply) * Lovastatin 10- 40mg * Pravastatin 10-80mg * Simvastatin 5-80mg * * Statins are the most powerful drugs available for lowering LDL-C and are the most effective lipid lowering drugs for improving clinical outcomes when used for primary and secondary prevention of cardiovascular disease * The choice of statin depends upon a number of factors, including the degree of hyperlipidemia, pharmacokinetic properties, drug interactions, the presence of renal impairment, and cost. * * Pts with high CV risk or who require >35% reduction in LDL: suggest treatment with rosuvastatin, atorvastatin, or simvastatin * cause the greatest percentage change in LDL-C * Pts with CKD: suggest treatment with atorvastatin or fluvastatin * do NOT require dose adjustment * Pts with chronic liver disease who require a statin because of high cardiovascular risk: suggest complete abstinence from alcohol and the use of pravastatin at a low dose * Pts on multiple medications: consider pravastatin, fluvastatin, rosuvastatin, and pitavastatin because they are not metabolized through the CYP3A4 & fewer pharmacokinetic drug interactions are likely to occur * * 66 year old female presents to the office * CC: “I have a rash for the last 2 days” * ROS: +burning, itchy, painful rash on side, HA yesterday, resolved now, +malaise, denies fevers/chills, recent illness * PMHx: HTN, anxiety * FHx: unremarkable * PE: VSS, afebrile * * * Dx: Shingles (Zoster) * Treatment: start antiviral medication & monitor response * What antiviral do I choose? What dose do start? * Are there any labs I need to monitor? * What are the adverse effects? * * Characterized by painful vesicular eruptions in a dermatomal distribution * May be preceded by a prodromal phase with fever and malaise or pain over the affected dermatome * Lesions continue to form over a period of 3 to 5 days, and disappear, often with a degree of scarring, after 10 to 15 days * Chronic pain that may persist after the rash has healed is termed postherpetic neuralgia * occurs in about 10% of patients * Involvement of the trigeminal nerve can lead to sightthreatening ophthalmic herpes zoster * Herpes zoster may be more severe and extensive in immunocompromised patients but is rarely fatal * * Member of herpesviridae family * Causes 2 separate diseases: chickenpox (varicella) and herpes zoster (zoster, shingles) * Primary infection with VZV usually occurs in childhood and * results in chickenpox * In immunocompetent persons, chickenpox is self-limiting and results in lifelong immunity * Virus is not eliminated and remains dormant within sensory nerve ganglia * In later life or in immunocompromised persons, reactivation of the virus from the sensory nerve may occur and give rise to nerve pain and a dermatomal rash * Immunocompromised patients may develop a second episode of chickenpox Infection may be acquired through the respiratory tract via airborne droplets or by close contact with infected individuals * * * Can reduce the severity and duration of acute pain, minimize complications and propagation of the rash, and reduce viral shedding * Systemic antivirals are recommended for: * all immunocompetent patients who are over 50 years of age * have moderate to severe pain or rash * have non-truncal involvement. * Treatment should be started within 72 hours of the onset of the rash and is usually continued for 7 to 10 days. * Antiviral therapy may also be considered in those presenting 72 hours after the onset of the rash when: * there are skin, motor, neurological, or ocular complications * when new vesicles are still forming * in the elderly * those with severe pain. * Topical antivirals are not recommended. * * Antiviral therapy should be initiated within 72 hours of clinical presentation in patients greater than 50 years of age to maximize the potential benefits of treatment * Clinical utility of initiating acyclovir therapy more than 72 hours after the onset of lesions in the immunocompetent host is unknown * Treatment should be considered if new lesions are still appearing at that time of clinical presentation, indicating ongoing viral replication * Likely minimal benefit of antiviral therapy in the patient who has lesions that have encrusted. * The rapid initiation of therapy is particularly critical in the severely immunocompromised patient, such as the organ transplant recipient * Antiviral therapy should be initiated in all immunocompromised patients, even if they present after 72 hours * Immunocompromised hosts with disseminated zoster should be hospitalized for intravenous acyclovir therapy. * * Recommend antiviral therapy for patients >50 years of age with uncomplicated herpes zoster who present within 72 hours of clinical symptoms * Acyclovir, famciclovir, and valacyclovir have all demonstrated clinical benefit and safety in the treatment of herpes zoster in immunocompetent patients * Prefer valacyclovir or famciclovir compared with acyclovir based on the convenience of less frequent dosing * selection of drug may also be influenced by cost considerations. * Duration of treatment is seven days * Dosing is as follows: * Acyclovir 800 mg five times daily * Famciclovir 500 mg three times daily * Valacyclovir 1000 mg three times daily * * Efficacy of antiviral therapy in patients less than 50 years of age has not been as well studied * Risk of adverse events secondary to antiviral therapy is very low, and early treatment can decrease symptoms of acute neuritis and hasten resolution of cutaneous lesions * Generally give antiviral therapy to patients <50 years of age with herpes zoster who present within 72 hours of clinical symptoms * * No clinical trials examining the role of antiviral therapy in the pregnant woman with herpes zoster infection * Experience with acyclovir therapy in both HSV infection and varicella pneumonia suggests that this drug is safe in pregnancy (Category B) * Maternal varicella infection during pregnancy can lead to severe complications, such as congenital varicella with neonatal morbidity, maternal herpes zoster infection has not been associated with the development of congenital varicella * No evidence to suggest that the pregnant female is at increased risk for complicated disease. * Consensus panel of experts issued management guidelines for the pregnant woman with acute herpes zoster in 2007 * Suggested initiation of antiviral therapy in a pregnant women with severe zoster rash (eg, >50 lesions) to promote more rapid healing and in those with acute neuritis to lessen the severity and duration of pain * * Episodes of recurrent zoster are uncommon * Patients with recurrent zoster should be treated with antiviral therapy with similar dosing and duration as for a primary episode * In addition, patients who present with recurrent herpes simplex outside of the mouth or genital areas may be misdiagnosed with recurrent zoster * viral cultures or other detection assays should be performed when a diagnosis of recurrent zoster is being considered * * Administration within 48 to 72 hours of the onset of rash has demonstrated clinical benefit in the treatment of acute neuritis and in the prevention of post-herpetic neuralgia * Has been the mainstay of herpes zoster tx * Need for frequent daily dosing * 800mg PO 5 times daily x7-10days * * 9-[2-hydroxymethyl]guanine; a nucleoside analog * Selectively inhibits the replication of herpes simplex virus types 1 and 2 (HSV 1 & 2) and varicella-zoster virus (VZV) * After intracellular uptake, it is converted to acyclovir monophosphate by virally-encoded thymidine kinase * This step does not occur to any significant degree in uninfected cells and thereby lends specificity to the drug's activity * The monophosphate derivative is subsequently converted to acyclovir triphosphate by cellular enzymes * Acyclovir triphosphate competitively inhibits viral DNA polymerase by acting as an analog to deoxyguanosine triphosphate (dGTP) * Incorporation of acyclovir triphosphate into DNA results in chain termination since the absence of a 3' hydroxyl group prevents the attachment of additional nucleosides * Acyclovir triphosphate has a much higher affinity for viral DNA polymerase than for the cellular homolog, yielding a high therapeutic ratio * * * Modest oral bioavailability, ~15- 30% * decreases with higher doses * multiple oral doses of 200 to 800 mg yield steady-state peak plasma concentrations of 0.6 to 1.6 mcg/mL * IV doses at 5 to 10 mg/kg every eight hours results in concentrations of 10 to 20 mcg/mL * IV formulation should be used for serious infections such as disseminated varicella in an immunocompromised host * Not highly bound to plasma protein (~15%) * Achieves widespread tissue and fluid penetration * including the CSF, in which acyclovir concentrations are plasma ~50%of those in * Excretion is predominantly renal, both by glomerular filtration and tubular secretion * Plasma half-life is 2-3 hours in patients with normal renal function * dosage modifications are required in the presence of renal insufficiency, which is a risk factor for acyclovir-related neurotoxicity * * Acute Renal Failure * produced by the precipitation of relatively insoluble acyclovir crystals in the renal tubules * an occasional complication of intravenous therapy * Risk can be minimized by prior hydration (with the urine output maintained above 75 mL/hour) and slow drug infusion over one to two hours * Neurotoxicity * Rare reports of neurologic toxicity, particularly in patients with underlying renal failure, have included agitation, tremors, delirium, hallucinations, and myoclonus * Severe neurotoxicity, characterized by delirium and coma, has been described at doses as low as 800 mg twice daily in patients requiring dialysis * The potential for this complication is greater in patients treated with peritoneal dialysis, which is associated with minimal removal of acyclovir * Peritoneal Dialysis Pts: daily doses of 600 to 800 mg/day should lead to safe serum acyclovir concentrations * HD Pts: a loading dose of 400 mg followed by maintenance dosing of 200 mg twice daily plus 400 mg after each dialysis is recommended * Patients who develop serious neurotoxicity should be treated with hemodialysis to remove the drug. * CrCl 10-25 mL * Normal dosing regimen 800 mg 5 times daily Administer 800 mg every 8 hours CrCl <10 mL * Normal dosing regimen 800 mg 5 times daily Administer 800 mg every 12 hours * * No dosage adjustment provided in manufacturer's labeling * Use caution in patients with severe impairment * * Mycophenolate: May increase the serum concentration of AcyclovirValacyclovir. Acyclovir-Valacyclovir may increase the serum concentration of Mycophenolate * Risk C: Monitor therapy * Tenofovir: Acyclovir-Valacyclovir may decrease the excretion of Tenofovir * Risk C: Monitor therapy * Zidovudine: Acyclovir-Valacyclovir may enhance the CNS depressant effect of Zidovudine * Risk C: Monitor therapy * Zoster Vaccine: Acyclovir-Valacyclovir may diminish the therapeutic effect of Zoster Vaccine. * Management: When possible, discontinue antiviral agents with anti-zoster activity (i.e., acyclovir, valacyclovir, famciclovir) for at least 24 hours prior to and 14 days after receiving a live attenuated zoster vaccine * Risk X: Avoid combination * Oral: * >10%: Central nervous system: Malaise (≤12%) * 1% to 10%: * * Central nervous system: Headache (≤2%) Gastrointestinal: Nausea (2% to 5%), vomiting (≤3%), diarrhea (2% to 3%) Parenteral: * 1% to 10%: * * * * * Dermatologic: Hives (2%), itching (2%), rash (2%) Gastrointestinal: Nausea/vomiting (7%) Hepatic: Liver function tests increased (1% to 2%) Local: Inflammation at injection site or phlebitis (9%) Renal: BUN increased (5% to 10%), creatinine increased (5% to 10%), acute renal failure All forms: * <1%, postmarketing, and/or case reports: * Abdominal pain, aggression, agitation, anemia, anorexia, ataxia, coma, confusion, consciousness decreased, delirium, desquamation, disseminated intravascular coagulopathy (DIC), dizziness, dysarthria, encephalopathy, fatigue, fever, gastrointestinal distress, hallucinations, hematuria, hemolysis, hepatitis, hyperbilirubinemia, hypotension, insomnia, jaundice, leukocytoclastic vasculitis, leukocytosis, leukopenia, lymphadenopathy, mental depression, myalgia, neutrophilia, pain, psychosis, renal failure, renal pain, seizure, somnolence, sore throat, thrombocytopenia, thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS), thrombocytosis, visual disturbances * * Should be started within 72 hours of the appearance of the rash to be effective * More convenient dosing and increased bioavailability, without increasing side effects, make valacyclovir a favorable choice compared to acyclovir * Rapidly converted to acyclovir in vivo * provides a three- to fivefold increase in acyclovir bioavailability * Less frequent daily dosing than acyclovir * 1 g 3 times daily for 7 days * Has been shown to accelerate resolution of postherpetic pain. * * Valyl ester of acyclovir * Acting as an oral prodrug, valacyclovir is converted in vivo to acyclovir * Acyclovir, a nucleoside analog, is phosphorylated by virally-encoded thymidine kinase and subsequently by cellular enzymes, yielding acyclovir triphosphate, which competitively inhibits viral DNA polymerase * * The antiviral activity of valacyclovir reflects its in vivo conversion to acyclovir * Valacyclovir has three to fivefold greater oral bioavailability (about 55 percent) than acyclovir * Then undergoes rapid and extensive first-pass intestinal and/or hepatic hydrolysis to yield acyclovir and L-valine * Food does not affect absorption. * Valacyclovir, at a dose of 250 mg 4 times daily, generates essentially the same acyclovir AUC (area under the curve, or exposure over 24 hours) as oral acyclovir at a dose 800 mg five times daily * at a dose of 1000 mg 3 times daily, produces a similar acyclovir AUC as intravenous acyclovir at a dose of 5 mg/kg every eight hours * * When administered at approved doses (up to 1000 mg three times daily), valacyclovir has been remarkably well tolerated * * CrCl 30-49 mL/minute * 1 g every 12 hours * CrCl 10-29 mL/minute * 1 g every 24 hours * CrCl <10 mL/minute * 500 mg every 24 hours * * No dosage adjustment necessary * * Pregnancy Category B * no clear evidence of risk in humans despite the lack of controlled studies documenting safety * For certain patients, the potential benefits may outweigh the potential risks to the fetus * In order to monitor the outcome of pregnancies exposed to this drug, Glaxo Wellcome Inc. maintains a Valacyclovir in Pregnancy Registry * 800-722-9292, extension 39437 * >10%: * Central nervous system: Headache (13% to 38%) * Gastrointestinal: Nausea (5% to 15%), abdominal pain (1% to 11%) * Hepatic: ALT increased (≤14%), AST increased (2% to 16%) * Respiratory: Nasopharyngitis (≤16%) 1% to 10%: * Central nervous system: Fatigue (≤8%), depression (≤7%), fever (children 4%), dizziness (2% to 4%) * Dermatologic: Rash (≤8%) * Endocrine: Dysmenorrhea (≤1% to 8%), dehydration (children 2%) * Gastrointestinal: Vomiting (<1% to 6%), diarrhea (children 5%; adults <1%) * Hematologic: Thrombocytopenia (≤3%), mild leukopenia (≤1%) * Hepatic: Alkaline phosphatase increased (≤4%) * Neuromuscular & skeletal: Arthralgia (<1 to 6%) * Respiratory: Rhinorrhea (children 2%) * Miscellaneous: Herpes simplex (children 2%) * <1%, postmarketing, and/or case reports: * Acute hypersensitivity reactions (angioedema, anaphylaxis, dyspnea, pruritus, rash, urticaria); aggression, agitation, alopecia, anemia, aplastic anemia, ataxia, creatinine increased, coma, confusion, consciousness decreased, delirium, dysarthria, encephalopathy, erythema multiforme, facial edema, hallucinations (auditory and visual), hemolytic uremic syndrome (HUS), hepatitis, hypertension, leukocytoclastic vasculitis, mania, photosensitivity reaction, psychosis, renal failure, renal pain, seizure, tachycardia, thrombotic thrombocytopenic purpura (TTP), tremor, urinary precipitation, visual disturbances * * Mycophenolate: May increase the serum concentration of AcyclovirValacyclovir. Acyclovir-Valacyclovir may increase the serum concentration of Mycophenolate * Risk C: Monitor therapy * Tenofovir: Acyclovir-Valacyclovir may decrease the excretion of Tenofovir * Risk C: Monitor therapy * Zidovudine: Acyclovir-Valacyclovir may enhance the CNS depressant effect of Zidovudine * Risk C: Monitor therapy * Zoster Vaccine: Acyclovir-Valacyclovir may diminish the therapeutic effect of Zoster Vaccine. * Management: When possible, discontinue antiviral agents with anti-zoster activity (i.e., acyclovir, valacyclovir, famciclovir) for at least 24 hours prior to and 14 days after receiving a live attenuated zoster vaccine * Risk X: Avoid combination * * Initiate therapy as soon as possible after diagnosis and within 72 hours of rash onset * Well absorbed from the gastrointestinal tract * Rapidly converted in the intestinal wall and liver to the active compound penciclovir * broad activity against VZV * 500 mg every 8 hours for 7 days * Famciclovir has been shown to accelerate healing, reduce the duration of viral shedding, and resolve posthepatic neuralgia faster than placebo * * Oral prodrug, converted by first-pass metabolism to the antiviral drug penciclovir * Penciclovir, upon intracellular uptake, is monophosphorylated by virally-encoded thymidine kinase * Subsequently, converted to a triphosphate by cellular enzymes * Penciclovir triphosphate preferentially inhibits the DNA polymerase of susceptible viruses * at clinically relevant levels, there is no substantial effect upon cellular DNA polymerase, thereby minimizing side effects to the host * mechanism is similar to that described for acyclovir * compared to acyclovir triphosphate, penciclovir triphosphate has a lower affinity for viral DNA polymerase but a longer intracellular half-life * * * Well absorbed, featuring an oral bioavailability of 77% * Prompt first-pass metabolism in the intestine and liver results in conversion to penciclovir * 500 mg dose of famciclovir yields peak penciclovir levels of 2.7 to 4.0 mg/L, with a plasma half-life of 2.1 to 2.7 hours * Food has no clinically important effect upon these levels * Prolonged intracellular half-life of penciclovir triphosphate: 7 to 14 hours in VZV-infected cells. * In comparison, the intracellular half-life of acyclovir triphosphate is one hour or les as a result, famciclovir requires less frequent dosing * Excretion is primarily renal * dose reduction is recommended in patients with impaired renal function * Penciclovir is removed by hemodialysis * Well-compensated chronic liver disease does not require dose modification, but pharmacokinetic studies in patients with poorly compensated hepatic insufficiency have not been performed * * Very well tolerated, with a side effect profile similar to those of placebo and oral acyclovir * although long-term safety data are unavailable * A review of over 1600 patients receiving famciclovir for herpes zoster or genital herpes revealed an adverse event profile not significantly different from placebo * * CrCl ≥60 mL/minute * No dosage adjustment necessary * CrCl 40-59 mL/minute * Administer 500 mg every 12 hours * CrCl 20-39 mL/minute * Administer 500 mg every 24 hours * CrCl <20 mL/minute * Administer 250 mg every 24 hours * Hemodialysis: Administer 250 mg after each dialysis session. * * Mild-to-moderate impairment: * No dosage adjustment is necessary * Severe impairment: * No dosage adjustment provided in manufacturer’s labeling; has not been studied * However, a 44% decrease in the Cmax of penciclovir (active metabolite) was noted in patients with mild-to-moderate impairment; impaired conversion of famciclovir to penciclovir may affect efficacy. * * Pregnancy Category B * animal studies suggest safety, although there have been no adequate studies in pregnant women * In some cases, the potential benefits of therapy may outweigh the potential risks to the fetus * In order to monitor the outcomes of pregnancies exposed to this drug, SmithKline Beecham maintains a Famvir Pregnancy Registry at 800-366-8900, ext. 5231 * * Zoster Vaccine: Famciclovir may diminish the therapeutic effect of Zoster Vaccine * Management: When possible, discontinue antiviral agents with anti-zoster activity (i.e., acyclovir, valacyclovir, famciclovir) for at least 24 hours prior to and 14 days after receiving a live attenuated zoster vaccine. * Risk X: Avoid combination * >10%: * Central nervous system: Headache (9% to 39%) * Gastrointestinal: Nausea (2% to 13%) 1% to 10%: * Central nervous system: Fatigue (1% to 5%), migraine (1% to 3%) * Dermatologic: Pruritus (≤4%), rash (≤3%) * Endocrine & metabolic: Dysmenorrhea (≤8%) * Gastrointestinal: Diarrhea (2% to 9%), abdominal pain (≤8%), vomiting (1% to 5%), flatulence (≤5%) * Hematologic: Neutropenia (3%) * Hepatic: Transaminases increased (2% to 3%), bilirubin increased (2%) * Neuromuscular & skeletal: Paresthesia (≤3%) <1%, postmarketing, and/or case reports: * Anemia, angioedema (eyelid, face, periorbital, pharyngeal edema), cholestatic jaundice, confusion, delirium, disorientation, dizziness, erythema multiforme, hallucinations, leukocytoclastic vasculitis, palpitations, somnolence, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis, urticaria * * Walmart/Target ($4 List) * Acyclovir 200mg * Walgreens (Prescription Savings Club; $10 for #60; $20 for #180) * Acyclovir 200mg * Remember dosing: Acyclovir 800 mg 5x/day * If using 200mg pills 20 pills/day! * * * *Questions? * * * * * Levothryoxine. http://www.drugs.com/pro/levothyroxine.html * Chong PH, Seeger JD, Franklin C. Clinically relevant differences between the statins: implications for therapeutic selection. Am J Med 2001; 111:390. * Cohen DE, Anania FA, Chalasani N, National Lipid Association Statin Safety Task Force Liver Expert Panel. An assessment of statin safety by hepatologists. Am J Cardiol 2006; 97:77C. * Edison RJ, Muenke M. Central nervous system and limb anomalies in case reports of first-trimester statin exposure. N Engl J Med 2004; 350:1579. * * * Hosokawa A, Bar-Oz B, Ito S. Use of lipid-lowering agents (statins) during pregnancy. Can Fam Physician 2003; 49:747. * * Liao JK. Safety and efficacy of statins in Asians. Am J Cardiol 2007; 99:410. * * Newman TB, Hulley SB. Carcinogenicity of lipid-lowering drugs. JAMA 1996; 275:55. * Rojas-Fernandez CH, Cameron JC. Is statin-associated cognitive impairment clinically relevant? A narrative review and clinical recommendations. Ann Pharmacother 2012; 46:549. * Smith CC, Bernstein LI, Davis RB, et al. Screening for statin-related toxicity: the yield of transaminase and creatine kinase measurements in a primary care setting. Arch Intern Med 2003; 163:688. * Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM. Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy 2003; 23:871. * Wang KL, Liu CJ, Chao TF, et al. Statins, risk of diabetes, and implications on outcomes in the general population. J Am Coll Cardiol 2012. Statins: Actions, side effects, and administration. UpToDate. Antons KA, Williams CD, Baker SK, Phillips PS. Clinical perspectives of statin-induced rhabdomyolysis. Am J Med 2006; 119:400. Carter AA, Gomes T, Camacho X, et al. Risk of incident diabetes among patients treated with statins: population based study. BMJ 2013; 346:f2610. Istvan ES, Deisenhofer J. Structural mechanism for statin inhibition of HMG-CoA reductase. Science 2001; 292:1160. Kasiske BL, Wanner C, O'Neill WC, National Lipid Association Statin Safety Task Force Kidney Expert Panel. An assessment of statin safety by nephrologists. Am J Cardiol 2006; 97:82C. Miettinen TA. Diurnal variation of cholesterol precursors squalene and methyl sterols in human plasma lipoproteins. J Lipid Res 1982; 23:466. Ridker PM, Pradhan A, MacFadyen JG, et al. Cardiovascular benefits and diabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial. Lancet 2012; 380:565. * * * "Acyclovir (Systemic)." LexiComp. N.p., n.d. Web. * * * * * * * * * * * Cunningham AL, et al.. The prevention and management of herpes zoster.Med J Aust. 2008; 188: 171–6. * Perry CM, Faulds D. Valaciclovir. A review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in herpesvirus infections. Drugs 1996; 52:754. * * * “Valacyclovir (Systemic)." LexiComp. N.p., n.d. Web. * Wood MJ, Kay R, Dworkin RH, et al. Oral acyclovir therapy accelerates pain resolution in patients with herpes zoster: a metaanalysis of placebo-controlled trials. Clin Infect Dis 1996; 22:341. BSSI Working Group. Guidelines for the management of shingles: report of a working group of the British Society for the Study of Infection (BSSI).J Infect. 1995; 30: 193–200. Dworkin RH, et al.. Recommendations for the management of herpes zoster.Clin Infect Dis. 2007; 44 1–S26 “Famcicilovir (Systemic)." LexiComp. N.p., n.d. Web. Famvir (famciclovir) prescribing information. SmithKline Beecham, 1997. Feldman S, Rodman J, Gregory B. Excessive serum concentrations of acyclovir and neurotoxicity. J Infect Dis 1988; 157:385. Gnann JW Jr, Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med 2002; 347:340. Gnann JW Jr. New antivirals with activity against varicella-zoster virus. Ann Neurol 1994; 35 Suppl:S69. Gross G, et al.. Herpes zoster guideline of the German Dermatology Society (DDG).J Clin Virol. 2003; 26: 277–89. Hirsch MS, Swartz MN. Drug therapy: antiviral agents (second of two parts). N Engl J Med 1980; 302:949. HOPE-SIMPSON RE. THE NATURE OF HERPES ZOSTER: A LONG-TERM STUDY AND A NEW HYPOTHESIS. Proc R Soc Med 1965; 58:9. Perazella MA. Drug-induced renal failure: update on new medications and unique mechanisms of nephrotoxicity. Am J Med Sci 2003; 325:349. Valtrex (valacyclovir hydrochloride) Product Information, Glaxo Wellcome Inc, 1996. Vere Hodge RA. Famciclovir and penciclovir: The mode of action of famciclovir including its conversion to penciclovir. Antiviral Chem Chemother 1993; 4:67. *