Protection of Human Subjects - American Occupational Therapy
advertisement

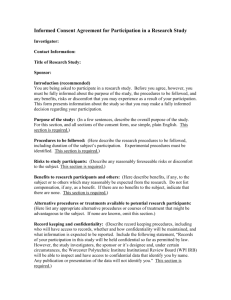
Promoting Integrity in the Next Generation of Researchers A Curriculum for Responsible Conduct of Research in Occupational Therapy (2005) Funded by the Office of Research Integrity through the American Association of Medical Colleges Protection of Human Subjects Occupational therapy documents typically refer to human subjects as participants. The terms are used interchangeably in this PowerPoint Objectives Discuss the historical abuses of participants that influenced guidelines for human subject research. Describe the three Belmont Report principles that guide ethical conduct of research. Compare and contrast the goal of treatment to that of research, and the rights of a patient to those of a research participant. Appreciate the role of institutional review boards (IRBs), and the need for occupational therapists to serve on these boards. Objectives (continued) Differentiate the process of informed consent from a consent or assent document. Describe the types of IRB reviews. Describe the content required in a consent form. Commit to being honorable in participant recruitment and selection, gaining informed consent, participant assessment and intervention, and management and use of data and records. Given case studies, recognize human subjects issues and discuss ways to prevent and/or resolve these problems. Why Weren’t Research Ethics a Part of Early Medical Doctors’ Training? Medical research relies on human subjects. Medical research was commonly performed by MDs. MDs were presumed ethical and were rarely supervised in their assessment and intervention with patients. By association, it was assumed that research by MDs was ethical, and medical researchers were rarely supervised in their efforts to make discoveries about diseases and treatment. Abuse Led to Rules for Human Research Questions about research arose because of failed ethics: Nazi medical experiments in concentration camps 1930-1945 Federally funded Tuskegee syphilis study 19321972 Human Radiation Studies 1944-1974 Examples from the news Nazi Medical War Crimes So-called medical experiments conducted on uninformed and unwilling concentration camp prisoners After WWII, 20 MDs & 3 laypersons found guilty of “crimes against humanity”. Most carried through to death 7 sentenced to death, the others to 10 yrs to life imprisonment Resulted in the NUREMBERG CODE First international code of medical research ethics (United States Holocaust Memorial Museum, n.d.) Tuskegee Syphilis Study (1932-1972) A classic example of a slippery slope. Initially a legitimate study conducted by researchers with good intentions, it becomes one that is horrifically unethical. Tuskegee Syphilis Study (continued) The Ethical Beginning 1926 An estimated 35% of men of reproductive age have syphilis. There is no effective and safe treatment 1929 Drs. Clark and Vondelehr at Tuskegee begin research on effects of topical Mercury and Bismith on syphilis. Funding lost after Wall Street Crash reduces foundation funds. 1931 Drs. Clark and Vondelehr continue to follow participants to show need for treatment program (Centers for Disease Control and Prevention, 2005) Tuskegee Syphilis Study (continued) The Slippery Slope 1932 US Public Health Services funds "Tuskegee Study of Untreated Syphilis in the Negro Male” to document natural course of syphilis in black men and possibly justify treatment programs for African Americans. At the time there is no safe effective treatment for syphilis 399 poor black sharecroppers with syphilis and 201 men without (controls) agree to participate. They are falsely told that some of the assessments being performed (e.g. spinal taps) are treatment. (Centers for Disease Control and Prevention, 2005) Tuskegee Syphilis Study (continued) The Slippery Slope (continued) 1934-36 Study begins publishing findings. Infrequent concerns are raised about whether the men are receiving any treatment. There is no general outcry. 1940s Local black and white MDs agree not to treat the study men for syphilis. Study is widely known in Tuskegee and few questions are raised. (Centers for Disease Control and Prevention, 2005) Tuskegee Syphilis Study (continued) The Clear Unethical Turn 1945 Penicillin becomes known as an effective and safe drug for syphilis. 1947 Penicillin readily available to the US poor via federally funded Rapid Treatment Centers (RTCs) established to treat poor people with syphilis. Participants are denied access to Penicillin from all controllable sources (e.g., RTCs, general public clinics, local black and white MDs, Armed Forces). Participants not given option to withdraw from study. (Centers for Disease Control and Prevention, 2005) Tuskegee Syphilis Study (continued) The Fallout 1968 Public concerns raised about ethics of the study 1969 Center for Disease Control and AMA defend study’s continuation 1970 Newspaper and magazine articles condemn the study 1971 Congress holds hearings 1972 Front-page NY Times article causes large public outcry 1972 Per panel recommendation, the study is ended 1973 Class action suit - participants compensated with cash and continued medical care for themselves and their families. (Centers for Disease Control and Prevention, 2005) Tuskegee Syphilis Study (continued) The Effect on US Policy 1974 National Research Act, creates the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research Requires that all researchers get voluntary informed consent from all research participants in Dept. of Health, Education and Welfare funded studies. 1997 President Bill Clinton apologizes to all participants and their families on behalf of nation. Reparations paid (Centers for Disease Control and Prevention, 2005) What Guides Responsible Study of Humans? Since the 1974 National Research Act, the Belmont Report (the result of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research) has been the dominant research ethics statement Belmont Report Principles Autonomy/ Respect Beneficence Justice Principle of Autonomy/Respect Persons have a right to decide if they will or will not participate in a study Persons who cannot make a competent decision (i.e., vulnerable individuals) must be protected by outside decision makers and must be closely monitored Persons invited to participate must know & understand risks and benefits, and be informed if these change while in the study Individuals may decline or withdraw without penalty Children must give assent before participating in study Principle of Beneficence Research design and method should yield valid results If possible, do no harm If harm in an inescapable risk, minimize it and maximize direct benefits to study participants Inform participants of risk and benefits. Principle of Justice Access to risk & benefit must be fairly distributed in society. Studies should not exclude by age, race, sex, etc. without strong reason. When possible, studies should randomly assign participants to treatment groups to ensure that risk and benefits are equally distributed MDs should not be excluded or included differently than others The Unexpressed Belmont Principle The researcher cannot decide whether she or he is conducting reasonable research, meeting ethical requirements, or has a conflict of interest The Tuskegee studies (among others) show that researchers can be myopic when it comes to their own studies. There must be external review and oversight by individuals and groups not directly involved in the study. Differences Between Being a Patient and Being a Research Participant Based on an idea presented at the 1999 American College of Rheumatology/ Association of Rheumatology Health Professionals Annual Conference - author unknown A Difference in Goals Goal of TREATMENT: To improve patient’s condition or state Goal of RESEARCH: To answer a question A Difference in Rights PATIENTS 1) Must be provided effective treatment, if known; or the treatment thought to be most likely to be effective in their case PARTICIPANTS 1) May receive no treatment (i.e., control) or a treatment that is purposely neutral (i.e., placebo) A Difference in Rights (continued) PATIENTS 2) Cannot be treated in a manner that risks harm, unless there is high likelihood of benefit PARTICIPANTS 2) May be intentionally treated in a manner that carries risk if such risk is monitored, all risk is as low as possible, and subject is informed of risks. The likelihood of benefit may be unknown A Difference in Rights (continued) PATIENTS 3) Are responsible for costs related to treatment PARTICIPANTS 3) Are generally NOT expected to pay costs associated with experimental assessment or intervention A Difference in Rights (continued) PATIENTS 4) Do not need to give formal consent to the process of occupational therapy treatment. It is implied. PARTICIPANTS 4) Must give formal consent to the process of randomization and experimental assessment and intervention – regardless of group assignment A Difference in Rights (continued) PATIENTS 5) Participation and results are shared with referring physician as required by state rules regarding documentation PARTICIPANTS 5) Results or status of participation cannot be shared with anyone outside of study without formal permission of subject A Difference in Rights (continued) PATIENTS 6) Must be accurately informed of the treatment s/he is receiving. 6) PARTICIPANTS May be intentionally deceived if a) b) c) there is low risk of injury, persons are properly debriefed at earliest opportunity, and persons are given right to withdraw data postdebriefing. A Difference in Rights (continued) PATIENTS PARTICIPANTS 7) Records are kept under 7) Records are private, individual’s name and kept under code, and carry identifiable may be reviewed only elements. They may be by those individuals reviewed by anyone described in the with legitimate access consent form or an to charts, as permitted examining body. MD by state and federal of participant may not law. automatically access A Difference in Rights (continued) PATIENTS PARTICIPANTS 8) May or may not be fully 8) Must be fully informed informed about about alternatives to alternative treatment participation in options. research. This includes the option to decline to participate and alternative treatments. Occupational Therapist Researchers Are Also Guided By… AOTA Code of Ethics Federal Rules/Regulations Educational Institution’s Rules/Regulations Hospital/Clinic/Center Rules/Regulations AOTA Code of Ethics (Principle 3) (American Occupational Therapy Association, 2000) Occupational therapy personnel shall respect the recipient and/or their surrogate(s) as well as the recipient's rights. (autonomy, privacy, confidentiality) Occupational therapy practitioners/personnel shall: C. Obtain informed consent from participants involved in research activities and indicate that they have fully informed and advised the participants of potential risks and outcomes. …(and) ensure that the participants comprehend these risks and outcomes. D. Respect the individual's right to refuse professional services or involvement in research or educational activities. E. Protect all privileged confidential forms of written, verbal, & electronic communication gained from educational, practice, research, and investigational activities unless otherwise mandated by local, state, or federal regulations. Federal Rules and Regulations Seventeen federal agencies have regulations governing research involving humans. Contracts and grants from these agencies require that rights of participants be ensured and overseen by both federal and institutional bodies Academic Institutions’ Rules and Regulations Educational institutions generally require that all faculty & all students performing research have their studies reviewed by the College or University Institutional Review Board (IRB) or Human Subjects Protection Office. This is typical regardless of research locale, regardless of whether faculty/students are being paid or conducting the research gratis, and regardless of whether faculty/student are conducting the research as part of their faculty/student roles or as external jobs. INSERT YOUR INSTITUION’S HUMAN SUBJECTS REGULATIONS HERE Hospital & Clinic Rules and Regulations Generally include that : Employees involved in research be trained and approved Employees involved in research gain IRB approval, even if the research is not on-site. If the institution does not have an IRB, it may accept approval from another institution’s. Institutional Review Board (IRB) IRB Uses prospective review. Review and permission required before any research takes place Assign review type based on level of risk vs benefit, and according to the Federal guidelines: Exempt = public info, use of anonymous data, no subject contact Expedited (quicker - single reviewer) = low risk, adults, typical daily activities Full committee (requires individual review followed by discussion of committee) research on children, study of treatment or assessment that have risk, sensitive topics The IRB, not the researcher, makes category decision IRB (continued) The IRB must review each study: Regardless of the type of study (qualitative vs. quantitative; descriptive vs experimental; natural history vs intervention), and Regardless of the researcher (student vs faculty) For IRB Process, Timeline or Forms Go To Insert your institution’s IRB website here After Initial Approval, IRB Monitors Research Studies Re-review at least annually Audit a selection of studies to ensure all processes being performed as promised. The Consent Form The Consent Form is only 1 part of the informed consent process Consent forms should be readable at <8th grade reading level Consent Forms are used for adults >18 years old Assent Forms are used for subjects 8-17 years old Verbal or nonverbal consent/assent can be accepted for young children, non-competent persons & nonliterate adults Nonverbal consent/assent may be documented by witness or by videotape/ audiotape of explanation and participant response Contents of Consent Form (Elements of Informed Consent, 21 C.F.R. § 50.25, 2000) Purpose and details of the research study, including description of drugs or devices (tools or pieces of equipment) or procedures used in the research study and type of assignment and odds of assignment to different study groups. Identification of the researching individuals and affiliations. Students should be identified as students, but should not indicate that the research is to complete degree requirements Explanation of research procedures, schedule and timeline of the research study. Costs of research procedures, drugs, devices, etc. and who is responsible to pay. Differentiation of research expenses from those of usual care. Contents of Consent Form (continued) Payment or non-payment to participant. Risks, dangers, and discomforts of the study, and means that will be used to control for these. Benefits and advantages of participating in the research study. Direct benefits, not payment or good to society. Alternatives to study participation. Medical treatment available if participant is injured by the research, and who will pay for this treatment. Contents of Consent Form (continued) Who, if anyone, will have access to subject data, and whether study results will identify participant Will study create or use any Protected Health Information (PHI), and if data will be part of chart. Assurance that participation is voluntary and person may quit without affecting future treatment or current relationships. Description if treatment requires withdrawal or monitoring after quitting. Statement that data may be withdrawn from study or why this is not possible. Contents of Consent Form (continued) Assurance that new information will be shared with participants Chance to ask questions about the research study. Outside-of-study contact information. Place to sign consent/assent form, Notice that they will be given a copy of signed/dated form for their records. Place for investigator to sign, date form. Place for witnesses signature/date, if witness is needed Consent Forms for Non-English Speakers Download free generic Consent Short Forms in 11 languages (Arabic, Croatian, French, Hmong, Khmer, Lao, Oromo, Russian, Somali, Spanish, and Vietnamese) from http://www.research.umn.edu/irb/consent/downloadshortfor ms.cfm Generic forms may be used with more detailed oral explanation, to obtain consent from occasional non-English speaking participants. Generic forms cannot substitute for properly translated consent form in studies of primarily non-English speakers. Adverse Events & Unexpected Experiences Definitions Adverse events are any experience that suggests a significant hazard, contraindication, side effect, or precaution – even if it is already listed as possible in IRB materials Unexpected adverse experiences are any adverse experience whose nature, severity, & incidence are not described in the information provided for IRB review or in the consent form Immediately report events/experiences to the IRB & change procedure and consent accordingly. If event/experience is significant, IRB may pause or stop study Unanticipated Problems or Events Report unanticipated problems that might affect subject Risk/benefit analysis, Confidentiality, Participants’ willingness to continue The IRB will consider the effect of the problem on the study and on the participants already enrolled. Events at Other Institutions If a research project involves many institutions and the event occurred at another institution, inform your IRB of event, severity, likelihood that it could occur at your institution, and implications for your future subjects. Resources American Occupational Therapy Association (2000). Occupational Therapy Code of Ethics. Retrieved September 11, 2005, from http://www.aota.org/general/coe.asp. Centers for Disease Control and Prevention (2005). The Tuskegee Timeline. Retrieved September 11, 2005 from http://www.cdc.gov/nchstp/od/tuskegee/time.htm. Elements of Informed Consent, 21 C.F.R. § 50.25 (2000). Retrieved August 20, 2005, from http://frwebgate.access.gpo.gov/cgi-bin/getcfr.cgi?TITLE=21&PART=50&SECTION=25&YEAR=2000 &TYPE=TEXT. Resources (continued) Magnus, P.D., Kalichman, M. (September 2002). Protection of Human Subjects. Retrieved September 11, 2005, from RCR Educational Resources, Online Resource for RCR Instructors: http://www.rcrec.org/r/index.php?module=ContentExpress&f unc=display&meid=74&ceid=33. National Institutes of Health. (2000). Available from http://cme.cancer.gov/c01/nih_reg.htm (Course Registration). United States Holocaust Memorial Museum (n.d.) The doctors trial: The medical case of the subsequent Nuremberg proceedings.Retrieved September 11, 2005, from http://www.ushmm.org/research/doctors/ This completes the presentation on Protection of Human Subjects THANK YOU!