GTD Case Study
advertisement

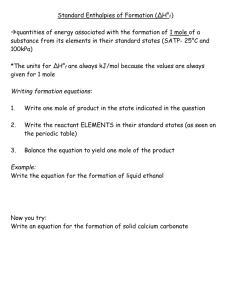
Diagnosis and management of hydatidiform mole Diagnosis and evaluation of postmolar GTN Case Scenario A 21 year old nulligravida presents with bleeding during early pregnancy. Last normal menses was 9 weeks ago, home urine pregnancy test was positive 2 weeks ago, and she has been spotting for two days with heavier bleeding the last 6 hours. Examination: afebrile, BP 130/84, P 112, T 37.4. the patient is anxious and tremulous, oriented X 3. The uterine fundus is not tender and palpable mid-way between symphysis and umbilicus. FHTs not present. Pelvic: Cervical cyanosis, uterus enlarged to 14 weeks’ size, bilateral 6 cm cystic adnexal masses. Questions What is your differential diagnosis? What initial diagnostic tests would you obtain? What ancillary tests would be helpful for managing this patient? Laboratory Results Serum beta hCG 510,000 mIU/ml Ultrasound: mixed echogenic intrauterine mass with no fetus identified. Bilateral septated ovarian cysts. CBC: WBC 8,900; hct 27%; plates 252k Electrolytes, Cr, LFTs normal T4 elevated 2 X normal, TSH normal CXR: No effusions, infiltrates, nodules or edema Ultrasound Images Questions What is your primary diagnosis? What are secondary diagnoses? What is your management plan? Initial Management Beta blockers are begun to stabilize the secondary hyperthyroidism caused by stimulation from hCG Blood is cross-matched in the event that transfusion is required Large-bore IV is started The patient is taken to the operating room for an emergent suction D & E to evacuate the hydatidiform mole Theca lutein cysts will be monitored after evacuation, but do not require operative intervention Initial Management During suction D&E a large amount of grape-like tissue clusters are evacuated. EBL is 500 mL. Pitocin is started by IV infusion after cervical dilatation; there is prompt uterine involution and scant bleeding. In the recovery room, the patient becomes tacchypneic and tacchycardic, with generalized rales. SaO2 is 88% on 2 liters oxygen via nasal prongs. Questions What is your differential diagnosis for this patient’s acute respiratory decompensation? What diagnostic tests could be obtained to aid in management? Post-evacuation CXR Management of ARDS CXR now demonstrates diffuse pulmonary edema with no evidence of trophoblasticembolization. Electrolytes are normal, Cr normal. Hct has fallen to 22%, WBC 11,000, and plates 300k The patient is transferred to the ICU for monitoring in the event that intubation is required. She is transfused, treated with furosemide, and improves with resolution of ARDS over 36 hours Hospital Course On POD #3 the patient is transferred out of the ICU with SaO2 98% on room air and ambulatory. Uterine involution to 4-5 weeks’ size, persistent 6 cm cystic adnexal masses. No vaginal bleeding. Pathology: Complete hydatidiform mole hCG 80,000 mIu/mL Hct 28% Electrolytes, LFTs normal T4 1.5 X normal Questions How should this patient be monitored after evacuation of hydatidiform mole? Why is she being monitored? How soon can she attempt pregnancy? How should she prevent pregnancy during monitoring? Are there any risks during subsequent pregnancy after a hydatidiform mole? Monitoring after Hydatidiform Mole The patient is scheduled for weekly serum quantitative beta hCG testing until normal values (<5 mIu/ml), and then monthly hCG values for at least 6 months. Follow-up pelvic examination in 2-3 weeks to monitor her ovarian theca lutein cysts. Thyroid function tests will be repeated during that visit. The patient is offered, and accepts, oral contraceptives to prevent pregnancy during monitoring with hCG values. She is counseled that she has an increased (1-2%) risk of a second mole in subsequent pregnancies. She is counseled that her risk of malignant GTN is increased (>50%) because of the very high hCG, theca lutein cysts and medical complications of her molar pregnancy Monitoring after Hydatidiform Mole The patient’s hCG rapidly drops to 8,000 mIU/mL by week 4 and examination reveals regressing ovarian cysts. Subsequent monitoring as follows: Week 5: 7,800 mIU/mL Week 6: 8,500 mIU/mL Week 7: 10,050 mIU/ml – the patient reports increased vaginal spotting Questions What is your provisional diagnosis? What additional diagnostic tests should be obtained? What tests will be obtained to aid in management? What general category of treatment will be given (eg: surgery, radiation therapy, chemotherapy)? Evaluation of GTN An ultrasound reveals persistent tissue in the uterus and bilateral 4 cm theca lutein cysts. CXR reveals 3 new lesions, each 1-2 cm Brain MRI is negative for metastases. CT of chest/abdomen/pelvis reveals approximately 15 bilateral pulmonary subcentimeter metastases, in addition to the lesions noted above. No other metastases are noted. hCG is confirmed to be 11,000 mIU/mL CBC, electrolytes, Cr, and LFTs are essentially normal Management This patient has low-risk postmolar GTN. FIGO Stage II by staging studies FIGO risk score < 8 She is offered single-agent chemotherapy with intramuscular methotrexate She is counseled that her chance of cure without requiring multiagent chemotherapy or hysterectomy is > 90% and overall cure rates approach 100% If hysterectomy can be avoided, future fertility is not affected by methotrexate 1-2% risk of second mole