NurseLecture_PelvicPain_060514
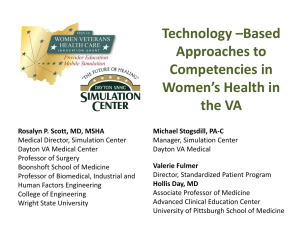
advertisement

Pelvic Pain Learning Objectives Discuss common causes of acute pelvic pain Discuss common causes of chronic pelvic pain Identify triage questions to differentiate urgent vs. non-urgent presentations Describe components of a pain evaluation Provide appropriate patient education Case Study Becky, a 39-year-old female veteran calls with a complaint of pelvic pain that started 24 hours ago. Nurse’s Critical Thinking: Assess the urgency of the complaint. VETERANS HEALTH ADMINISTRATION 3 Triage Questions to Assess Acute Pelvic Pain Pregnancy • LMP? Form of birth control? Pain characteristics • Location? Does it radiate elsewhere? Has location changed? • Duration? Where/when did it occur? • Onset sudden or gradual? Sharp, dull, stabbing? Pain come and go (cyclic)? • Rate pain on scale: 1=minor to 10=unbearable • What makes it worse/better? Treatment tried? • Similar pain before? If yes, how treated? Past gyn surgery Past STIs Other symptoms Bowel movement pattern • • • • Hysterectomy, oophorectomy, or tubal ligation? When? How treated? Nausea, vomiting, vaginal discharge/bleeding Constipation? Diarrhea? Both? 4 Case Study (continued) Becky states that she has never had pain like this before. She tried acetaminophen and ibuprofen, but neither helped. Her LMP was 2 weeks ago and she has a history of tubal ligation. Nurse’s Critical Thinking: Becky is probably not pregnant. A clinic appointment is appropriate. VETERANS HEALTH ADMINISTRATION 5 Signs & Symptoms Purulent vaginal discharge (possible STI) Cramping, vaginal bleeding (may be ectopic pregnancy or threatened AB) Dyspareunia, dysmenorrhea (suggest endometriosis) Anorexia, nausea and vomiting (seen with appendicitis) Pelvic pain (inflammatory process such as PID, or adnexal torsion/twisting, or degenerating fibroid) Dysuria (suggestive of UTI) Constipation and/or diarrhea ACUTE PELVIC PAIN VETERANS HEALTH ADMINISTRATION 7 Definition of Acute Pain Definition Varies… Pain <1 week Pain undiagnosed for <10 days VETERANS HEALTH ADMINISTRATION 8 Common Causes of Acute Pelvic Pain Gynecologic Conditions (PID, dysmenorrhea) Gynecologic and Pregnant (ectopic pregnancy, miscarriage) Non-Gynecologic Conditions (appendicitis, UTI, diverticulitis, kidney stones, trauma) VETERANS HEALTH ADMINISTRATION 9 Physical exam and nursing role for acute pelvic pain Immediate vitals − Marked hypotension, tachycardia, or fever: may need emergency treatment − Pregnant: follow local policy for disposition of acutely ill pregnant patient − Heavy vaginal bleeding: consider orthostatic vitals Set up supplies for a complete pelvic exam 10 Patient Education for Acute Pelvic Pain • Questions about treatment plan or discharge instructions? • How to reach provider including after-hours contact (e.g., 24-hour nurse advice line) • Understanding of when/if she is to return for follow-up • When to seek immediate emergency care ─ If pain worsens ─ If fever develops ─ If orthostatic symptoms appear (lightheadedness or passing out, confusion, nausea, blurred vision) VETERANS HEALTH ADMINISTRATION 11 Pregnancy should be ruled out for every woman of reproductive age who complains of acute pelvic pain. VETERANS HEALTH ADMINISTRATION 12 CHRONIC PELVIC PAIN VETERANS HEALTH ADMINISTRATION 13 Definition of Chronic Pelvic Pain (CPP) Non-cyclical pain for at least 6 mos in pelvis, anterior abdominal wall, lower back or buttocks AND serious enough to cause disability or lead to medical care VETERANS HEALTH ADMINISTRATION 14 Epidemiology of CPP Occurs in 15% of reproductive-aged women Cited as diagnosis in 10% of outpatient GYN consultations 40% of women undergo laparoscopic surgeries due to CPP The reason for 18% of all hysterectomies >$2 billion in costs per year Not associated with race, ethnicity, education, socioeconomic status Co-Morbidities 50% of women with CPP also have depression (consider depression screening) Drug and alcohol abuse may make women more susceptible to pain 16 CPP is also associated with: Physical and sexual abuse Military sexual trauma VETERANS HEALTH ADMINISTRATION • Of 713 women in pelvic pain clinic: − 46.8% hx of sexual/physical abuse − 31.3% PTSD symptoms − Trauma hx = worse medical symptoms (headache, muscle ache, constipation, diarrhea) • Prevalence of MST, which includes harassment, is 1 in 5 among all women Veterans ─ Hx of MST = twice as likely to report chronic pelvic pain 17 Common Physiologic Causes of CPP GI Gynecologic (e.g., irritable bowel syndrome) (e.g., endometriosis) Urologic Musculoskeletal (e.g., interstitial cystitis) VETERANS HEALTH ADMINISTRATION (e.g., fibromyalgia) 18 CPP Diagnosis • • • 61% of cases, no diagnosis 40% more than 1 diagnosis Four most common physiologic causes: − Endometriosis − Adhesions − Irritable bowel syndrome (IBS) − Interstitial cystitis VETERANS HEALTH ADMINISTRATION 19 Triage Questions to Assess Chronic Pelvic Pain Had this type of pain before? Describe today’s pain Location, duration, intensity, etc. Today’s pain differ from prior episodes? If yes, how? Associated symptoms? • Sudden weight loss may occur with malignancy • Nausea and vomiting may occur with bowel obstruction Pain timing? Constant? Associated with menses, eating, intercourse, or stress? Pain intensity? Rate on scale: 1=minor to 10=unbearable Treatments tried? Today? In the past? Anyone in her family have chronic pain? If yes, what? Does she have a pain plan? If yes, is she following it? When did it stop working? Physical exam and nursing role for CPP Vital signs Listen to her concerns and prepare provider Set up supplies for complete pelvic exam VETERANS HEALTH ADMINISTRATION 21 Trauma-Informed Care: Before the Exam Nursing: • Tell your provider if the patient has a trauma history or if she is reluctant to have a pelvic exam Provider: • Talk with the patient (while dressed) about her symptoms • State that, to do a complete assessment, a pelvic exam is necessary because the exam may reveal more than her history • Discuss ways to relieve her stress • Reassure her that she can stop the exam at any point VETERANS HEALTH ADMINISTRATION 22 Be Alert for Trauma-Informed Care: The Exam Signs of Trauma Nursing: • Watch for: Tears Silence or staring Nervous chatter • Employ distractions Providers: • Get permission before starting and re-starting the exam • If signs of distress appear, ask if she would like a minute to relax or if she would like to delay the rest of the exam VETERANS HEALTH ADMINISTRATION 23 Important Aspects of Care for CPP Patients Addressed as an individual by a supportive team Pain is taken seriously and legitimized Information and involvement in her plan of care VETERANS HEALTH ADMINISTRATION Explanation for her condition (more so than a cure) Reassurance: Pain is not “all in her mind” Not serious/cancer 24 Patient Education for CPP • Questions about treatment plan or discharge instructions? ─ e.g., If she is to keep a pain diary, reinforce what she should record (episodes of pain including location, severity, mood at the time as well as associated factors such as menses, activity, intercourse, bowel functions, and medications • How to reach provider including after-hours contact (e.g., 24-hour nurse advice line) • Understanding of when/if she is to return for follow-up • When to seek immediate emergency care ─ If pain worsens or fever develops ─ If orthostatic symptoms appear (lightheadedness or passing out, confusion, nausea, blurred vision) VETERANS HEALTH ADMINISTRATION 25 Most Common Causes of CPP Irritable Bowel Endometriosis Interstitial Cystitis Pelvic Adhesions VETERANS HEALTH ADMINISTRATION 26 Irritable Bowel Syndrome (IBS) Abdominal pain/discomfort with altered bowel habits for at least 3 mos • Colon spasms and food moves too quickly or too slowly through intestines • Affects 20% of the population • 1.5x more common in women • Onset before age 35 in 50% of cases • Poorer physical and mental health reported with IBS 27 Diary (document everything eaten and symptoms) Dietary manipulation (nutritional consult, add fiber slowly) Exercise and Stress Management Medication and Other Therapies (biofeedback, probiotics, peppermint oil) IBS Patient Education Elimination Diet Eliminate all for 2 weeks; slowly add one food group every 3 days; record symptoms ● Dairy (lactose) ● Wheat (gluten) ● High fructose corn syrup ● Sorbitol (chewing gum) ● Eggs ● Nuts ● Shellfish ● Soybeans ● Beef ● Pork ● Lamb Endometriosis • Mean age at diagnosis 25-30 • May be caused by endometrial cells implanting outside uterus • Exact cause not known • Affects 3-15% (avg 10%) of population • 25-50% of infertility population VETERANS HEALTH ADMINISTRATION 30 Endometriosis Symptoms • • • • • Pelvic pain in 70-75% of women Increasing dysmenorrhea Deep dyspareunia Premenstrual dysmenorrhea Lower abdominal pain, often bilateral • Lower back pain • Bowel or bladder symptoms ─ Difficult or painful defecation, bloating, constipation, diarrhea VETERANS HEALTH ADMINISTRATION The stage of endometriosis is NOT correlated with the presence or severity of symptoms. Instead, symptoms are more related to local peritoneal inflammatory reaction. 31 Physical Exam History Laparoscopy Endometriosis Diagnosis Could treat based on H&P alone. Laparoscopy, however, is “gold standard”. VETERANS HEALTH ADMINISTRATION Patient Education for Endometriosis Can often be managed in primary care setting with medications alone • NSAIDs • Monophasic oral contraceptive, vaginal ring, or contraceptive patch continuously for 3 months ─ If you take away her menses, you REMOVE most of the pain cycle! Sometimes, however, patients will need GYN referral for further management VETERANS HEALTH ADMINISTRATION 33 Interstitial Cystitis (IC) • Definition: 3-6 mos of pain/pressure/discomfort over suprapubic area or bladder, with frequent urination day and night in a patient without a UTI − Major symptoms in women are dysuria, frequency, urgency, chronic pelvic pain, dyspareunia • Bladder pain can be variable; most consistent feature is increased discomfort with bladder filling and relief after voiding • 90% of all IC cases are female; diagnosis should be high on suspicion list if her pelvic pain can’t be controlled • Symptoms vary over time with flares and remissions • Cause is unknown; may be defects in protective lining (epithelium) of the bladder • No cure; goal is to relieve symptoms and improve quality of life • Patients often referred to Urology for further evaluation/management 34 IC Patient Education • Dietary management: low potassium, low acid diet trial x 2 wks. Eliminate: - carbonated drinks - pickled foods - caffeine (including chocolate) - alcohol - citrus products - spicy food - tomatoes - artificial sweeteners • Some patients urinate up to 60x per day - Retrain bladder by slowly increasing voiding intervals. Patients may mention knowing location of every bathroom in town. Some are confined to their homes due to incontinence if a bathroom is not readily available. • Pelvic floor/easy stretching exercises can reduce muscle spasms • Some improvement reported with acupuncture, guided imagery, biofeedback • Symptoms can sometimes be managed by applying heat or cold over perineum. Encourage patients to try both to see what works. Psychosocial support is also an integral part of treatment for chronic pain disorders. Bands of scar tissue form between pelvic organs Pelvic Adhesions Lead to infertility, chronic pain VETERANS HEALTH ADMINISTRATION Risk factors: infection, pelvic surgery, trauma Pelvic Adhesion Diagnosis Aggravated IBS symptoms or pain during sexual intercourse Diagnosed by excluding other pathology GYN referral for potential laparoscopy VETERANS HEALTH ADMINISTRATION 37 Addressing Co-Morbidities with Pelvic Adhesions These patients can be the most difficult to manage. They present with a chronic pain history that is suggestive of adhesions mainly because everything else has been ruled out. Sending them back to surgery is not the best option. The first step is a depression screen and a good assessment of the patient’s alcohol and drug use to rule out abuse. As mentioned in an earlier slide, pain can be exacerbated by overuse of alcohol and drugs. This is the point where the involvement of a mental health provider is crucial. VETERANS HEALTH ADMINISTRATION 38 Patient Education for Pelvic Adhesions • • • Avoid constipation High-fiber diet Pain management Medications, physical therapy, trigger point injections, Botox injections, biofeedback • VETERANS HEALTH ADMINISTRATION Goal is to try to keep them out of the OR as long as possible 39 The bottom line regarding CPP… • • • • Chronic pelvic pain is a complex condition. Patients need a good triage assessment to determine care urgency Many women have concurrent depression, PTSD, MST, or IPV Existing data is hampered by a lack of standard definitions, algorithms, and adequate clinical trials; regardless, our patients rely on us to listen and arrive at the best treatment plan possible • Nurses are on the front line. Your involvement in taking a complete history, encouraging compliance with the plan of care, and listening when women become frustrated with their chronic pain is crucial • Multidimensional care is often warranted; recognize when to bring in the team to help manage these patients. Consider involving your mental health provider or your PACT team or the social worker. VETERANS HEALTH ADMINISTRATION 40 Helpful Resources • Bordman & Jackson. Below the belt: approach to chronic pelvic pain. Can Fam Physician 2006;52:155662. • Meltzer-Brody et al. Trauma and posttraumatic stress disorder in women with chronic pelvic pain. Obstet Gynecol 2007;109:902-8. • Price J, et al. Attitudes of women with chronic pelvic pain to the gynaecological consultation. BJOG Int J Obstet Gynaecol 2006; 113:446–452. VETERANS HEALTH ADMINISTRATION 41 Patient Education Resources • Womenshealth.gov − Irritable bowel syndrome − Endometriosis − Interstitial cystitis/bladder pain syndrome • International Pelvic Pain Society. Chronic pelvic pain booklet (6 p.) VETERANS HEALTH ADMINISTRATION 42 Authors Megan Gerber, MD, MPH VA Boston Healthcare System Sarina Schrager, MD, MS University of Wisconsin-Madison Department of Family Medicine Lisa Roybal, MSN, WHNP-BC Loma Linda VA Health Care System Linda Baier Manwell, MS University of Wisconsin-Madison Division of General Internal Medicine Molly Carnes, MD, MS University of Wisconsin-Madison Center for Women’s Health Research VETERANS HEALTH ADMINISTRATION 43