Health personnel
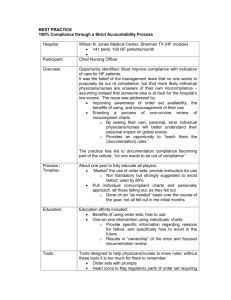
advertisement

Health Service Professionals Chapter 4 Health Services Professionals Learning Objectives To recognize the diff types of health service professionals To differentiate between primary and specialty care, and the causes for imbalance between the two in the U.S. Discuss maldistribution in the physician labor force To help overcome the physician imbalance and maldistribution To understand the role of non physician providers To identify Allied Health professionals and their role The discuss the functions and qualifications of health service administrators Health Services Professionals • The US health care industry is the largest and most powerful employer • 3% of the total labor force • 13.2% of the Gross Domestic Product • Health care will continue to grow because: 1) growth in population 2) aging of the population Health Services Professionals Types of professionals: • • • • • • • • • • • Physicians Nurses Dentists Pharmacists Optometrists Psychologists Podiatrists Chiropractors Nonphysician practitioners Health administrators Allied health professionals • Therapists • Social Workers • Educators Health Services Professionals • Health professionals among most educated and diverse • Look at Tabl 4-1, page 118 • Work places • • • • • • • • • • • Hospitals Managed Care Organizations Nursing Homes Mental health facilities Insurance firms Pharmaceutical Companies Outpatient Community Health Centers Mental Health Centers School Clinics Many others – you name a few Health Services Professionals • 43.4% employed by hospitals • 14.8% by nursing and personal care facilities • 14.6% physician offices and clinics Health Personnel • Physicians • Play a central role in evaluating the patient • States require licensure • Graduate from an accredited medical school • Pass licensure • Complete residency • Paid graduate medical education • 2-6 years • number of active physicians increased • Look at Table 4-2, page 120 Health Personnel • Physicians • Two types: • MD - Doctor of Medicine • views medical treatment as active intervention to counter reaction to neutralize the effects of disease • Most are Specialist • DO – Doctor of Osteopathic Medicine • emphasizes the musculoskeletal system of the body such corrections of joints or tissue • Most are Generalist Health Personnel • MDs and DOs • Both use accepted methods of treatment • (ie drugs, surgery) • They differ in their: • Philosophies and approach to medicine Health Personnel • Osteopathic medicine • Practiced by DO’s • Stresses preventative medicine • (ie diet, environment, other factors) • Takes a holistic approach • < 6% of physicians are osteopaths Health Personnel Physicians: Generalists and Specialists • Primary Care Physicians (Primary Care Provider) / Generalists • Train in family medicine/general practice, general internal medicine and pediatrics • Provide preventative medicine • (ie exams, immunizations, mammographies, pap smears) • Patients problems less severe and occur less frequently Health Personnel Physicians: Generalists and Specialists • Specialists • Physicians in nonprimary care specialties • Must seek certification in a medical specialization • Takes more years of advanced residence training plus years of practice • 6 Functional Groups: 1) internal med 2) medical 3) Obstetrics/Gynecology 4) Surgery 5) Hosp-based Radiology, anesthesiology, pathology 6) Psychiatry Health Personnel Physicians: Generalists and Specialists • Specialists • General Practitioner/Family Practice accounts for greatest proportion of ambulatory care visits • Obstetrics/Gynecology: • spent most hours in patient care per week • highest in operating expense and malpractice premium • Surgeons paid most ($269,000 per year) Difference between Primary and Specialty Care Primary Care • Different accord to time, focus and scope of service to patients • 5 Areas of Distinction: 1) the first contact to the health care system 2) in managed care, primary care providers are “gate-keepers” 3) primary care is longitudinal, they follow up in treatment and coordinate care • they serve as patient advisors and advocates 4) focuses on the whole person • holistic, integrates 5) spend much time in ambulatory care settings Difference between Primary and Specialty Care Specialty Care • 5 Areas of Distinction: 1) Seen after patient has seen a General Practitioner usually 2) Requires referral from a Primary Care Provider to see a patient 3) Episodic, more focused and intense 4) Limited to an illness episode • Deal with specific disease or body organs 5) Time spent in inpatient hospitals, using state-of art technology Issues in Medical Practices 1) Involvement in Clin Practice Guidelines 2) Threat of Compromise 3) Lopsided Medical Training 4) Aggregate physician Oversupply 5) Geographic Maldistribution 6) Specialty Maldistribution 7) International Medical Graduates (IMG) Issues in Medical Practices 1) Involvement in Clinical Practice Guidelines • To align practices with research • Due to increase in health care cost, the viability of the health care delivery system is under constant threat • Physicians are constantly justifying cost over benefit 2) Threat of Compromise • Physicians’ professional judgment compromised to meet managed care’s financial arrangements 3) Lopsided Medical Training • Too many specialists in a primary care setting Issues in Medical Practices 4) Aggregate Physician Oversupply • 173% increase from 1950 to 1990 • Balanced Budget Act ’97 capped residency that Medicare would pay • • Payments >$7 billion per year, >$70,000 per resident Government does not mandate how these physicians will be trained • Led to unnecessary health care expense • Shortages in parts of the country exist • Maldistribution • a surplus or shortage of physician types needed to maintain the health status of a population Issues in Medical Practices 5) Geographic Maldistribution • Shortages outside metropolitan areas (<50k) • Shortages exist because: • • • • • • • Less income Less professional interaction Little access to facilities and technology Less continuing education and professional growth Lower standards of living Fewer social and cultural diversities Less education for children Issues in Medical Practice 6) Specialty Maldistribution • An imbalance between primary and specialty care • From 1965 to 1992, • the number of primary care physicians increased by only 13%, • the number of specialists increased 121% • In the US, • approximately 34.5% of the physicians are generalists • approximately 65.5% are specialists • 25-50% in other countries are specialists Issues in Medical Practice Reasons for specialty maldistribution: 1) Medical technology 2) Reimbursement methods 3) Specialty-oriented medical education • (See Table 4-6 page132) • Specialists: • • • • • Make more Better work hours More prestige Use high technology Intellectual challenge Issues in Medical Practice Consequences of Too Many Specialists: • High volume of intensive, expense and invasive procedures • Rises health care costs • Surgeries grew at two times the rate of population growth Key Issues in Medical Practice 7) International Medical Graduates (IMG) • Steadily growing • ¼ of residency positions are filled by IMGs • Move from rural to urban areas thereafter • Not the solution to the maldistribution Types of Health care Care Personnel • Dentists • Dental Hygienists • Dental Assistants • Pharmacists • Other Doctoral-Level Health Professionals • • • • Optometrists Psychologists Podiatrists Chiropractors • Nurses • Registered Nurses • Licensed Practical Nurses • Advanced Practice Nurses • Non Physician Practitioners • Physician Assistants • Nurse Practitioners • Certified Nurse Midwives • AH Professionals • • (includes many health-related professionals) See Chart 4-2, page 144 • Health Services Administrators Dentists • Must be licensed to practice • DDS – Doctor of Dental Surgery • DDM – Doctor of Dental Medicine • Eight specialties recognized by American Dentist Association • • • • • • • • Orthodontics – straighten teeth Oral/maxillofacial surgery – mouth and jaw Pediatric dentistry Periodontics – treat gums Prosthodontics – artificial teeth or dentures Endodontics – root canals Public health dentistry – community Oral pathology – disease of the mouth Dentists • Major role: • Diagnose and treat dental problems related to teeth, gums and mouth • Dental hygienists • Do preventative dental care • Clean, educate • Must be licensed • Dental Assistants • Help in the preparation, exam and treating of patients • Do not need licensure Pharmacists Role: • Dispense medicine prescribed by doctors, dentists, podiatrists, psychiatrists • Consult on selected uses of medicine • Need license to practice • PharmD degree, 6 years of education • $70,000 in 2000 Other Doctoral-Level Health Professionals • Optometrists • Psychologists • Podiatrists • Chiropractors Other Doctoral-Level Health Professionals • Optometrists • Provide vision care with • Exams, diagnostics, correction • Need license • Doctor of Optometry (OD) • Usually work in solo or group practices Other Doctoral-Level Health Professionals • Psychologists • Provide patients with mental health care • Need license • Doctor of Philosophy (PhD) or Doctor of Psychology (PsyD) Other Doctoral-Level Health Professionals • Podiatrists • Treat disease or deformities of the feet • Includes surgeries, medicine, corrective devises • Need a license • Doctor of Podiatric Medicine (DPM) Other Doctoral-Level Health Professionals • Chiropractors • Treatment by hand manipulation, physiotherapy and dietary counseling • Help patients with neurological, muscular, vascular problems • Believes body is self-healing • Do not prescribe medicine or do surgery • Need license to practice • Doctor of Chiropractic (DC), 4 years Nurses • The largest group of health care professionals • Profession developed after World War I • The major caregivers of sick and injured patients • Addressing physical, mental and emotional needs • Need to be licensed to practice • 2 levels: • Registered Nurses (RN) • Licensed practical nurses (LPN) Nurses • As average length of stay decreased, demand for nursing fell, • but patients are sicker and more nurses are needed • work more intensive • Shortfall of 110,000 nurses • 120,000 trained but not working • In 2008, 331,000 RNs will need to be replaced Nurses Reasons for shortfall: • sluggish wages • low job satisfaction • inadequate career mobility • falling nursing enrollments • demand from other alternative hospital sites Nurses Nurse Reinvestment Act of 2002 • grants and scholarships to attract and keep • most money goes to nursing schools, but hospitals will benefit • encouraging nurses to get: • • • • • higher education training internships retention to enhance role of nurses Advanced Practice Nurses Nurses who have an education and clinical experience is required for a Registered Nurse 4 Areas of Specialization: 1) Clinical Nurse Specialist (CNS) – hospital 2) Certified Registered Nurse Anesthetist (CRNA) 3) Nurse Practitioners (NP) - primary care 4) Certified Nurse Midwives (CNM) Nonphysician Practioners (NPP) • Clinical professionals who practice in many areas similar to a physician, but • do not have a physician or DO degree • “Delivery extenders” Nonphysician Practioners • Physician Assistant (PA) • Part of the health care team who works in a dependent relationship with a supervising physician to provide comprehensive care • Licensed to do medical procedures under supervision of a physician • supervision can be on or off-site • Duties include: • evaluation, monitor, diagnostics, therapy, counseling, referral • Follows a medical model • focuses on disease Nonphysician Practioners Nurse Practitioners • have completed study with competence of an RN in an expanded role • largest group of NPPs that has most growth, but • may be declining • follows a nursing model with • health promotion and education Allied Health Professionals • Includes many health-related areas • Constitutes 60% of U.S. health care workforce • 2 Broad Categories: 1) technicians/assistants 2) Therapists/technologists • Look at Exh 4-2, page 144 Health Service Administrators • Employed at various levels of organizations • Manage integrated delivery organizations that are complex • • • • • MHA - Master in Health Administration MHSA - Master in Health Serv Admin MBA – Master in Business Administration MPH – Master in Public Health MPA - Master in Public Administration/Affairs Health Service Administrators Challenges: • financing and payment structures • work with decreasing levels of reimbursement • pressure of uncompensated care • high quality • community health service • demands by both public and private payers • new policy developments • changing competitive environment • maintaining integrity Summary • Health care is the largest labor force • Professions influenced by: • • • • demographic trends advances in research and technology disease and illness trends changing environment