CODING and BILLING Am I Being Paid Appropriately?
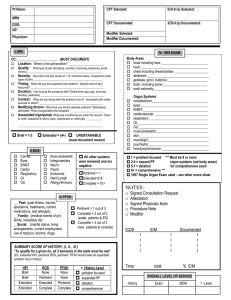
advertisement
Sandra M. Nettina, MSN, CRNP President, NPAM Nurse Practitioner, Columbia Medical Practice CODING ICD-9 International Classification of Diseases Published by United States Government Diagnoses based Assign codes to your assessment at the highest level of differentiation CPT Current Procedural Terminology Copyrighted by American Medical Association Procedural rather than disease or disorder Coding (cont.) ICD-9 codes are used to justify medical necessity of a service CPT codes are used for billing Evaluation and management codes (E&M) are CPT codes that describe consultations, ER, and office visits Evaluation and Management Codes new and established office visit 99201/99211: 10 min. (new) or 5 min. (est.) Presenting problem is self limiting or minor 99202/99212: 20 min. (new) or 10 min. (est.) low to moderate severity 99203/99213: 30 min. (new) or 15 min. (est.) moderate severity 99204/99214: 45 min. (new) or 25 min. (est). moderate to high severity 99205/00215: 60 min. (new) or 40 min. (est.) moderate to high severity Other Encounters Outpatient consultation: 99241 to 99245 Inpatient consultation: 99251 to 99255 Emergency Room: 99281 to 99285 Initial hospital observation: 99221 to 99223 Subsequent hospital: 99231 to 99233 Initial nursing facility: 99304 to 99306 Subsequent nursing facility: 99307 to 99310 Domiciliary, Rest home, custodial care Billing Use E&M codes for Outpatient Visits, Consultations (outpatient and inpatient), ER visits Calculated by 7 components Similar process for hospital observation, nursing facility, and home care, but will not be discussed Components determine E&M coding level—must be documented Key History Exam Medical Decision Making (MDM) Contributing Counseling Coordination Nature of Presenting Problem Time HISTORY Chief Complaint—required for all level of visits History of Present Illness (HPI)—brief or extended Review of Systems (ROS)—problem focused, extended, complete Past, Family, Social History (PFSH)—pertinent or complete How much information is obtained and documented? CC and HPI Chief complaint is required for all level of histories: simple statement HPI elements: OLFQQAAT, OLDCART, PQRST Onset, location, frequency, duration, quality (character), quantity (severity), aggravating factors, relieving factors (treatments tried), associated factors REVIEW of Systems Constitutional Neurologic Eyes Psychiatric Ears, nose, throat Endocrine Cardiac/vascular Heme/lymph Respiratory Allergy/immunology GI GU Musculoskeletal Intgumentary/breast Past Medical, Family, and Social History Past illnesses, chronic conditions, surgeries, injuries, hospitalizations, health screening and diagnostic tests Medications Related family history Social history—tobacco, alcohol, drugs, exercise, diet, work, sexual activity Level of History Type of History CC HPI ROS PFSH Problem Focused Required Brief (1-3 elements) Not required Not required Expanded problem focused Required Brief (1-3 elements) Problem pertinent Not required Detailed Required Extended (4+ elements, or status of 3+ chronic conditions) Extended (2-9 systems) Pertinent (1 item from 1 area) Extended Complete (10+ systems) Complete (1 item from 2 areas (est.) or 3 areas (new)) Comprehensiv Required e Level of History (cont.) Complete ROS—10 or more systems or some systems with statement “all other systems negative” Complete PFSH—need 3 for new patients, consultations, hospital observation, initial nursing facility care Determine the level of history by the column farthest to the left (one poorly documented element can bring the level down). EXAM Body Area Head/face, Back/spine, Chest/breast/axilla, Genitalia/groin/buttocks, Abdomen, Neck, Each Extremity Organ Systems Constitutional, Eyes, Ears/nose/throat, Cardiovascular, Respiratory, GI, GU, Musculoskeletal, Skin, Neuro, Psych, Heme/lymph/immune EXAM Problem focused Expanded Detailed problem Comprehensive Single Organ System 1-5 elements At least 6 elements At least 12 (eye and psych: 9) All elements Multi-system Exam 1-5 elements in 1 or more systems At least 6 elements in 1 or more systems At least 6 systems with 2 elements each At least 9 systems with 2 elements each Medical Decision Making Number of diagnoses and treatment options Amount and complexity of data reviewed Risk of complications Morbidity and mortality Number of Diagnoses and Treatment Options Problem Status Points Self limited or minor 1 Established problem (to examiner): stable or improved 1 Established problem (to examiner): worsening 2 New problem (to examiner): no additional work up 3 New problem (to examiner): additional work up planned 4 Add up the scores for all problems to obtain a total. Self limited or minor maximum of 2. New problem with no additional work up maximum of 1. Amount and Complexity of Data Reviewed Reviewed Data Points Review and/or order of clinical lab tests 1 Review and/or order of radiology 1 Review and/or order of other medical tests 1 Discussion of test results with performing physician 1 Decision to obtain old records or history from someone other than patient 1 Review and summarize old records and/or obtain history from someone else and/or discuss case with another health care provider 2 Independent review of imaging, tracing, or specimen itself 2 Total Risk of Complications, Morbidity/Mortality Minimal—one self-limited or minor problem Low—2 or more self-limited or minor problems; 1 stable chronic illness; 1 acute, uncomplicated illness Moderate—1 or more chronic illness with minor exacerbation; 2 or more stable chronic illnesses; undiagnosed new problem with uncertain prognosis; acute illness with systemic symptoms; acute complicated injury Risk (continued) High 1 or more chronic illnesses with severe exacerbation Acute or chronic illnesses or injuries that may pose a threat to life or bodily function An abrupt change in neurologic status Minimal Risk examples Cold, insect bite, tinea corporis Order blood work, chest xray, ECG Recommend rest, gargles, superficial dressing Low Risk Examples 2 or more self limited or minor problems 1 chronic illness that is well controlled Acute illness such as UTI, simple sprain, allergic rhinitis PFT, skin biopsy, non-cardiac imaging OTC meds, physical therapy, minor surgery without risk factors, IV fluid without additives Moderate Risk examples One or more chronic condition, worsening Two or more stable chronic conditions Acute illness with systemic symptoms such as pylonephritis, pneumonia Acute complicated injury such as concussion New problem needing additional work up Stress test, endoscopy, cardiovascular imaging Minor surgery with risk factors, prescription drugs, closed treatment of fracture High Risk examples One or more chronic illness with severe exacerbation, abrupt change in neuro status Acute threatening illnesses such as severe respiratory distress, acute MI, pulmonary embolus, peritonitis, acute renal failure Invasive tests with identified risk factors Elective surgery with risk factors Drug therapy requiring intensive monitoring Decision not to resuscitate or de-escalate care Summary of Decision Making Summary of Results of Complexity (Level of Medical Decision Making) Straigh tforwar d Low Compl ex Number of diagnoses or treatment options (points) <1 2 minimal limited 3 multiple >4 Extensive Amount and complexity of data (points) <1 Minima l or low 3 multiple >4 extensive Highest Risk minimal low moderat e High 2 limited Moderat High e Compl Comple ex x If all 3 are not at the same level, then level of medical decision making is determined by the second highest indicated. Established Office Visit Level 2 (99212) Level 3 (99213) Level 4 (99214) Level 5 (99215) History Prob-focused Expanded PF Detailed Comprehensiv e Exam Prob-focused Expanded PF Detailed Comprehensiv e MDM (complexity) Straight forward Low Moderate High Approximate time 10 min. 15 min. 25 min. 40 min. Level is determined by at least 2 components in the same level. Level 1 (99211) is a minimal visit that may be done by ancillary staff New Patient/Consultation I II III IV V History PF EPF Detailed Comp Comp Exam PF EPF Detailed Comp Comp MDM SF SF Low Medium High New patient—Has not had any professional face-to-face services from the provider or any provider in the same specialty in the group in previous 3 years. Requires 3 components on the same level. Preventative Services By age, coverage and reimbursement are preset and vary by insurance Medicare does not cover a routine yearly physical Welcome physical in first year Other preventative services and screenings at determined intervals Must use appropriate codes Counseling/Coordination of Care For an encounter dominated by counseling about a medical condition or coordination of care, time is a determining factor. For outpatient visit, must be face-to-face time For inpatient, can be time on unit Time can be estimated Must document 3 components: total time, at least 50% of the visit was spent counseling, nature of the counseling Incident To Paid at full physician fee schedule amount NPs and other non-physician providers are usually allowed at 85% Usually used for follow up of a physician’s patient following the same plan of care. Incident To Providers Auxiliary personnel: RNs, LPNs, Technicians Non Physician Providers (NPPs): NP, PA, CNS, CNM (can supervise auxiliary personnel for payment, except in hospital outpatient departments) Physical therapists, occupational therapists, clinical social worker On claim report both name and NPI of initiating physician and supervising physician Requirements Services must be furnished in the office (not hospital) Furnished under direct supervision of a doctor Must have employment relationship Are integral, although incidental to the doctor’s services. Commonly rendered without a physician charge but incur some expense (for dressing change, drug administration) Direct Supervision Supervising physician can be any member of the group Must be present in the office suites and immediately available. Does not need to speak to or lay hands on the patient. Employment Relationship Employee Leased employee Independent contractor of physician or legal entity that employs or contracts physician Documentation must Identify who rendered the service Indicate supervision requirement is met Show physician’s initiation and continued involvement in treatment plan Show that care was reasonable and necessary Show that care was within the scope of practice of NPP Modifiers 25—significant, separate E&M performed by same provider on same day 24—unrelated E&M done by provider at post operative visit 50—bilateral (pays 150%) 51—multiple procedures Documentation should show medical necessity and what was done in addition Comprehensive Error Rate Testing CMS program monitors accuracy of claims and payments National error rate is 4.5% Maryland and surrounding states: 4.3% Services associated with errors: Consults 27% --Established office visits 21% other outpatient 21% Initial hospital 15% ---Subsequent 13% Billing and Coding Tip Document every visit using a SOAP note with subheads and bulleted points for HPI (OLDCART, PQRST), ROS, related past/family/social history, exam by systems, diagnoses, and treatment plan. You will more easily be able to determine the E&M level, or if you document electronically, a computer program may determine the E&M. Resources Center for Medicare and Medicaid Services www.CMS.hhs.gov www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.aps (Documentation Guidelines) www.cms.hhs.gov/MLNProducts/downloads/1995dg.pdf (1995 Guidelines) www.cms.hhs.gov/MLNProducts/downloads/master1.pd f (1997 Guidelines) www.cms.hhs.gov/manuals (Claims processing) Resources (cont.) Highmark Medicare Services www.highmarkmedicareservices.com www.highmarkmedicareservices.com/faq/p artb/index.html (Frequently Asked Questions) www.highmarkmedicareservices.com/partb /reference/scoresheets.html (E&M score sheets)