Case Study
advertisement
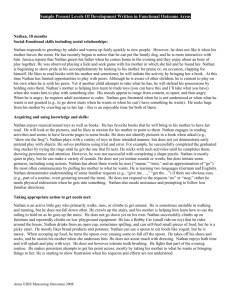
NADD Specialist Certification Training Nathan A. DeDiminico Case Study Past History: Mr. Nathan A. DeDiminico is a mid 40’s year old white male who currently receives services. He is diagnosed with Mild Intellectual Disability and Chronic Schizophrenia. His history can be related in four major frameworks: Family/ Support Systems: He is from a large, extended family, and as the youngest of the brothers and sisters, he has lived at home with his 84 year old mother and a brother in a working class neighborhood. New neighbors moved in next door about 18 months ago and they have befriended Nathan. His two sisters, one brother and a nephew identify that he had maintained a basic level of activity before his decompensation. His interests and abilities in the family home include running the sweeper, making small meals, and enjoying outside activities such as riding his bike. He had been active in his neighborhood until about a year ago doing odd jobs for neighbors on his street. Over the past five months he has had altercations with family members; pushing his mother to the floor and choking his brother. His family is extremely worried that Nathan will hurt himself or others if stabilization of his mental illness does not occur. Education/ Level of Services: Mr. DeDiminico graduated from high school. He did attend Special Education classes all of his twelve years of schooling. His sister relates proudly that he also graduated from a vocational technical program that focused on the trade of construction. He has had Supports Coordination only with monitoring which was described as non-eventful. Trauma: Mr. DeDiminico was sexually molested at the age of 17. The details surrounding this trauma were not disclosed. He was also hit by a car at the age of 10 and had multiple broken bones, evident by his left leg being shorter than the right. He was not diagnosed with a head injury from the accident however he did experience trauma to the head and 15 minutes of unconsciousness. Genetics: Mr. DeDiminico has been diagnosed with fragile X syndrome. Current Situation: According to his family members and the Medical Center Psychiatric Team, Nathan has had six psychiatric admissions within five months. These included the Extended Acute Care Facility . In the past ten years, it appears he had sporadic psychiatric admissions. Several staff at the hospital know his history as a result of these inpatient stays. The RN Manager and Psychiatrist also described his symptom increase within this five month period as the most severe they have seen to date. A high level review meeting was held for Nathan. The team and Mr. DeDiminico’s family described Nathan’s current needs as needing help and supervision with his medications, cueing for his activities of daily living, and addressing the effectiveness of his psychiatric medications. Prior to this most recent admission, he refused his medications. He threatened to kill himself. He grabbed his medications for what his sisters described as intent. He became afraid of the snow and rain. This intensified as his desire to kill himself increased in the snow. This was evidenced by increased anger, irritation, and altercations with family members. Nathan attended the meeting for about a five minute length of time. His affect was flat. It was evident that the stimulation in the room was intolerable for him. He became highly anxious as the move to a state hospital was discussed. It was clear that the thought of change/transition was overwhelming to him despite the empathetic presentation of the information and the presence of family members. During his time at the meeting, a few short moments when he did recognize family members and his supports coordinator, he brightened. He was unable to remember anyone’s name whom he had met that day. When he was excused he jaunted to the door to escape the stimulation. The presence of his family did not deter his need to avoid being with the group. The dual diagnosis clinician met and spoke with Nathan for about forty five minutes prior to the meeting. The following were observations. He appeared older than his age with sandy brown long hair, gray eyes, and a stubbly beard. He was very focused on his glasses and would often grab and pull upwards to his face. Nathan identified that he felt important for having a special meeting. He knew the day of the week but not the date. He was unable to do any mathematical computations. He also appeared withdrawn. At times he would appear to brighten and smile especially as he spoke about his family. He did complain about being very tired due to his peers on the unit being up various times of the night. According to hospital staff, Nathan is unable to identify his medications, has no insight into his illness, and/or his past actions toward his family members in his home over the past five months. As noted in the medical record, Nathan’s diagnoses (DSM5) are: Chronic Schizophrenia, Mild Intellectual Functioning, Poor eyesight, Fragile X syndrome Moderate- medication noncompliance Clinical Impression: Nathan A. DeDiminico is a mid 40’s year old gentleman who is diagnosed with Chronic Schizophrenia. The exacerbation of his mental illness over the past five months has risen to the need for intensive treatment and stabilization. Short term inpatient stays have not been able to 1 stabilize him in the community. Irritability, withdrawal and high anxiety were observed during the visit with Nathan. Symptom driven behaviors that were described by his family include suicidal threats, attempts to harm his mother and the attempted choking of his brother . During the visit, his symptom presentation was consistent across environments (on his floor and at the meeting). His inability to tolerate external stimuli was evidenced by his quick exit from the room after only a five minute period. Discussions of change and transition to a new environment were also intolerable and prompted him to remove himself from the meeting. It was apparent that his abilities described previous to his decompensation were not present. This is suggestive of severe cognitive disruption. His overall presentation indicates his symptoms of mental illness continue to be present at an intense level. It was noted by the psychiatric team that the addition of Risperadol has been added and has made a slight difference, however it is too early in the process to note long term benefit. It needs to be noted clearly that his family is very concerned about next steps after he is discharged. His family cannot continue to support him in the home. 2