Biosafety Program Management
advertisement

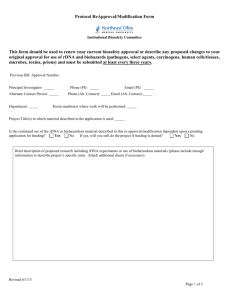
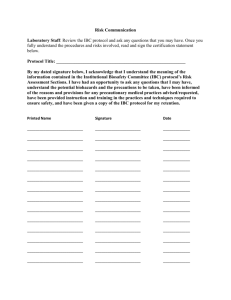
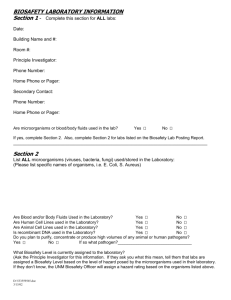
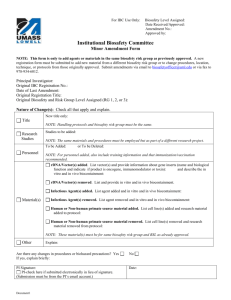
Biosafety Program Management EMD Lecture #3 Biosafety Program • Institutional oversight & acceptance – President, CEO, CFO • Institutional Biosafety Committee (IBC) – peer review, adopt/establish policies • Biosafety Office – inform, administer program, assist • Faculty, staff, students & visitors – merge biosafety into work Related Compliance Entities • • • • • • IRB IACUC ICC Grants & Contracts Police, Security Other Regulations/Responsibilities • 1970 OSH Act – 5(a)(1) General Duty Clause • Related OSHA Standards – PPE, BBP, EtO, Labels, HAZWOPER, etc. • NIH Guidelines (rDNA) – Applicability, scope • Transport – DOT, IATA, USDA, CDC/PHS, DoC, other Regulations/Responsibilities • Agencies – FDA, EPA, NIH OHRP, State, City • Guidelines – CDC/NIH BMBL, CDC TB, APIC, WHO, NSF 49, etc. • Training – BBP, TB, Shipping, Biosafety, Lab Safety, PPE, Infection Control, special hazards Information to Employees • • • • • • • Hazard awareness Risk (toxicity/disease), signs/symptoms Exposure limits/infectious dose Employer’s responsibilities Protective measures (controls) Medical surveillance/monitoring Emergency response procedures Biosafety Program Management I GO WHERE I’M TOWED TO! Biosafety Program Management • IBC as DMV – speed limits, rules/regulations – registrations/renewals, fines • Program is tow truck and pace car – safely deliver to desired location • BSO as State Police – inform, assist, control, emergency response Biosafety Program Management • Employees – luxury, economy, SUV’s, dragsters, stalled, etc. • AAA – Administrative support – Active (pro-active biosafety program = awareness) – Accountability for compliance at all levels Biosafety Program Management • Adopt/mandate required policies • Apply OSHA General Duty Clause elsewhere • Establish policies where needed Rationale • Control hazards – Anticipate – Identify – Evaluate • Prevent lab-acquired infections – Interaction – Proactive – Assumption of responsibility Prevention • Interaction – Registration/reauthorization – Initial and periodic training & inspections – Sanctions • Evaluation – Risk assessment/risk management – Incidents/near misses Risk Assessment & Risk Management Prior Planning Prevents Poor Performance Risk Assessment & Risk Management • • • • • Pathogen Procedures Personnel Place Protective Equipment Ineffective Program Management • • • • • • Morbidity/mortality Perceived lack of institutional control Regulatory visit/action Legal action (civil/criminal penalties) Bad press Low morale Biosafety Program Management • “I go where I’m towed to!” – “Tell ‘em where you’re going to tow them” – “Tow ‘em where you want them” – “Tell ‘em why you’ve towed them there” Identification of Biological Agents Identification of Agents • • • • • • Department PI/Lab Director Type of Lab Lab Supervisor Building(s)/room(s) Phone/fax/email/campus address Identification of Agents • rDNA – exempt/non-exempt, IBC, NIH-OBA registration • Human material – OSHA regulated, other • Plants – low risk, plant pests, pathogens, USDA APHIS requirements Identification of Agents • Human Pathogens – Risk group – local, state, federal registrations • Animals – natural infections – work with biohazards – work with animal pathogens Identification of Agents • • • • • Human subjects Healthcare/clinical locations Toxins of biological origin Shipping/transport of regulated agents Other? Identification of Equipment • Autoclaves • Biosafety cabinets, clean benches, glove boxes • Eyewashes, showers • Centrifuge containment Identification of Handlers • • • • • Name, employee ID Number Campus address/contact information Identify work experience Observe work practices if necessary Refresher training as needed Biosafety Database Management Occupationally exposed workers • • • • • • • Bloodborne Pathogen training (initial/annual) Biosafety Training (initial/periodic) HBV Vaccination program (other immunizations) TB Training, PPD Test Shipping/Transport Training (biennial) BSL3 Training/certification of researchers Select Agent registration/training/review Equipment & Facilities • Autoclave (location, testing) • Clean air device (location, certification) • biosafety cabinets, ventilated enclosures – repairs, moves • BSL3 facilities – commissioning – annual air balancing – HEPA filter testing Research Registration • Comprehensive Biohazard Registration Form (all biological materials used) • rDNA protocols (new, updates, new personnel) • Human pathogens (biennial) • Select Agent transfers (inventory, tracking) • Inspections (semi-annual, annual) – BSL1, BSL2, BSL3, Animal, Select Agents Institutional Documentation • • • • IBC minutes (subcommittee deliberations) Approval letters Safety Manuals (periodic updates) Incidents – Non-compliance reports – Accidents, exposure investigations and recommendations – Serious adverse events (human subjects) Biosafety Manual Biosafety Manual • Introduction/Contact Info/Overview • Responsibilities – – – – – Chairperson Principal Investigator/Manager Researcher/Employee Safety Office IBC Biosafety Manual • Requirements – – – – – – – Annual registration Human etiologic agents/select agents rDNA Regulated human material Biohazards in animals/USDA Regulated agents Clean air device program Training Biosafety Manual • Medical Surveillance/Employee Health – – – – – – – Screening Immunization Medical restrictions Serum storage Incident reporting/evaluation/follow-up Counseling Records Biosafety Manual • Risk Assessment/Risk Management – – – – – – Biosafety levels Routes of transmission Signs/labels Work practices Personal protective equipment Protective equipment/engineering controls Biosafety Manual • Decontamination – – – – Disinfectants Sterilization methods Medical waste program Treatment of mixed wastes Biosafety Manual • Spill/Emergency Response – Spill kits/training/preparation – BSL1, BSL2, BSL3 spill response – Mixed spills Biosafety Manual • Shipping/Transport – – – – – Clinical, diagnostic specimens Etiologic agents, toxins of biological origin Packaging Shipping declaration forms Import/export requirements Biosafety Training Biosafety Training • Lab safety – chemical, biological, fire, security, incident response • Biosafety – – – – human/animal pathogens RG2/BSL2 rDNA proficiency/competency Biosafety Training • Bloodborne Pathogens – Initial @ time of hire • specific components of standard • targeted to audience – Annual retraining – Sharps Safety Devices • Evaluation & training Biosafety Training • BSL3 Training – – – – – – work practices, PPE, controls biosafety cabinet facility operations spill/incident response formal evaluation of proficiency inspection of proposed SOP Biosafety Training • Shipping/Transport of Infectious Substances – IATA (initial and every 2 years) – DOT (initial and every 3 years) • labs working with etiologic & other regulated agents • provide info to those handling clinical specimens – Shipper/transporter/receiver • general awareness • function specific Biosafety Training • Tuberculosis – – – – – At time of hire, screening Infection control Proposed annual training requirement Respiratory protection Healthcare and beyond! Biosafety Training • Effective Use of the Biosafety Cabinet – recommended – part of Biosafety training – can require based on audit results Institutional Biosafety Committee Role of the IBC • Established by highest administrator • Oversight for potentially hazardous work • Set policy for safe conduct of biohazard research • Oversee rDNA projects; ensure compliance • Responsibilities not restricted to rDNA IBC Membership (NIH rDNA) • varied disciplines (rDNA, microbiology, lab safety, engineering, lab technical staff, legal, community) • > 5 members (2 from community) • plant pathogen/containment expertise • animal containment expertise • biosafety officer if BL3/BL4 or large scale IBC Membership • • • • consult with other scientists as needed annual report to NIH/OBA suggest opening meetings to public minutes available to public upon request Suggested IBC Subcommittees • • • • Human Gene Transfer Clinical Trials Xenotransplantation Medical Surveillance Biosafety Level 3 • All report back/through IBC IBC Function • review rDNA research • assess physical/biological containment level • assess: – – – – facilities procedures practices training/expertise of personnel IBC Function • Infectious agents, toxins, other biohazards – – – – – review PI written risk assessment perform risk assessment/assign RG or BSL train personnel, verify proficiency, retrain inspect proposed work practices/area periodically monitor • Design/commissioning containment labs – annual verification IBC Function • periodically review rDNA research • adopt emergency response plans • report significant accidents/illnesses to state local public health agencies & NIH/OBA • report significant problems/violations of guidelines to NIH/OBA IBC Function • communicate results of review to PI • don’t authorize initiation of work not covered by guidelines w/out NIH review • ensure compliance with surveillance data reporting for human gene transfer projects IBC Function • Sanctions – – – – – – establish framework in advance develop with related institutional entities acquire administrative backing perform case by case review work with & prevent repeat document, file, and report to required bodies Communication with Related Committees/Groups • • • • • • NIH OBA, OHRP FDA CBER CDC, USDA IACUC IRB Grants & Contracts Occupational Health Program Goals of Health Program • prevention of occupational illness and injury • early recognition of health alterations due to exposure • prompt treatment and management of occupational illness/injury Occupational Health Program • identify employees at risk – medical history compared to hazards of position • pre-placement medical evaluation – baseline health information – pre-existing conditions • determine need for medical surveillance • schedule update of work/health history Occupational Health Program • understand the risks faced by employees • inform of hazards and methods of protection • educate on warning signals of illness (prompt visit to health clinic) • clear procedure for reporting incidents and exposures Medical Evaluation • BL3, BL4, non-human primate handlers, respirator users • pre-assignment/periodic evaluations – immunization status – base-line tests (TB, biochemical analysis, serology) – high risk medical conditions (GI disorders, pregnancy, immunosuppressive drugs, etc) Immunizations • effective vaccine • condition of employment? • evidence of antibody response before starting work • booster or revaccination as necessary Serum Storage • potential to monitor serological changes resulting from employee’s exposure • sample at time of hire, annually, after overt exposure, at termination • test at time of collection if agent produces known serological response • confidential • informed consent (may decline) Report of seroconversion • examine worker • investigate procedures • revise procedures to eliminate exposure Accidents & Illnesses • prompt reporting • immediate medical assistance – serum samples, stool specimens, nasal and skin washings • investigate serious, unusual or extended illnesses Employee Health Records • • • • confidential exposure reports serious illnesses maintain for duration of employment plus 30 years