OHC - CLAS Users
advertisement

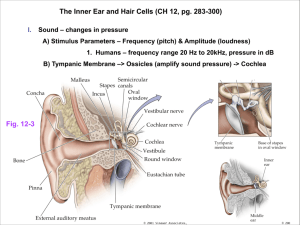
Dimensions of the cochlear partitions Cochlea: Narrower toward the apex Basilar membrane: Narrower at the base and wider toward the apical end Apical end: Flaccid and under no tension Base end: Stiff and under a small amount of tension Cochlear microstructure Organ of Corti Lies on the basilar membrane in the scala media Contains many different types of specialized cells Organ of Corti Pillar cells or rods of Corti Provide structure and support Inner and outer pillar cells Form a tunnel called tunnel of Corti Contains fluid called cortilymph Hair cells On the outer side of the outer pillar/rod cells: Outer hair cells (OHC) (Away from modiolus) On the inner side of the inner pillar/rod cells: Inner hair cells (IHC) (Toward the modiolus) Supporting cells OHC supported by cells of Deiter and Hensen IHC supported by border cells of the inner sulcus Reticular lamina Formed partly by the phalangeal processes of the Deiter’s cells. OHC Around 12000 in number Test-tube shaped Three-five rows IHC Around 3400 in number Flask shaped Single row Stereocilia Hairlike projections Project from the top of IHC and OHC Graded in length Have cross-bridges called tip-links Stereocilia of OHC and IHC OHC: 6-7 rows per OHC Each row has a W shaped arrangement IHC: 2-4 rows per IHC Each row in a shallow Ushaped arrangement Tectorial membrane Gelatinous transparent membrane projecting from spiral lamina Attaches loosely on outer edge to the Deiter’s and Hensen’s cells. Longest stereocilia of OHC embedded in inferior surface of tectorial membrane Stereocilia of IHC not embedded in tectorial membrane Physiology of the cochlea Mechanical response of cochlea in response to sound Two major functions: 1. Analysis of sound into components: Frequency/Spectral analysis 2. Transduction of sound: Converting mechanical energy into electrochemical/neural energy http://www.neurophys.wisc.edu/animations/ Mechanical response of cochlea to sound Basilar membrane moves in response to stapes vibration This vibration takes the form of a ‘traveling wave’ (von Bekesy) Wave motion starts at the base and moves toward the apex http://www.iurc.montp.inserm.fr/cric/audition/english/corti/fcorti.htm Instantaneous basilar membrane pattern and envelope of traveling wave Characteristics of traveling wave Points of maximum displacement: Peak Peak depends on the frequency of incoming sound Each part of basilar membrane ‘tuned’ to a particular frequency called critical/center/characteristic frequency (CF) Low frequencies: Localized toward the apex High frequencies: Localized toward the base Frequency/Spectral analysis Cochlea acts as a series of bandpass filters Incoming sound broken down into individual sinusoidal components Basilar membrane vibrates in response to each of these components Basilar membrane mechanics Greater the stimulus level, greater the amount of basilar membrane displacement Temporal pattern of basilar membrane vibration follows that of incoming sound Input-output functions At mid-intensity levels, basilar membrane vibration increases with intensity in a non-linear or compressive fashion At very low (< 30 dB SPL) and very high (> 90 db SPL), linear vibration This is frequency dependent: Only for the CF Above and below the CF: Linear input-output functions Steps in transduction Mechanical vibrations translated into neural responses in the auditory nerve Stapes vibration sets inner ear fluid into vibration Basilar membrane vibrates Shearing motion of tectorial membrane Stereocilia of haircells bend http://www.iurc.montp.inserm.fr/cric/audition/english/corti/fcorti.htm Bending of stereocilia http://www.iurc.montp.inserm.fr/cric/audition/english/corti/hcells/ohc/fohc.htm http://www.iurc.montp.inserm.fr/cric/audition/english/corti/fcorti.htm Transduction, Cont’d. Increase in number of open ion channels at tip links Influx of positive pottassium and calcium ions into the cell body Resting membrane potential of endolymph: + 80 mv Intracellular resting potential: OHC: -70mv IHC: - 45mv Change in membrane potential Release of neurotransmitter Neuron at the base of the haircell fires Transduction, Cont’d. Increase in number of open ion channels at tip links Influx of positive pottassium and calcium ions into the cell body Resting membrane potential of endolymph: + 80 mv Intracellular resting potential: OHC: -70mv IHC: - 45mv Change in membrane potential Release of neurotransmitter Neuron at the base of the haircell fires Differences between OHC and IHC IHC: True sensory part of the cochlea Only forward transduction (Mechanical to neural) OHC: Both sensory and motor functions Forward and backward transduction (Mechanical to neural, and neural to mechanical) Physiology of OHC and IHC OHC display ‘motility’ (change in length) in response to stimulation. IHC do not. Because of muscular contractions within the cell body and efferent connections to the OHC bodies. Thought to be basis of ‘cochlear amplifier’ and ‘active cochlea’ What is the cochlear amplifier? ‘Feedback loop’ within the Organ of Corti, because of OHC motility. Forward transduction: Basilar membrane moves, stereocilia are deflected, tranduction current flows into the OHC. This transduction current causes a change in the receptor potential (depolarization). Reverse transduction: Depolarization triggers the motility of the OHC. This change in length exerts force on the basilar membrane, deflecting the stereocilia and so on. OHC feed energy back into the basilar membrane!! Evidence for active versus passive cochlea History: von Bekesy measured broad traveling waves in dead cochleae. However, finely-tuned tuning curves measured for auditory neurons. Fine tuning of basilar membrane is lost when OHC die. Compressive non-linearity (as seen in input-output curve) lost when OHC are damaged. Most important evidence for active cochlea: Otoacoustic emissions. Otoacoustic emissions (OAE) Responses that originate within the inner ear May be spontaneous or evoked Generated due to The feedback system in the cochlea Active processes within the cochlea Non-linearities within the cochlea Tuning in the basilar membrane Vibration of basilar membrane can be described by a ‘tuning curve’ Amplitude required for the basilar membrane to vibrate at a certain constant displacement, as a function of the frequency of the input sound Neural connections in the cochlea Afferent and efferent fibers of the VIIIth cranial nerve (auditory nerve) Afferent: From organ of Corti to brain Efferent: From brain to organ of Corti Peripheral processes of auditory nerve neurons enter the cochlea through small openings on the edge of the osseous spiral lamina These openings are called ‘habenulae perforata’ These fibers are then gathered in the modiolus Organization of the auditory nerve bundle in the modiolus Fibers from the apex in the middle Fibers from the base on the outside This nerve bundle then goes to the cochlear nucleus in the brain Afferent fibers Around 30,000 neurons in man Only 5-15% of these innervate the OHC These are called Type II or outer spiral fibers One neuron connects to one OHC (one-to-many) Rest innervate the IHC These are called Type I or radial fibers Many neurons connect to one IHC (many-to-one) Efferent fibers Originate from the olivocochlear bundle in the auditory brainstem Efferent fibers synapse on the afferent nerves innervating the IHC Efferent fibers synapse directly on the OHC Discharge pattern of a neuron Neural spike has an initial large potential shift Following this, refractory or rest period of around 1 msec Other terms Spontaneous discharge rate: Neuron’s discharge rate without a stimulus Threshold: Minimum stimulus level needed to cause an increase in the discharge rate above the spontaneous discharge rate Spontaneous rate and thresholds Neurons with high spontaneous rate: Low threshold Neurons with low spontaneous rate: High threshold Rate-Level function Also called input-output or intensity function Increase the level of the acoustic stimulus and measuring changes in the discharge rate of a single neuron Response area Also called isolevel or isointensity curve Iso: “Same” Plotting how a neuron fires in response to sounds of different frequencies at a fixed intensity Tuning curve Define a certain threshold for a neuron Plot the level of the tone required for this neuron to discharge at this threshold, as a function of the frequency of the tone Encoding of frequency Two theories: 1. Place theory Tonotopic organization 2. Temporal theory Based on the periodic nature of nerve firing Place theory Different neurons in the nerve respond to different frequencies Frequency of input determined by which neuron(s) in the auditory nerve fires at the greatest rate Temporal theory For lower frequencies (< 5000 Hz), discharge rates of neurons are proportional to the period of the input stimulus. So for lower frequencies, rate of discharge of the neuron also provides information about the frequency of the stimulus. Encoding of intensity Increase in discharge rate with increase in stimulus intensity However, for most neurons, increase in discharge rate only occurs for a limited range of input intensity Possible that discharge rate of many neurons may be combined to account for the 140 dB dynamic range of the ear Psychoacoustics Branch of psychophysics Relation between the physical aspects of sound and the perception of sound Psychoacoustic correlate of intensity: Psychoacoustic correlate of frequency: Threshold Threshold of detection Absolute threshold Just detectable level of sound Threshold of discrimination Difference limen (DL) or Just noticeable difference (JND) Just detectable difference between two sounds 1000 Hz tone 4000 Hz tone Minimum audible curve Plot of threshold as a function of frequency Minimum audible pressure (MAP) Measured using headphones Minimum audible field (MAF) Measured in free field using loudspeakers 10 Hz 20 Hz 100 Hz 1000 Hz 2000 Hz 4000 Hz 250 Hz 8000 Hz 500 Hz 10000 Hz Dynamic range of hearing Range between threshold of hearing and threshold of pain About 140 dB in normal hearing listeners Temporal integration Signal must contain some critical amount of energy to be detected. If time is short, then needs more power to be detected (power = energy/time) For sounds below a certain duration (300ms), the threshold of detection decreases with duration. Ear summates or integrates energy over time.