Ethnic differences in mortality
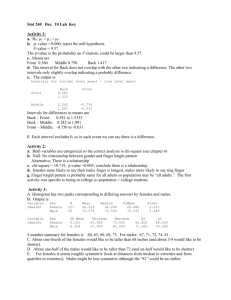
advertisement

Ethnic Differentials in Mortality Based on the Study of Ethnic Differentials in Adult Mortality in Central Asia Michel Guillot (PI), University of Wisconsin-Madison Natalia Gavrilova, University of Chicago Tetyana Pudrovska, University of Wisconsin-Madison Background on Kyrgyzstan Former Soviet republic; became independent in 1991 Population: 5.2 million (2006) Experienced a severe economic depression after break-up of Soviet Union GNI per capita = 440 USD; 28th poorest country in the world (2005) 48% of population below national poverty line (2001) Ethnic Groups in Kyrgyzstan Native Central Asian groups: Kazakh, Kyrgyz, Tajik, Turkmen, Uzbek (Sunni Muslims) Slavs: Russian, Ukrainian, Bielorussian Kyrgyzstan, 1999 census: Central Asians: 79% of pop. (Kyrgyz 65%) Slavs: 14% of pop. (Russian 12%) Recorded trends in adult mortality (20-60 years) Kyrgyzstan, 40q20 0.30 0.10 0.20 q2060 0.10 0.20 q2060 0.30 0.40 Females 0.40 Males 1960 1970 1980 y ear 1990 2000 1960 1970 1980 y ear 1990 2000 russian ky rgy z russian ky rgy z slv cas slv cas Mortality paradox? Soviet period: Russians/Slavs occupied dominant positions in the socio-economic structure of Central Asian societies (Kahn 1993) Mortality paradox? Slavic females more educated than Central Asian females (1989 and 1999 censuses) Slavic males: educational advantage not so clear – varies by age (1989 and 1999 censuses) Slavic households less poor than Central Asians (1993 World Bank poverty survey) Infant mortality lower among Slavs (Soviet and post-Soviet period) Proportion of individuals with post-secondary education, by age and ethnicity, in 1989 census. Females SLAVIC (Russian, Ukrainian, Belorussian), 1989 CENTRAL ASIAN (Kyrgyz, Uzbek), 1989 0.300 Proportion higher education 0.250 0.200 0.150 0.100 0.050 0.000 20-24 25-29 30-34 35-39 40-44 45-49 50-54 55-59 60-64 Mortality paradox? Slavic females more educated than Central Asian females (1989 and 1999 censuses) Slavic males: educational advantage not so clear – varies by age (1989 and 1999 censuses) Slavic households less poor than Central Asians (1993 World Bank poverty survey) Infant mortality lower among Slavs (Soviet and post-Soviet period) Proportion of individuals with post-secondary education, by age and ethnicity, in 1989 census. Males. SLAVIC (Russian, Ukrainian, Belorussian), 1989 CENTRAL ASIAN (Kyrgyz, Uzbek), 1989 0.250 Proportion higher education 0.200 0.150 0.100 0.050 0.000 20-24 25-29 30-34 35-39 40-44 45-49 50-54 55-59 60-64 Mortality paradox? Slavic females more educated than Central Asian females (1989 and 1999 censuses) Slavic males: educational advantage not so clear – varies by age (1989 and 1999 censuses) Slavic households less poor than Central Asians (1993 World Bank poverty survey) Infant mortality lower among Slavs (Soviet and post-Soviet period) Mortality paradox? Slavic females more educated than Central Asian females (1989 and 1999 censuses) Slavic males: educational advantage not so clear – varies by age (1989 and 1999 censuses) Slavic households less poor than Central Asians (1993 World Bank poverty survey) Infant mortality lower among Slavs (Soviet and post-Soviet period) IMR by ethnicity, 1958-2003, Kyrgyzstan 30 20 10 IMR 40 50 Urban areas 1960 1970 1980 year Central Asians 1990 Slavs 2000 Data Unpublished population and death tabulations since 1959 collected from local archives Individual census records – 1999 Individual death records – 19981999 obtained from national statistical office Possible explanations for mortality paradox Data artifacts Migration effects (esp. 1989-99) Cultural effects Data artifacts? Could the lower recorded mortality among Central Asian adults be due to lower data quality among them (coverage of deaths, age misreporting)? Cultural effects? Culture may affect mortality in various ways: individual health and lifestyle behaviors (e.g., diet, smoking, alcohol, use of preventive care) family structure and social networks (denser social networks may produce lower stress levels and better health) Could different cultural practices among Slavs and Central Asians explain the observed mortality differentials? Data artifacts? Intercensal estimates of death registration coverage above age 60 (Guillot, 2004): 90+ % as early as 1959 in urban areas coverage in rural areas was low initially (~50%) but caught up with urban areas in 1980s Total population: 92% for 1989-99 period Adult deaths (20-59) usually better reported than deaths 60+ Kyrgyzstan, 40q20, Urban areas 0.30 0.20 0.10 0.10 0.20 q2060 0.30 0.40 Females 0.40 Males 1960 1970 1980 y ear 1990 2000 1960 1970 1980 y ear 1990 2000 russian ky rgy z russian ky rgy z slv cas slv cas Migration effects? 1/3 of Russian population has left Kyrgyzstan since 1991 Could the increased disparity between Russian and Kyrgyz adult mortality be due to selective migration (healthy migrant effect)? Health selection? Russians in KG vs. Russia, 40q20 0.40 0.50 Females 0.10 0.20 0.30 q2060 0.30 0.20 0.10 q2060 0.40 0.50 Males 1960 1970 1980 y ear Russians in KG 1990 2000 Russia 1960 1970 1980 y ear Russians in KG 1990 2000 Russia Cohort-specific changes in educational attainment, Males, 1989-99 SLAVIC, 1989 SLAVIC, 1999 0.300 Proportion higher education 0.250 0.200 0.150 0.100 0.050 0.000 Age in 1989: 20-24 Age in 1999: 30-34 25-29 35-39 30-34 40-44 35-39 45-49 40-44 50-54 45-49 55-59 50-54 60-64 55-59 65-69 60-64 70-74 65-69 75-79 70-74 80-84 75-79 85-89 80-84 90-94 Cohort-specific changes in educational attainment, Females, 1989-99 SLAVIC, 1989 SLAVIC, 1999 0.300 Proportion higher education 0.250 0.200 0.150 0.100 0.050 0.000 Age in 1989: Age in 1999: 20-24 30-34 25-29 35-39 30-34 40-44 35-39 45-49 40-44 50-54 45-49 55-59 50-54 60-64 55-59 65-69 60-64 70-74 65-69 75-79 70-74 80-84 75-79 85-89 80-84 90-94 Cultural effects? Analysis of causes of death by ethnicity, 1998-99 Calculations based on micro-data Deaths: vital registration (1998-99) Exposure: census (March 1999) Ages 20-59 Ethnicity: Central Asians vs. Slavs ~20,000 death records; ~2.2 million census records Age-standardized Death Rates at working ages (per 100000), 1998-99, by cause and ethnicity, Males Infectious/par. diseases - incl. TB Neoplasms CVD CA Slavs - incl. IHD Respiratory diseases Digestive diseases Injuries/poisoning Other causes 0 50 100 150 200 250 Contribution of causes of death to the difference in life expectancy at working ages (40e20) between Slavs and Central Asians Males (total difference = 2.90 years) 1.8 1.6 1.4 1.2 1.0 0.8 0.6 0.4 0.2 au se s O th e rc ju ri es In C V R D es pi ra to ry D is . D ig es t iv e D is . pl as m s N eo In fe ct io ns 0.0 ho m un de te rm in ed su ic id e . ic id ac e cid .p oi al so lo ni ng th er ac ci d. tra ca ns us po . rt ac ci ac de ci nt de s nt al dr ow ac c. ni ca ng us ./e ac le ct c. r.c m ec ur ha n. su ffo ca t. ot he r in ju ry ac ci d. po is on ./a lco h Age-standardized Death Rates at working ages (per 100,000). Detailed Injuries, Males 50 45 40 Slavs CA 35 30 25 20 15 10 5 0 Age-standardized Death Rates at working ages (per 100,000), 1998-99, by cause and ethnicity, Females Infectious/par. diseases - incl. TB Neoplasms CVD - incl. IHD Respiratory diseases Digestive diseases CA Slavs Injuries/poisoning Other causes 0 10 20 30 40 50 60 70 80 Contribution of causes of death to the difference in life expectancy at working ages (40e20) between Slavs and Central Asians Females (total difference = .28 years) 0.35 0.30 0.25 0.20 0.15 0.10 0.05 au se s O th e rc ju rie s In Di s. e es t iv CV D pl as m s Di s. Di g -0.10 Re sp ir a to ry In -0.05 Ne o fe ct io ns 0.00 . su ic id e .a cc id en t.c tra au ns s. po rt ac ci ac de ci nt d. s ca us e ac by c. fir ca e us ./e le ac ct ci r.c de ur nt al dr ow ni ng al lo o. ic id ac e ci d. po iso in ju ni ry ng un de te rm in ed ho m ac ci d. po is on ./a lco h Age-standardized Death Rates at working ages (per 100,000) Detailed Injuries, Females 9 8 7 Slavs CA 6 5 4 3 2 1 0 Alcohol-related Causes of Death (Chronic alcoholism, Alcohol psychoses, Alcohol cirrhosis of the liver, Accidental poisoning by alcohol) Age-standardized Death Rates at working ages (per 100,000) 50 45 CA Slavs 40 35 30 25 20 15 10 5 0 Males Females Multivariate analysis Do ethnic mortality differentials at adult ages remain once we account for differences in education and urban/rural residence? Negative binomial regression Dependent variable: deaths from all causes; deaths by major cause (7) Explanatory variables: exposure, dummy variables for age, ethnicity, urban/rural residence, education (3 cat.) Males and Females analyzed separately Model 1: age, ethnicity Model 2: age, ethnicity, education, residence Males, all causes of death In e s. ie s di s. di ju r es t iv Di g y Re sp ir a to r CV D pl as m s ns ca us es fe ct io Ne o In Al l Risk Ratio Slavs/CA Males 3.5 3.0 2.5 2.0 Model 1 1.5 Model 2 1.0 0.5 0.0 Risk Ratio Slavs/CA Females 3.5 3.0 2.5 2.0 Model 1 Model 2 1.5 NS NS 1.0 NS NS NS NS NS NS 0.5 au se s ie s O th e rc ju r In CV Re D sp ir a to ry Di s. Di ge st iv e Di s. pl as m s Ne o ns fe ct io In Al l C au se s 0.0 Conclusions Excess mortality among adult Slavs (Soviet and post-Soviet period) is not likely due to data artifacts or migration effects Excess mortality due to important ethnic differences in cause-specific mortality – alcohol and suicide in particular Differences remain unexplained by education or residence Conclusions Role of cultural characteristics? Alcohol tied to cultural practices (“culture of alcohol” among Russians; Impact of Islam for Central Asians) Denser social networks and stronger social support among Central Asian ethnic groups? Обследования населения, биомаркеры и продолжительность здоровой жизни Н.С. Гаврилова Population surveys Provide more detailed information on specific topics compared to censuses Cover relatively small proportion of population (usually several thousand) Population-based survey – random sample of the total population; represents existing groups of population International Surveys in Russia and FSU Russia Longitudinal Monitoring Survey (RLMS) http://www.cpc.unc.edu/rlms/ Demographic and Health Surveys (DHS) are nationally-representative household surveys that provide data for a wide range of monitoring and impact evaluation indicators in the areas of population, health, and nutrition. http://www.measuredhs.com http://www.cpc.unc.edu/projects/rlms 16 раундов обследования Demographic and Health Surveys Child Health - vaccinations, childhood illness Education - highest level achieved, school enrollment Family Planning knowledge and use of family planning, attitudes Female Genital Cutting - prevalence of and attitudes about female genital cutting Fertility and Fertility Preferences - total fertility rate, desired family size, marriage and sexual activity Gender/Domestic Violence - history of domestic violence, frequency and consequences of violence HIV/AIDS Knowledge, Attitudes, and Behavior - knowledge of HIV prevention, misconceptions, stigma, higher-risk sexual behavior HIV Prevalence - Prevalence of HIV by demographic and behavioral characteristics Household and Respondent Characteristics- electricity, access to water, possessions, education and school attendance, employment Infant and Child Mortality - infant and child mortality rates Malaria - knowledge about malaria transmission, use of bednets among children and women, frequency and treatment of fever Maternal Health - access to antenatal, delivery and postnatal care Maternal Mortality - maternal mortality ratio Nutrition - breastfeeding, vitamin supplementation, anthropometry, anemia Wealth/Socioeconomics - division of households into 5 wealth quintiles to show relationship between wealth, population and health indicators Women's Empowerment - gender attitudes, women’s decision making power, education and employment of men vs. women DHS sample designs The sample is generally representative: At the national level At the residence level (urban-rural) At the regional level (departments, states) The sample is usually based on a stratified two-stage cluster design: First stage: Enumeration Areas (EA) are generally drawn from Census files Second stage: in each EA selected, a sample of households is drawn from an updated list of households DHS охватывает следующие страны б.СССР Азербайджан Казахстан (1995, 1999) Кыргызстан (1997) Молдова (2005) Туркменистан (2000) Узбекистан (1995, 2002) Biomarkers in Population-Based Aging and Longevity Research Natalia Gavrilova, Ph.D. Stacy Tessler Lindau, MD, MAPP CCBAR Supported by the National Institutes of Health (P30 AG012857) NSHAP Supported by the National Institutes of Health (5R01AG021487) including: National Institute on Aging Office of Research on Women's Health Office of AIDS Research Office of Behavioral and Social Sciences Research Goals: Foster interdisciplinary research community Establish means of exchanging rapidly evolving ideas related to biomarker collection in population-based health research Translation to clinical, remote, understudied areas Why? Need for move from interdisciplinary data COLLECTION to integrated data ANALYSIS Barriers Models/methods Rules of academe Reviewers/editors Why? Growing emphasis on value of interdisciplinary health research NIH Roadmap Initiative NAS report Overcome barriers of unidisciplinary health research Concern for health disparities Response bias in clinical setting Self-report in social science research What is needed? Methods and models for analytic integration Streamlining data collection Advances in instruments Minimally invasive techniques Best practices Concern for ethical issues Central coordination? Introduction to: Public Dataset http://www.icpsr.umich.edu/NACDA/ NSHAP Collaborators Co-Investigators Linda Waite, PI Ed Laumann Wendy Levinson Martha McClintock Stacy Tessler Lindau Colm O’Muircheartaigh Phil Schumm NORC Team Stephen Smith and many others Collaborators David Friedman Thomas Hummel Jeanne Jordan Johan Lundstrom Thomas McDade Ethics Consultant John Lantos Outstanding Research Associates and Staff Affiliated Investigators and Labs LAB SPECIMENS ASHA Test results Lundstrom, Sweden Olfaction Hummel, Germany Gustation Magee Women’s Hospital, Jeanne Jordon Vaginal Swabs, TM Orasure McClintock Lab, Univ. Chicago Vaginal Cytology McDade Lab, Northwestern Univ. Blood Spots Salimetrics Saliva USDTL* Urine Corporate Contributions and Grants Item Company/Contact Information Smell pens Martha McClintock, Institute for Mind and Biology at the University of Chicago OraSure collection device Orasure Technologies Digital scales Sunbeam Corporation Blood pressure monitors A & D Lifesource Vision charts David Freidman, Wilmer Eye Institute at the Johns Hopkins Bloomberg School of Public Health Filter paper for blood spot collection Schleicher & Schuell Bioscience Blood pressure cuff (large size) A & D Lifesource OraSure Western Blot Kit Biomerieux Company HPV kits Digene Laboratory Boxes of swabs Digene Laboratory 2-point discriminators Richard Williams Study Timeline Funding: NIH / October, 2003 Pretest: September – December, 2004 Wave I Field Period: June 2005 – March 2006 Wave I Analysis: Began October, 2006 He, W., Sengupta, M., Velkoff, V. A., DeBarros, K. A. (2005). 65+ In the United States: 2005. Current Population Reports: Special Studies, U. S. Census Bureau. NSHAP Design Overview Interview 3,005 community-residing adults ages 57-85 Population-based sample, minority over-sampling 75.5% weighted response rate 120-minute in-home interview Questionnaire Biomarker collection Leave-behind questionnaire Est. Pop. Distributions (%) AGE 57-64 65-74 75-85 RACE/ETHNICITY White African-American Latino Other RELATIONSHIP STATUS Married Other intimate relationship No relationship SELF-RATED HEALTH Poor/Fair Good Very good/Excellent Men (n=1455) Women (n=1550) 43.6 35.0 21.4 39.2 34.8 26.0 80.6 9.2 7.0 3.2 80.3 10.7 6.7 2.2 77.9 7.4 14.7 55.5 5.5 39.0 25.5 27.5 47.0 24.2 31.5 44.3 Domains of Inquiry Demographics Basic Background Information Marriage Employment and Finances Religion Social Networks Social Support Activities, Engagement Intimate relationships, sexual partnerships Physical Contact Medical Physical Health Medications, vitamins, nutritional supplements Mental Health Caregiving HIV Women’s Health Ob/gyn history, care Hysterectomy, oophorectomy Vaginitis, STDs Incontinence NSHAP Biomeasures Blood: hgb, HgbA1c, CRP, EBV Saliva: estradiol, testosterone, progesterone, DHEA, cotinine Vaginal Swabs: BV, yeast, HPV, cytology Anthropometrics: ht, wt, waist Physiological: BP, HR and regularity Sensory: olfaction, taste, vision, touch Physical: gait, balance NSHAP Biomeasures Cooperation Measure Height Weight Blood pressure Touch Smell Waist circumference Distance vision Taste Get up and go Saliva Oral fluid for HIV test Blood spots Vaginal swabs Eligible Respondents 2,977 2,977 3,004 1,502 3,004 3,004 1,505 3,004 1,485 3,004 972 2,493 1,550 Cooperating Respondents 2,930 2,927 2,950 1,474 2,943 2,916 1,441 2,867 1,377 2,721 865 2,105 1,028 * Person-level weights are adjusted for non-response by age and urbanicity. Cooperation Rate* 98.6% 98.4% 98.4% 98.4% 98.3% 97.2% 96.0% 95.9% 93.6% 90.8% 89.2% 85.0% 67.6% Principles of Minimal Invasiveness Compelling rationale: high value to individual health, population health or scientific discovery In-home collection is feasible Cognitively simple Can be self-administered or implemented by single data collector during a single visit Affordable Low risk to participant and data collector Low physical and psychological burden Minimal interference with participant’s daily routine Logistically simple process for transport from home to laboratory Validity with acceptable reliability, precision and accuracy Lindau ST and McDade TW. 2006. Minimally-Invasive and Innovative Methods for Biomeasure Collection in Population-Based Research. National Academies and Committee on Population Workshop. Under Review. Applying Biomeasures in NSHAP Uses of Biomeasures Population-Based Sample Clinic-Based Sample ++ ++ - ++ -- ++ To determine effectiveness of intervention ++ + To identify biological correlates or mechanisms of social/environmental conditions ++ -- To detect and monitor risk for disease, pre-disease, disease, mortality OR to quantify and monitor function To recruit or exclude people from study To determine efficacy of intervention ++ = Very well suited -- = Poorly suited NSHAP Biomeasures “Laboratory Without Walls” McClintock Laboratory (Cytology) UC Cytopathology (Cytology) Jordan Clinical Lab Magee Women’s Hospital (Bacterial, HPV Analysis) Salimetrics (Saliva Analysis) McDade Lab Northwestern (Blood Spot Analysis) Salivary Biomeasures Sex hormone assays Estradiol Progesterone DHEA Testosterone Cotinine Frequency Frequency Frequency Salivary Sex Hormones (preliminary analysis) log(estradiol) Units: pg/ml log(progesterone) log(testosterone) Salivary Cotinine Nicotine metabolite Objective marker of tobacco exposure, including second-hand Non-invasive collection method (vs. serum cotinine) Distribution of Salivary Cotinine Classification of Smoking Status by Cotinine Level in Females Cut-points based on distribution among smokers .2 Occasional Fraction .15 Nonsmoker Passive Regular .1 10 ng 15 ng 34 ng 10% M 103 ng 30% M 344 ng M .05 0 -5 0 log(Cotinine) M = mean cotinine among female who report current smoking Bar on left corresponds to cotinine below level of detection 5 10 Dried Blood Spots C-Reactive Protein (CRP) Epstein-Barr Virus (EBV) Antibody Titers Thanks, Thom and McDade Lab Staff! Self-Report Measures Demographic Variables: Age Race/Ethnicity Education Insurance Status Self-Report Measures Social/Sexuality Variables: Spousal/other intimate partner status Cohabitation Lifetime sex partners Sex partners in last 12 months Frequency of sex in last 12 months Frequency of vaginal intercourse Condom use Self-Report Measures Health Measures: Obstetric/Gynecologic history Number of pregnancies Duration since last menstrual period Hysterectomy Physical health Overall health Co-morbidities Health behaviors Tobacco use Pap smear, pelvic exam history Cancer Challenges Specimen Storage First enrollment July, 2005 Last enrollment March 2006 Specimens collected and sent to lab When does a study end? Initial storage (pre-assay) Interim storage (post-assay) Continued storage (post-assay) Destruction? Storage for future use? More Information on Biomarkers is Available at the CCBAR website http://biomarkers.uchicago.edu/ Measures of Population Health Living longer but healthier? Keeping the sick and frail alive Delaying onset and progression expansion of morbidity (Kramer, 1980). compression of morbidity (Fries, 1980, 1989). Somewhere in between: more disability but less severe dynamic equilibrium (Manton, 1982). WHO model of health transition (1984) Quality or quantity of life? Health expectancy partitions years of life at a particular age into years healthy and unhealthy adds information on quality is used to: monitor population health over time compare countries (EU Healthy Life Years) compare regions within countries compare different social groups within a population (education, social class) What is the best measure? Health Expectancy Healthy LE (self rated health) HLE Disability free LE DFLE Disease free LE DemFLE Cog imp-free LE Active LE (ADL) Many measures of health = many health expectancies! What is the best measure? Depends on the question Need a range of severity Performance versus self-report dynamic equilibrium cultural differences Cross-national comparability translation issues Estimation of health expectancy by Sullivan’s method Life expectancy expectancy and expected lifetime with and without long-standig illness 1.0 Survival probability probability 0.9 Years with longstanding illness 0.8 0.7 0.6 0.5 0.4 Years without Life expectancy long-standing illness 0.3 0.2 0.1 0.0 0 10 20 30 40 50 60 Age 70 80 90 100 110 Health expectancy by Sullivan's method 1,0 Survival probability 0,9 Life table data 0,8 0,7 0,6 Prevalence data on health status 0,5 0,4 Unhealthy 0,3 Healthy 0,2 0,1 0,0 0 10 20 30 40 50 60 Age 70 80 90 100 110 Calculation of health expectancy (Sullivan method) Lxh = Lx x πx Where πx - prevalence of healthy individuals at age x Lxh - person-years of life in healthy state in age interval (x,x+1) Вероятность быть здоровым в зависимости от возраста Мужчины Andreyev et al., Bull.WHO, 2003 Вероятность быть здоровым в зависимости от возраста Женщины Andreyev et al., Bull.WHO, 2003 Choice of health expectancy indicators Self-rated health Interview question: “How do you rate your present state of health in general?” Answer categories: Very good Good Fair Poor Very poor } } Dichotomised Long-standing illness Interview question: “Do you suffer from any long-standing illness, longstanding after-effect of injury, any handicap, or other long-standing condition?” Long-lasting restrictions (if “yes” to the following questions) First question: “Within the past 2 weeks, has illness, injury or ailment made it difficult or impossible for you to carry out your usual activities?” Second question: “Have these difficulties/restrictions been of a more chronic nature? By chronic is meant that the difficulties/restrictions have lasted or are expected to last 6 months or more”