Document
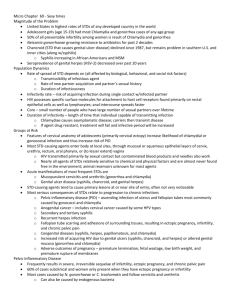
advertisement

Genital Discharge : 1st : Gonococcal (specific) cause 2nd : Nongonococcal (nonspecific) cause GONORRHEA (GC) causative agent and Pathogenesis *Albert Ludwig Sigismund Neisser 1879 *Neisseria gonorrhoeae Gram-negative, aerobic diplococci intracellular *mode of transmssion: sexual contact ,poor hygiene or medical use of urine, vertical transmssion *virulent factors: PilC and Opa, adhesins and sphingomyelinase, IgA proteases, lipooligosaccharide endotoxin *disseminated infection: Delays in antibiotic treatment, physiologic changes in host defenses, resistance to immune responses, and highly virulent strains of bacteria Clinical Findings *LOCALIZED DISEASE (MEN): I.P 2-8 d…..2wks, 10% asymptomatic - urethritis: cloudy or purulent discharge from the penile meatus, painful urination and surrounding redness and swelling, Testicular pain and swelling may indicate epididymitis or orchitis Proctitis, rectal mucopurulent discharge, pain on defecation, constipation, and tenesmus in MSM higher risk of acquiring HIV infection… damaged epithelial integrity Pharyngitis caused by N. gonorrhoeae is rare, asymptomatic * LOCALIZED DISEASE (WOMEN): 50% asymptomatic Sterility, urethritis…mucopurulent discharge, vaginal pruritus, and dysuria sites of infection: commonly endocervix, Bartholin's and Skene's glands upper genital tract… PID (10-40%) Cervicitis urethritis *PID: fever, lower abdominal pain, back pain, vomiting, vaginal bleeding, dyspareunia, and adnexal or cervical motion tenderness Sequelae…tubo-ovarian abscesses, subsequent ectopic pregnancies, chronic pelvic pain, and infertility due to chronic inflammation with resultant scarring *Fitz-Hugh-Curtis syndrome: inflammation of the liver capsule, up to one-fourth of women with PID caused by either N. gonorrhoeae or C. trachomatis. c/f: right upper quadrant pain and tenderness with abnormal liver function tests *DISSEMINATED DISEASE: DGI...0.5-3% classical tried dermatitis, migratory polyarthritis, and tenosynovitis Skin features 40-70% small macules or hemorrhagic pustules on an erythematous base located on palms and soles, erythema nodosum or erythema multiforme like. (a) Early macular lesion *Disseminated gonococcal infection (c) Papule with central necrosis (b) Haemorrhagic pustule (d) Arthritis of the foot Laboratory Tests 1. Culture & Gram stain Culture is “gold standard” dx test for years modified Thayer-Martin medium In men done on secretions or urethral swabs, in women done on endocervical and endourethral specimens 2. FDA approved chemiluminescent DNA probes 3. nucleic acid amplification tests (NAATs)…. In DGI culture from blood, joint fluid, and skin lesions Complications -infertility as a result of untreated PID -DGI can lead to septic arthritis….permanent joint damage. Meningitis and endocarditis are rare manifestations of DGI. fever, malaise, and perihepatitis (Fitz-Hugh-Curtis syndrome) Prognosis and Clinical Course excellent with appropriate antibiotics DGI good prognosis if treated before permanent damage Treatment 10-30% of people with gonococcal infection are co-infected with Chlamydia..routine dual therapy with doxycycline and azithromycin decreases the development of antimicrobial resistance in bacteria Treatment of Localized, Uncomplicated Gonococcal Infection Single dosage of any of the following: Cefixime, 400 mg PO Ceftriaxone, 125 mg IM Ciprofloxacin, 500 mg Ofloxacin, 400 mg PO Levofloxacin, 250 mg PO Patients allergic to cephalosporins or quinolones may be treated with spectinomycin, 2 g in a single IM dose. In dual therapy for chlamydia, add: Azithromycin, 1 g orally in a single dose Doxycycline, 100 mg orally twice a day for 7 days Management of Disseminated Gonococcal Infection Recommended regimen: Ceftriaxone 1 g IM or IV every 24 h Alternative regimens: Cefotaxime 1 g IV every 8 h or Ceftizoxime 1 g IV every 8 h or Ciprofloxacin 400 mg IV every 12 h or Ofloxacin 400 mg IV every 12 h or Levofloxacin 250 mg IV daily or Spectinomycin 1 g IM every 12 h All of the preceding regimens should be continued for 24-48 h after improvement begins, at which time therapy may be switched to one of the following regimens to complete at least 1 wk of antimicrobial therapy: Cefixime 400 mg PO twice daily or Ciprofloxacin 500 mg PO twice daily or Ofloxacin 400 mg PO twice daily or Levofloxacin 500 mg PO once daily Treatment of Gonococcal Infection in Neonates Ceftriaxone, 25-50 mg/kg/day IV or IM in a single daily dose for 7 days, with duration of 10-14 days if documented meningitis or Cefotaxime, 25 mg/kg IV or IM every 12 h for 7 days, with duration of 10-14 days if documented meningitis Gonococcal ophthalmia neonatorum should be treated with ceftriaxone, 25 to 50 mg/kg IV or IM, not to exceed 125 mg in a single dose Contraindications Pregnant woman……tetracyclines or quinolones Rx cephalosporin or a single 2-gram dose of spectinomycin can be used for gonococcal infection, and erythromycin or amoxicillin for chlamydia NGU -50% ….Chlamydia -10-30% ….Ureaplasma urealyticum & Mycoplasam genitalium -less than 10%....Herpes v., T. vaginalis, Haemophilus sp., Anaerobic bact. -1/3 of cases….. No infectious cause found CHLAMYDIA causative agent and Pathogenesis chlamys means “cloak draped around the shoulder.” C. trachomatis is a nonmotile, Gram-negative, obligate intracellular organism with 15 serotypes: A through C cause chronic conjunctivitis D through K cause urogenital tract infections L1 though L3 cause lymphogranuloma venereum I.P 1-3 weeks Modes of transmission: oral, anal, vaginal Co-infection com. with GC Type G …….SCC Life cycle: elementary body (infectious form) host cell (by endocytosis) Replication by binary fission (inside host cell) using ATP secondary differentiation primary differentiation reticulate bodies hundreds of reticulate bodies Large intracytoplasmic inclusions Clinical Findings asymptomatic infection 80% of women and 50% of men Urethritis….a watery or mucoid discharge from the urethra that may be accompanied by dysuria in both men and women. Rectal infection may result in proctitis in both men and women & chronic prostatitis. In women...intermenstrual, postcoital bleeding & lower abdominal pain PID & sterility 5-10% perihepatitis (Fitz-Hugh-Curtis syndrome) In Newborns…conjunctivitis ophthalmia neonatorum …. Pneumonia after 1 to 3 months Laboratory Tests 1. Traditionally… tissue culture from endocervix in women, urethra in men, rectum, or conjunctivae 2. direct fluorescent antibody test 3. Enzyme immunoassays 4. nucleic acid amplification, such as PCR and ligase chain reaction Complications Reactive arthritis syndrome Reiter’s syndrome 1-3% …1 month after NGU, classic triad NGU, arthritis, and conjunctivitis, HLA-B27 Additionally fever, malaise, myalgias, asymmetric joint stiffness, lower back pain, cutaneous lesions involving the genitals, and aortic regurgitation Prognosis and Clinical Course Early treatment… excellent prognosis 95% eradicating infection Sexual contact should be avoided Treatment of Chlamydia Infection Azithromycin, 1 g PO in a single dose or Doxycycline, 100 mg PO twice a day for 7 days Recommended treatment for pregnant women: Erythromycin, 500 mg PO four times a day for 7 days Amoxicillin, 500 mg PO three times a day for 7 days GENITAL MYCOPLASMAS causative agent and Pathogenesis self-replicate extracellularly, colonizing the respiratory and urogenital tracts Disseminated infection is rare…in immunocompromised hosts M. genitalium and Ureaplasma sp…. isolated from lower urogenital tracts of men with urethritis and women with cervicitis and PID M. hominis…. isolated from cases of salpingitis Clinical Findings May be undiagnosed urethritis, cervicitis, PID, endometritis, salpingitis, and chorioamnionitis Laboratory Tests Limited…….reference laboratories M. hominis and U. urealyticum,…..cultured on special media PCR assay……detect M. genitalium Complications disseminated disease, especially in immunocompromised hosts…. respiratory tract invasion, osteomyelitis, or infectious arthritis Prognosis and Clinical Course Prognosis in immunocompetent hosts is excellent with appropriate treatment and prompt diagnosis. Treatment similar to treatment for chlamydia. Fluoroquinolones….an alternative treatment against M. hominis and Ureaplasma sp. in cases of resistance to other antibiotics TRICHOMONAS VAGINALIS causative agent and Pathogenesis STD caused by parasitic protozoa Women….vagina, urethra, cervix, Bartholin and Skene glands, bladder Men…external genital area, ant. urethra, epididymis, prostate, semen I.P… 4 and 28 days Women…..asymptomatic carrier state to inflammatory vaginitis Most men are asymptomatic carriers Clinical Findings Women…malodorous, yellow-green vaginal discharge, vulvar pruritus and erythema, dyspareunia, lower abdominal discomfort, or dysuria On exam., punctate hemorrhages…vaginal wall and cervix. colpitis macularis or strawberry cervix.…specific sign of trichomoniasis, 1- 2% percent of women during a regular pelvic exam 45% of cases with use of colposcopy. Men…balanitis, epididymitis, and prostatitis Co-infection with other STDs Laboratory Tests 1. saline wet mount of a vaginal swab…common diagnostic test 2. microscopically…ovoidshaped protozoa….phase contrast or dark-field 3. anaerobic culture….positive within 48 hours 4. PCR Complications premature delivery, early rupture of membranes, and low birth weight in newborns increased risk of HIV transmission,& atypical PID Prognosis Excellent…. after appropriate treatment Treatment of sexual partners is important to avoid re-infection Treatment of Trichomoniasis Metronidazole, 2 g PO in a single dose or Metronidazole, 500 mg PO twice a day for 7 daysa Alternative recommendations Tinidazole, 2 g PO in a single dose THANKS FOR LISTENING