Cases 2: Critical reasoning
advertisement
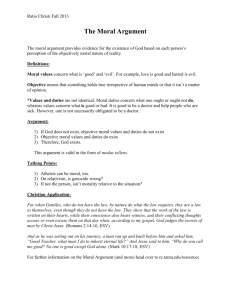
Critical reasoning in healthcare ethics Maggie Barker MD MPhil FFPH 13th September 2014 What is an argument? • An argument presents a conclusion –look for words such as ‘so’, ‘therefore’, ‘should’ • Based on information or reasons - often signalled by words such as ‘since’, ‘as’, ‘because’ • Prudential (practical) argument :‘If you want x you should do y’ What is a moral argument? • You should do y, regardless of your aims and interests, because it is the right thing to do.’ • A moral argument has a conclusion which makes a moral claim • Often expressed as recommendations using ‘should’ or ‘ought’ • ‘Should’, ‘ought’, ‘right’, ‘wrong’ are evaluative terms • Evaluative adjectives -‘cruel’, ‘admirable’ – often used in moral statements: ‘ A moral argument If there was a prenatal test for autism would this be desirable? What would we lose if children with autistic spectrum disorder were eliminated from the population? We should start debating this. There is a test for Down’s syndrome and that is legal and parents exercise their right to choose terminations, but autism is often linked with talent. It is a different kind of condition. Main conclusion • We should start debating whether a prenatal screening test for autism, with selective termination of affected pregnancies, would be desirable. • This conclusion is arrived at through analogy with Down’s screening, and through two intermediate conclusions. Step 1:Screening for Down’s syndrome 1st intermediate conclusion (and unstated assumption) Children with Down’s syndrome are being eliminated from the population Because: Reason 1: • There is a [prenatal screening] test [with selective termination of affected pregnancies] for Down’s syndrome Reason 2: • This is legal • Unstated assumption: And ethically acceptable Reason 3: • Parents exercise their right to choose terminations Step 2: Extending screening to autism 2nd intermediate conclusion: By contrast, if children with autistic spectrum disorder were also eliminated from the population through prenatal screening, we would lose something [“talent”]. Because Unstated reason 4 (explanation by analogy): • Autism might seem to be like Down’s syndrome and could equally be the target for prenatal screening. Parents would opt for terminations, as they do for Down’s syndrome, so children with autistic spectrum disorder would be eliminated from the population. Reason 5: • But autism is often linked with talent, so it is different. • Unstated assumptions: Down’s syndrome is not associated with talent. We lose nothing through eliminating people with Down’s syndrome. Facts and values • ‘Good’ doctor example (10) leads us to the importance of distinguishing between medical facts and moral evaluations. • Factual statements: “blood pressure of 200/120 needs to be treated with drug x”. Evaluate using techniques of ‘evidence-based-medicine’. • Evaluative statements: “The situation is significant enough to justify taking steps to persuade the patient to take the medicine.” Here ‘significant’ meaning it matters – incorporates values. Fact/value distinction and the truth of reasons • Factual statements can be true or false • Can evaluative (moral or aesthetic) statements be true or false? Eg ‘The roses in my garden are beautiful’; ‘Lying to patients is wrong’ • Beauty is in the eye of the beholder. Is this the case for moral judgements too? Are morals merely a matter of personal taste? – In reality we do seem to treat moral positions as if they could be either true or false (eg when we try to convince someone of our conclusion). – Morals do seem to be based on reason as much as feeling – Where we use an evaluative adjective (like the cruel treatment of the mouse in our example) - isn’t this actually factual. The is/ought gap • Evaluative statements can be factual (cruel cat). But not all factual statements are evaluative – they tell us what is the case not what ought to be. • Moral arguments have evaluative conclusions but their reasons can be factual or evaluative. • Arguments that move from non-evaluative reasons to evaluative conclusions give rise to a worry called the ‘is/ought gap’. Pointed out by David Hume (1711-76): many moral arguments start out be talking about what is the case and end up talking about what ought to be the case – but difficult to see how ought can follow from what is: “No ought from is”. – Passive smoking causes cancer. Therefore smoking in public places should be banned. [a causes b therefore c(which can result in a) should be d] – Vivisection causes pain to animals. So vivisection is wrong. [a causes b. So is c] Role of emotion Emotional responses and moral intuitions need to be subjected to rational analysis. The ‘yuk’ factor may be irrational. Rational morality 1. Fair-mindedness Appreciation of different peoples’ views and various perspectives 2. Reflective equilibrium with dialogue. 3. Valid reasoning Valid reasoning: Logically sound Deductive argument is a series of statements (premises) that lead logically to a conclusion – Basic form: Syllogism (modus ponens) Premise 1: If p then q Premise 2: p Conclusion q Deductively valid argument – does not necessarily mean that the reasons and conclusion are true – but that the logic of the argument is valid. Valid reasoning: Logically sound Valid reasoning: Logically sound Invalid argument in form of syllogism Premise 1: If p then q Premise 2: Not p False conclusion: Not q Valid reasoning: Conceptual analysis • Definition of key terms • Elucidating key concepts • Making distinctions • Identifying similarities Valid reasoning • Reasoning from principles and theories • Consistency and case comparison Spotting ethical issues in clinical situations • • • • • • • • • Patient’s wishes are unclear, or patient refuses treatment Questionable capacity to consent or to refuse treatment Disagreement involving relatives End-of-life issues (advance directive, “do not attempt resuscitation” decisions, lasting power of attorney, limitation of treatment etc) Issue over goal of care or appropriateness of current treatment Confidentiality or disclosure issue Resource or fairness issue Other No notable ethical issue Sokol D 2009;BMJ:338:b879 Cases The psychiatric home treatment team visit a man in his 90s at the behest of his GP. He has had several strokes and emergency admissions to hospital. Following the strokes he is severely disabled and can no longer transfer from bed to chair or care for himself without assistance. He has expressed the desire to commit suicide recently and is refusing all medical and physical care. The home treatment team find that he has capacity to make decisions regarding his future. How should this man be treated? Cases A woman in her twenties whose pregnancy is almost at term is brought to the hospital following a road traffic accident. She is a Jehovah’s witness, and refuses all blood products. She is diagnosed with bleeding into her abdomen and into her uterus, but maintains her refusal of blood. Her foetus dies in utero, and she succumbs to her injuries soon after. Should the emergency and obstetric teams have respected her refusal of blood? Cases An elderly man who lives alone is admitted with bowel obstruction. He is listed for an emergency operation the following day, but refuses surgery, stating that he has no reason to continue living. Despite steadily deteriorating, he continues to refuse an operation. Some members of the surgical team feel that he ought to have an operation in his own interests, and others think his choice should be respected. What should be done?