Butterfly Creek - Talk by Dr Paul Hofman
advertisement

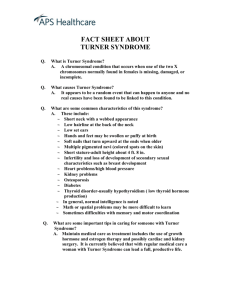
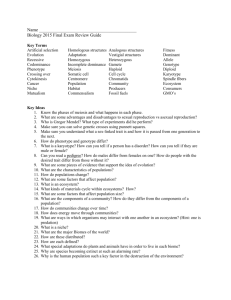
Paul Hofman 2007 Karyotype versus Phenotype in Turner Syndrome Karyotype = chromosomal structure Phenotype = Physical characteristics – ‘how the person looks’ maternal paternal q centromere p Most TS features occur when this area is missing X Inactivation q centromere p maternal paternal 45XO q Paternal/ Maternal centromere p Karyotype versus Phenotype in Turner Syndrome There is some correlations but karyotypes are not predictive of what any particular girl with TS will have 45XO most common and severest phenotype (highest incidence of cardiac, renal abnormalities and other dysmorphic features) Karyotype versus Phenotype in Turner Syndrome 45XO/46XX Some cells have normal XX and some have XO (often called a mosaic pattern as two distinct cell lines). The frequency of each cell line can vary from tissue to tissue- this can change the phenotype. Generally the least severe phenotype. Increased mean height and spontaneous puberty in up to 40%. maternal paternal q Iso q centromere q Karyotype versus Phenotype in Turner Syndrome 46Xi(Xq) Increased risk of autoimmunity esp thyroid and inflammatory bowel disease and deafness. Structural problems uncommon. Ring Chromosome (r)ing centromere Karyotype versus Phenotype in Turner Syndrome 46Xr(X) Ring Chromosome – often small and can be a mosaic pattern (ie not in all cells) Spontaneous periods in 33%. Congenital abns uncommon. Intellectual dysfunction in those with a small ring chromosome. Karyotype versus Phenotype in Turner Syndrome 45X/46XY Have male karyotype in some cells (46XY). Often taller and there is an increased risk of gonadal tumour. Imprinting – what is it and what does it mean for Turner Syndrome? We all possess two alleles for each gene product – one from our mother and one from our father. In most genes the end result is the combination of these two alleles (eg handedness). In some genes, especially those related to growth one allele is permanently turned off. This occurs at or soon after fertilisation and is called imprinting. ‘X Inactivation’ Imprinting also occurs on the X chromosome. One half of the X chromosomes are randomly inactivated (ie roughly half maternal and half paternal) However in 45XO there is only one chromosome this is usually maternal (~70%) but can be paternal (~30%) in origin. Does inheriting only one parents chromosome change the phenotype seen in TS? Parent of Origin Effects Personality/ learning – One British study Maternal X - poorer verbal skills - poorer sociobehavioural skills Not substantiated in several subsequent studies. Nature; 37:705-08, 1997 Parent of Origin Effects Growth – Several studies shown effects on growth Maternal X - maternal and midparental height - greater height gain with growth hormone Paternal X - weakly associated with parents height. - poorer final height. JCEM 91: 3002-10, 2006 Genetics and Molecular Research 6(1):1-7, 2007 Parent of Origin Effects Hearing Loss – one recent study Paternal X - Strongly associated with an increased risk of hearing impairment. Of 50 subjects, 23 (46% had sensorineural hearing loss (SNHL)). 12 of 18 with Xpat (67%) had SNHL versus 11 of 32 Xmat (34%). JCEM 91: 3002-10, 2006 Parent of Origin Effects Kidneys and eyes Maternal X - all renal abnormalities occurred in this group Paternal X - ocular problems more common JCEM 92: 846-852, 2007 Parent of Origin Effects Metabolism – two recent studies Maternal X - Increased total abdominal and visceral fat accumulation. - more atherogenic lipid profile. JAMA March 22/29 (12); 295, 1373-74, 2006 JCEM 92: 846-852, 2007 Body Composition Altered in adult TS (42.5 ± 9.7 years) showing: Increased fat mass including increased visceral fat. Reduced muscle mass. Reduced exercise capacity. n=55 n=54 European J of Endocrinology, 155: 583-92. 2006 Body Composition Effect of growth hormone Increased lean and bone mass Reduced fat mass Effects independent of oestrogen and still apparent > one year after finishing growth hormone. JCEM 91: 4302-05, 2006 n=28 12.8 yrs n=39 11.9 yrs Body Composition Effect of oestrogen replacement IM or transdermal oestrogen may result in reduced fat mass accumulation. Spray on gel (17b oestradiol) used in young lean adult TS women (n=9, 23 years) for 1 year. Total lean mass increased by 1kg compared to oral HRT group with no significant change in fat mass between groups. The route of administration may be more important than previously considered – watch this space. Gynecological Endocrinology, 22(10): 590-94, 2006 Oestrogen route and growth Oestrogen route of administration may affect puberty growth spurt. A small study examined giving IM oestradiol to 7 TS at either 12-12.9 years or 14-14.9 years. Predicted height in both groups was 150.8 cm. All received growth hormone. Final height was 154 cm in the early pubertal induction group and 152.9 cm in the late pubertal induction group JCEM, 90:6424-30. 2005 Oestrogen route and growth This equates to a pubertal height gain of 17.3 cm in the early oestrogen group 15.0 cm in the late pubertal group 11.4 cm after oral oestrogen therapy at 12 years age. Oral oestrogens have major effects on the liver which maty reduce pubertal growth. Transdermal oestrogen now available here – Watch this space! JCEM, 90:6424-30. 2005 Cognition and Turner Syndrome ‘Non verbal disability’ Characterised by - deficits in maths and science - Impaired performance in visuo-motor tasks that have a spatial component. - impaired adaptation to novel situations - impaired social competence - increased anxiety and depression - Increased ADHD (18 fold increase in TS) Hormone Research, 65: 47-56. 2006. J Ped. Psychology31(9): 945-55, 2006 Cognition and Turner Syndrome Therapeutic recommendations (by Harnadek and Rourke) J Learning Disability, 27:144-54. 1994. Cognition and Turner Syndrome a) Sex Steroid Effects on the Brain b) Lack of an X chromosome/ genes involved in neurocognitive development and behaviour c) Imprinting (? real) d) Environmental interactions Hormone Research, 65: 47-56. 2006 Sex Steroid Effects Oestrogen Improves adult women’s verbal memory, articulatory speed and fine motor abilities. Oestrogen supplementation to young TS girls has improved verbal memory. Doesn’t improve spatial deficits. Hormone Research, 65: 47-56. 2006 Sex Steroid Effects Androgen TS women are also androgen deficient. Higher testosterone levels in men and women associated with better spatial ability, mathematics and problem solving. Women tx with androgens after ovariectomy have improved memory, complex information processing and logical reasoning. Oxandrolone tx of TS girls improved working memory after 2 years of tx Hormone Research, 65: 47-56. 2006 Haploinsufficiency (one chromosome) Most of the genes involved in neurocognitive and behaviour involve areas of the X chromosome that don’t get inactivated and there are usually two copies of the gene available. Therefore in TS there is a reduction in the gene dose and possible developmental; consequences as a result. Hormone Research, 65: 47-56. 2006 Environment Shyness, social anxiety and impaired self esteem reduced equally in adults with TS (n=100, age 34.7 years) and women with premature ovarian failure (n=100, 30.9 years) and healthy controls (n=35, 35.8 years). Hormone Research, 65: 47-56. 2006 Self reported psychosocial function and body image perception 30 TS women (age 22.1 years) matched to 44 non TS women (20.5 years). No difference on most scores including all behavioural and emotional problems. They perceived themselves as socially less competent. BMI was related to the appraisal score. Hormone Research, 66: 277: 277-84. 2006 Self perception profile Hormone Research, 66: 277: 277-84. 2006 Self-Esteem and social adjustment – influence of pubertal management and sexuality French! 566 young adult TS women (18.3-31.2 years) Low self esteem associated with - hearing impairment - limited sexual experience JCEM 91:2972-79, 2006 Self-Esteem and Social Adjustment – influence of pubertal management and sexuality Low social adjustment associated with lower socio economic class and an absence of sexual experience Age at pubertal development associated with age at first sexual experience. Delayed pubertal induction had a long lasting effect on sex life. JCEM 91:2972-79, 2006 Turner Syndrome – Incidence, diagnostic delay and mortality Danish Cytogenetic register – 781 TS between 1970-2001. Incidence: 50/100,000 (1:2000 female births) a) There was a delay in diagnosis with the mean age being 15.1 years! Although this is historical many patients still seem to be missed until their 20s. b) There is a decreasing age at diagnosis over the 30 years study period. JCEM 91:3897-02, 2006 JCEM 91:3897-02, 2006 Turner Syndrome – mortality Overall mortality was increased compared to the general population (standardised mortality rate (SMR) 2.86 ~ almost 3 times the risk of dying) There was a karyotype risk with XO SMR=4.08 isoXq SMR= 3.86 other karyotypes SMR = 2.1 JCEM 91:3897-02, 2006 Turner Syndrome – mortality Commonest causes of death Congenital abnormalities (probably mainly cardiac) Coronary artery disease Metabolic/ endocrine (eg inadequate HRT) DIABETES MELLITUS was a contributing cause of death in 22% of cases. JCEM 91:3897-02, 2006 Thank You