Introduction to Biotechnology
advertisement

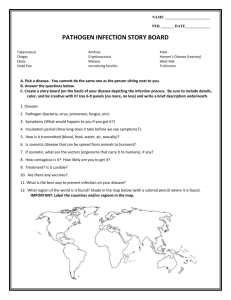
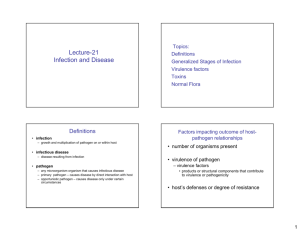
Chapter 30 Pathogenicity of Microorganisms Symbiosis the “living together” of two organisms in a variety of relationships Host-Parasitecommensalism Relationships mutualism parasitism Saprophytic organisms obtain nutrients from dead or decaying organic matter some are pathogenic but most are considered scavengers Parasites Parasites are organisms that live on or within a host organism and are metabolically dependent on the host types of parasites ectoparasite lives on surface of host endoparasite lives within host Types of Hosts Final host host on (or in) which parasite either gains sexual maturity or reproduces Intermediate host serves as temporary but essential environment for some stage of parasite’s development Transfer host is not necessary for development but serves as vehicle for reaching final host Reservoir host nonhuman organism infected with a parasite that can also infect humans Parasitism and Disease Infection growth and multiplication of parasite on or within host Infectious disease disease resulting from infection Pathogen any parasitic organism that causes infectious disease Primary (frank) pathogen – causes disease by direct interaction with healthy host Opportunistic pathogen – part of normal flora and causes disease when it has gained access to other tissue sites or host is immunocompromised Pathogenicity ability of parasite to cause disease Factors Impacting Outcome of Host-Parasite Relationships Factors: number of organisms present the degree of virulence of pathogen virulence factors e.g., capsules, pili, toxins host’s defenses or degree of resistance Table 30.1 Figure 30.1 Mathematical Expression of Infection Virulence Virulence: degree or intensity of pathogenicity determined by three characteristics of the pathogen invasiveness ability to spread to adjacent tissues infectivity ability to establish focal point of infection pathogenic potential degree to which pathogen can cause damage to host Aspects of Pathogenic Potential Toxigenicity ability to produce toxins Immunopathology ability to trigger exaggerated immune responses Measuring Virulence Lethal dose 50 (LD50) number of pathogens that will kill 50% of an experimental group of hosts in a specified time Infectious dose 50 (ID50) number of pathogens that will infect 50% of an experimental group of hosts in a specified time Figure 30.2:Determination of LD 50 Strain A LD is 30, B LD is 50 hence, A is more virulent. Pathogenesis of Viral Diseases Fundamental process of Viral infection in a host cell: maintain reservoir –a place to live and multiply before infection enter host contact and enter susceptible cells replicate within cells release from host (immediate or delayed) …Viral infection spread to adjacent cells Evade host immune response be cleared from body of host, establish persistent infection, or kill host be shed back into environment Maintaining a Reservoir most common reservoir of human viruses are humans and other animals some viruses are acquired early in host’s life and cause disease later most often, viruses are transmitted from one host to another host and cause infection in a short time frame Viral Entry Occurs at a variety of sites: via body surface via sexual contact, needle sticks, blood transfusions, and organ transplants via insect vectors organisms that transmit pathogen from one host to another Adsorption Adsorption attachment to the cell surface results from binding of viral protein to host cell receptors binding of virus to receptor results in cell penetration or delivery of viral nucleic acid to host cell cytoplasm Entry of Human Virus Nucleic Acids into Host Cell Direct entry of nucleic acid e.g., polio virus- enters the host cell and deliver viral nucleic acid into the cytoplasm of cell It enters through the human gastrointestinal tract but produces diseases in the central nervous system. endocytosis and release of nucleic acid from capsid (uncoating) e.g., pox viruses- causes small pox Fusion of viral envelope e.g. influenza –fusion of viral envelope with cell membrane of host Primary Replication Primary replication some replicate at site of entry, cause disease at same site, and do not spread throughout body others spread to distant sites and then replicate e.g., polio viruses enter through gastrointestinal tract but produce disease in central nervous system Evasion of Host Defenses begins when the virus first infects the host for the virus to cause a successful infection, it must be able to avoid host immunity so it can spread to a sufficient number of host cells to amplify the number of virions Viral Spread and Cell Tropism Viral spread vary but most common is by bloodstream and lymphatic system Viremia- presence of virus in blood Spread by way of nerves e.g rabies Tropisms Viruses exhibit cell, tissue, and organ specificities Virus-Host Interactions Cytopathic viruses local necrosis with ultimate host death alternatively, can trigger apoptosis (programmed cell death) i.e host cell dies, often before viral replication can occur Noncytopathic viruses cause latent or persistent infections …Non-Cytopathic Viruses Do not immediately cause cell death cause latent or persistent infections productive non-cytopathic viruses produce persistent infection with the release of only a few new particles at a time nonproductive non-cytopathic viruses do not actively make virus at detectable levels for a period of time (latent infection) these viruses may become productive by environmental stressors or other factors Other Outcomes of Virus-Host Interaction Clinical illness some tissues can be quickly repaired after viral damage e.g., intestinal epithelium others cannot be easily repaired e.g., tissues of central nervous system Integration of viral DNA may result in transformation of host cells into cancerous cells due to viral DNA interference with host DNA growth cycle regulation …Virus Shedding last step in infectious process is shedding of the virus in the environment needed for maintenance of viral source in a host population often occurs at same body surface used for entry of the virus at this stage host is very contagious/infectious/stay far…..can spread in some infections, host is dead (end of host) and no shedding occurs-e.g Rabies Maintain a reservoir Like viral infection Bacteria too need a place to live Pathogenesis of Bacterial before and after causing infection Diseases initial transport to/entry into host adhere to, colonize, and/or invade host …Bacterial infection initially evade host defenses multiply or complete life cycles on or in host damage host Maintaining a Reservoir of the Bacterial Pathogen For human pathogens, most common reservoirs are: other humans animals environment Transport of the Bacterial Pathogen to the Host Direct contact e.g., coughing, sneezing, body contact Indirect contact vehicles (e.g., soil, water, food) arthropod vectors fomites – inanimate objects that harbor and transmit pathogens Attachment and Colonization by the Bacterial Pathogen Adherence structures: Structures such as such as pili and fimbriae and specialized adhesion molecules on bacterium’s cell surface bind to complementary receptor sites on host cell surface Colonization: Colonization is the establishment of a site of microbial reproduction on or within host does not necessarily result in tissue invasion or damage Evasion of Host Defenses by Bacteria Successful pathogens can evade destruction by host : by: Formation of capsule- Neisseria gonorrhoeae production of leukocidins- substance that destroy phagocytes before phagocytosis can occur – Streptoccocus pneumoniae, Staphyloccocus Endotoxins Table 30.4-Bacterium polymerised host actin into long tail and for propulsion from one cell to another and out of the host. Bacterial Invasiveness Varies among pathogens e.g., Clostridium tetani (tetanus) produces a number of virulence factors (e.g toxin and proteolytic enzymes ) but is non-invasive i.e it does not spread from one tissue to another. e.g., Bacillus anthracis (anthrax) and Yersinia pestis (plague) also produce many virulence Growth and Multiplication of the Bacterial Pathogen occurs when pathogen finds appropriate environment within host some pathogens actively grow in blood plasma bacteremia – presence of viable bacteria in blood Bacteria that are able to grow and multiply in various cells of a host Facultative intracellular pathogens Intracellular Pathogens can live within host cells or in the environment e.g., Brucella abortus can grow independently as well as in macrophages, neutrophils and trophoblast cells Obligate intracellular pathogens incapable of growth and multiplication outside of a host eg., viruses and rickettsia Leaving the Host must occur if microbe is to be perpetuated most bacteria leave by passive mechanisms in feces, urine, droplets, saliva Regulation of Bacterial Virulence Factor Expression Often environmental factors control expression of virulence genes e.g., Corynebacterium diphtheriae gene for diphtheria toxin regulated by iron e.g., Bordetella pertussis expression of virulence genes increased at body temperature e.g., Vibrio cholerae Pathogenicity Islands Pathogenicity Islands- large segments of DNA that carry virulence genes acquired during evolution of pathogen by horizontal gene transfer e.g., genes for type III secretion system (TTSS) enables gram-negative bacteria to secrete and Toxigenicity Intoxications diseases that result from entry of a specific preformed toxin into host Toxin specific substance that damages host two main categories in bacteria exotoxins endotoxins Exotoxins - soluble, heat-labile, proteins and usually released into the surroundings as bacterial pathogen grows humans exposed to exotoxins in three main ways Exotoxins ingestion of preformed exotoxin bacterial colonization of a mucosal surface followed by exotoxin production colonization of a wound or abscess followed by local exotoxin production most exotoxin producers are gram-positive often travel from site of infection to other tissues or cells where they exert their effects Types of Exotoxins AB exotoxins- composed of two subunits A subunit – responsible for toxic effect once inside the host cell B subunit – binds to target cell od host specific host site exotoxins-e.g AB Exotoxins Composed of two subunits A subunit – responsible for toxic effect once inside the host cell B subunit – binds to target cell Specific Host Site Exotoxins can be AB toxins neurotoxins target nerve tissue e.g., botulinum toxin enterotoxins target intestinal mucosa e.g., cholera toxin cytotoxins target general tissues e.g., nephrotoxin Membrane-Disrupting Exotoxins do not have separable A and B subunits two types pore-forming exotoxins Phospholipases-lyses the plasma membrane e.gClostridium perfringens-gas gagresn Some Pore-Forming Exotoxins Bacterial Toxins that forms pores in the membranes: Leukocidins –membrane-disrupting toxins kill phagocytic leukocytes- pneumococci. Strepto, staphyloccus Hemolysins- other toxin that form pores in membranes of blood cells Hemolytic Reactions beta-hemolysis complete lysis observed as zone of clearing around colony on blood agar alpha-hemolysis partial lysis Phospholipase Enzymes Phospholipase Enzymes a second subtype of membrane-disrupting toxins remove charged head group from lipid part of phospholipids in hostcell plasma membranes Endotoxins Lipopolysaccharide (LPS) in gram-negative outer membrane can be toxic to specific hosts called endotoxin because it is bound to bacterium and released when organism lyses and some is also released during multiplication Polymicrobial Diseases Polymicrobial Diseases -many infectious diseases involve the interactions of more than one infectious agent these diseases can be polyviral, polybacterial, combined viral-bacterial, or polymycotic or protozoan Dental Infections Dental Infections -caused by various odontopathogens Formation of dental plaque creates environment for pathogens that produce acids and other virulence factors Figure 30.9: Plaque Development Process Figure 30.11-Microscopic Appearance of Plaque Periodontal Disease… Periodontitis initial inflammatory response to plaque bacteria and tissue destruction leads to swelling of tissue and formation of periodontal pockets Periodontosis bone destruction caused by colonization of periodontal pockets Periodontal Disease… Gingivitis inflammation of gingiva caused by colonization of periodontal pockets Treatment, prevention, and control oral surgery and antibiotic therapy in some cases plaque removal and good dental hygiene Bibliography • Lecture PowerPoints Prescott’s Principles of Microbiology-Mc Graw Hill Co. • http://en.wikipedia.org/wiki/Scientific_ method • https://files.kennesaw.edu/faculty/jhend rix/bio3340/home.html