Summer Board review General Medicine Session 3
advertisement
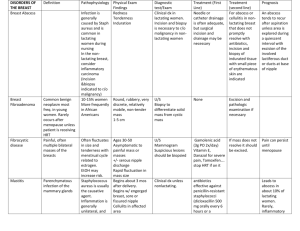
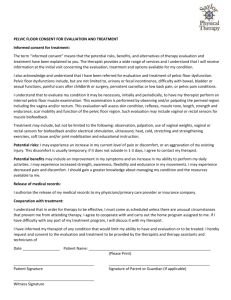
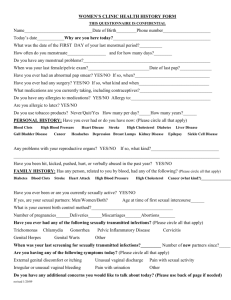
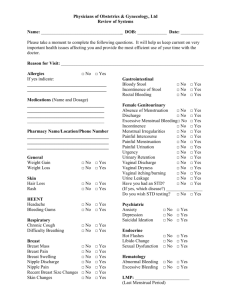
Internal Medicine Summer Board Review General Internal Medicine Session 3 Mashkur Husain Question 25 A 25-year-old woman is evaluated for a 1-week history of malodorous vaginal discharge associated with vulvar itching and burning. She is sexually active and has had three partners in the past 6 months. She has no history of sexually transmitted infection. On physical examination, vital signs are normal. BMI is 22. There is a thin, gray, homogeneous discharge coating the vaginal walls. There are no external genital lesions and no vulvar erythema or excoriations. The cervix appears normal.There is no cervical motion tenderness or adnexal tenderness.Vaginal pH is 6.0, “whiff” test is positive. Results of saline microscopy are shown (next slide) Microscopy after the addition of potassium hydroxide does not show hyphae or pseudohyphae. A urine pregnancy test is negative. Answer Choice Which of the following is the most appropriate treatment? A Clotrimazole cream, 7-day topical regimen B Fluconazole, single-dose oral regimen C Metronidazole, 7-day oral regimen D Metronidazole, single-dose oral regimen Answer Choice Which of the following is the most appropriate treatment? A Clotrimazole cream, 7-day topical regimen B Fluconazole, single-dose oral regimen C Metronidazole, 7-day oral regimen D Metronidazole, single-dose oral regimen Key Point and Education Objective Treat bacterial vaginosis Bacterial vaginosis is the likely diagnosis in women with at least three of the following features: (1) homogeneous thin discharge that coats the vaginal walls; (2) clue cells on saline microscopy; (3) pH of vaginal fluid >4.5; and (4) fishy odor of vaginal discharge (positive “whiff” test). Explanation The most appropriate treatment for this patient is a 7-day oral regimen of metronidazole (500 mg twice daily). She has bacterial vaginosis (BV), a polymicrobial infection characterized by an overgrowth of multiple anaerobic bacteria. Although BV is not a sexually transmitted infection, risk factors include lack of condom use and multiple or new sexual partners. BV can be diagnosed clinically using Amsel criteria, which include the following symptoms or signs: (1) homogeneous thin discharge that coats the vaginal walls; (2) clue cells (epithelial cells with borders obscured by small bacteria) on saline microscopy; (3) pH of vaginal fluid >4.5; and (4) fishy odor of vaginal discharge before or after the addition of 10% potassium hydroxide to the secretions (the “whiff” test). The presence of at least three of these clinical findings has a high sensitivity and specificity for diagnosing BV when compared with Gram stain of collected secretions, which is the gold standard. Because this woman is symptomatic, treatment should be offered with either oral metronidazole, vaginal metronidazole gel, or vaginal clindamycin cream; patient preference should dictate treatment choice. Topical clindamycin should be avoided during pregnancy as it may increase the risk of adverse outcomes. Women treated with oral metronidazole should be cautioned to avoid alcohol, which can cause a disulfiram-like reaction. Explanation This patient's abnormal vaginal pH and lack of yeast and hyphae on potassium hydroxide preparation make vulvovaginal candidiasis an unlikely explanation for her symptoms. Treatment with oral fluconazole or topical clotrimazole cream, effective therapies for vulvovaginal candidiasis, is not warranted. This patient has multiple sexual partners, increasing her risk for trichomoniasis. Characteristic symptoms and signs include a malodorous discharge with vulvar itching, burning, and postcoital bleeding. Although the vaginal pH will be elevated and the whiff test may be positive (as noted with this patient), clue cells are not a characteristic finding on saline microscopy, making trichomoniasis an unlikely diagnosis in this patient. Oral metronidazole is also used for the treatment of trichomoniasis, but it is typically given as a single 2-g dose, which would not be appropriate for treatment of BV. Vaginitis and Cervicitis Screening Screen all sexually active women age ≤25 years and all women age >25 years with risk factors for Chlamydia infection. Diagnosis Vaginitis is characterized by vaginal irritation, pruritus, pain, or unusual discharge. The three most common infectious causes of acute vaginitis are bacterial vaginosis, vulvovaginal candidiasis, and Trichomonas. Trichomoniasis is the only cause of vaginitis that is sexually transmitted. Noninfectious causes include allergic reactions to vaginal contraceptives or other products, such as douches, tampons, or soap; coitus-induced friction; or postmenopausal atrophy. Vaginitis and Cervicitis Cervicitis may be asymptomatic or symptomatic. When present, symptoms include vaginal discharge, postcoital bleeding, dysuria, and dyspareunia. The presence of endocervical mucopus defines cervicitis. Easily induced endocervical bleeding also may occur. Cervical motion tenderness suggests pelvic inflammatory disease. Cervicitis can be caused by Chlamydia, Neisseria gonorrhoeae, and Trichomonas. Definitive diagnosis of Neisseria and Chlamydia can be made by nucleic acid amplification test performed on vaginal or urine specimens. Vaginitis and Cervicitis Candida Albicans Clue Cell Vaginitis and Cervicitis Question 26 A 28-year-old woman is evaluated for a painful lump in her left breast of 6 weeks' duration. There is neither discharge from the nipple nor skin changes over the area. Her last normal menstrual period was 3 weeks ago and she thinks that the lump became slightly larger right before and during her menses. She is on low-dose oral contraceptives. She has no history of breast disease or breast biopsy. Menarche was at age 12 years. She has never been pregnant. A maternal aunt had breast cancer. On physical examination, vital signs are normal. BMI is 24. There is a 1.5-cm mobile, soft, slightly tender mass in the lower medial quadrant of the left breast. There is no nipple discharge and no abnormalities of the overlying skin. The right breast has no masses. There is no axillary lymphadenopathy. The remainder of the examination is unremarkable. Answer Choice Which of the following is the most appropriate management of this patient? A B C D Core needle biopsy Mammography Repeat clinical breast examination in 6 months Ultrasonography Answer Choice Which of the following is the most appropriate management of this patient? A B C D Core needle biopsy Mammography Repeat clinical breast examination in 6 months Ultrasonography Key Point and Education Objective Evaluate a breast mass in a young woman. A palpable breast mass should be evaluated until diagnosis or resolution Explanation This patient should undergo ultrasonography. A slightly tender, discrete, round, soft, and mobile breast mass, with no nipple discharge and no overlying skin changes, is consistent with a fibroadenoma or benign cyst and not breast cancer. However, no single clinical factor by history or physical examination has sufficient accuracy to rule in or rule out underlying malignancy, and diagnostic imaging should be performed. Ultrasonography serves to distinguish cystic from solid masses. A cystic mass should be aspirated and the fluid sent for cytologic evaluation if bloody or recurrent. A solid mass requires biopsy by fine-needle aspiration, core needle, or excision. A benign biopsy in a woman with a normal mammogram still requires close follow-up, as documented by a study in which breast cancer developed in 707 of 9087 women with previous benign breast biopsies followed for a median of 15 years. Explanation In general, imaging should precede core needle biopsy. A core needle biopsy will not be necessary if the mass is definitively cystic by ultrasonography. The increased density of breast tissue in women 30 to 35 years of age and younger may limit the utility of mammography, making ultrasonography a better first choice. Ultrasonography can readily distinguish cystic from solid lesions and guide further evaluation, such as aspiration, if needed. Clinical observation and follow-up in 6 months is not appropriate for a palpable breast mass, which should be evaluated until diagnosis or resolution. Breast Lump Diagnosis A dominant breast mass is defined as a lump or suspicious change in the breast texture that is discrete and distinctly different from the rest of the surrounding breast tissue. The differential diagnosis of a dominant breast mass includes cysts, fibroadenomas, fibrocystic changes, fat necrosis, carcinoma in situ, and invasive carcinoma. Don't Be Tricked Do not stop the evaluation of a breast mass if mammogram is normal. Ultrasonography is followed by aspiration of cysts or biopsy of solid breast masses regardless of mammogram results. Question 27 A 38-year-old woman is evaluated during a routine examination. She has recently divorced and is interested in some form of hormonal contraception, as her ex-husband had a vasectomy after their last child, and she does not want to use condoms. She has no history of deep venous thrombosis, hypertension, or heart disease. She drinks one glass of wine 4 or 5 nights per week, and smokes a pack of cigarettes daily. Family history is significant for stroke in her mother at age 72 years. All previous Pap smears have been negative. Physical examination, including pelvic examination, is normal. A Pap smear is obtained. Answer Choice Which of the following is the most appropriate hormonal contraceptive option for this patient? A B C D Estrogen patch Estrogen-progesterone combination Progesterone contraceptive No hormonal-based method Answer Choice Which of the following is the most appropriate hormonal contraceptive option for this patient? A B C D Estrogen patch Estrogen-progesterone combination Progesterone contraceptive No hormonal-based method Key Point and Education Objective Recommend contraception options for a woman who smokes. Estrogen-containing contraceptives are contraindicated in women older than 35 years who smoke more than 15 cigarettes daily because of the increased risk of thromboembolic disease. Explanation The best hormonal contraception option for this 38-year-old woman who smokes is a progesterone-only preparation. Women older than 35 years who smoke more than 15 cigarettes daily should not be prescribed estrogen-containing preparations because of the increased risk of thromboembolic disease. A family history of stroke itself is not a contraindication to the use of estrogen-containing preparations, although a personal history of stroke or thromboembolic disease is; progesteroneonly contraceptives are considered safe in these women. Progesterone-only options for women with contraindications to estrogen include the “mini-pill,” long-acting progesterone compounds (such as depot medroxyprogesterone acetate), subcutaneous progesterone implants, and progesterone-containing intrauterine devices. Estrogen-only patches are never appropriate for contraception; they may be used as hormone replacement therapy in postmenopausal women without an intact uterus. Combined estrogen-progesterone preparations are available in the form of patches and vaginal rings, which avoid first-pass hepatic metabolism and may limit estrogen's effects on the liver and on lipids. These products do not negate the thrombogenic effects of estrogen, however, and so they are still contraindicated in women who smoke. Contraception Key Considerations The combination estrogen-progestin OCPs, containing ethinyl estradiol and one of various progestins, are very effective. Use is associated with reduced risks of ovarian cancer and endometrial cancer. Users experience less acne and reduced severity of abnormal uterine bleeding, menstrual blood flow, and anemia. The risk for VTE is higher in patients who smoke and have thrombophilia, although routine screening for thrombophilia is not recommended. The risks for MI and ischemic stroke are higher in patients with diabetes or hypercholesterolemia. Breast cancer risk is controversial. OCPs are safe in nonsmoking women older than the age of 35 years until menopause. Contraception Other hormonal contraceptives include the topical patch, vaginal ring, progestin-only pill, and medroxyprogesterone acetate injection. A single-rod progestin implant is now available in the United States that provides contraception for 3 years. Progesterone-only contraceptives are alternatives for women who cannot take estrogen because of breastfeeding or estrogen side effects. Two types of pills are available for emergency contraception. Both must be taken within 5 days of a risked pregnancy. Levonorgestrel is the preferred formulation because it is more efficacious and has the fewest side effects. The second option is a combination of ethinyl estradiol and levonorgestrel. Nonhormonal Contraceptives Question 27 A 61-year-old woman is evaluated for hot flushes, which have been persistent for the last 10 years. They occur at least 7 times per day, last for approximately 60 seconds, and are associated with severe sweating, palpitations, and occasional nausea. She is awakened several times per night. She has tried herbal medications, including soy and black cohosh, but has not experienced any benefit. She has hypertension, type 2 diabetes mellitus, and hyperlipidemia. Five years ago, she developed deep venous thrombosis after hip replacement surgery. Her current medications are ramipril, metformin, atorvastatin, calcium, and vitamin D. On physical examination, vital signs are normal. BMI is 29. The remainder of the examination is normal Answer Choice Which of the following is the most appropriate treatment? A B C D E Citalopram Oral estrogen therapy Oral estrogen/progesterone therapy Topical (vaginal) estrogen Venlafaxine Answer Choice Which of the following is the most appropriate treatment? A B C D E Citalopram Oral estrogen therapy Oral estrogen/progesterone therapy Topical (vaginal) estrogen Venlafaxine Key Point and Education Objective Treat menopausal vasomotor symptoms Owing to cardiovascular and thromboembolic risks, systemic hormone therapy is not recommended for treatment of menopausal vasomotor symptoms in women older than 60 years who experienced menopause at the median age Explanation This 61-year-old woman with cardiovascular risk factors and a history of deep venous thrombosis should be started on a nonhormonal therapy for her hot flushes. Certain antidepressants, including serotoninnorepinephrine reuptake inhibitors such as venlafaxine, are effective nonhormonal medications for reducing menopausal vasomotor symptoms. Approximately 10% of menopausal women experience hot flushes for 7 to 10 years after the cessation of menses. This patient is continuing to experience frequent and severe hot flushes which have been refractory to conservative therapy and are decreasing her quality of life; thus, pharmacologic therapy is warranted. Systemic estrogen therapy is the most effective treatment for the relief of menopausal hot flushes and must be coadministered with progesterone in women with an intact uterus. However, combined estrogen and progesterone therapy has been shown to increase the risk of several adverse outcomes, including coronary heart disease, stroke, invasive breast cancer, and venous thromboembolism. The North American Menopause Society guideline notes that women older than 60 years who experienced natural menopause at the median age and have never used hormone therapy will have elevated baseline risks of cardiovascular disease, venous thromboembolism, and breast cancer; hormone therapy, therefore, should not be initiated in this population without a compelling indication and only after appropriate counseling and attention to cardiovascular risk factors. Moreover, this patient has a history of deep venous thrombosis, which is an absolute contraindication to initiating hormone therapy. Several nonhormonal medications have been found to be effective for the treatment of menopausal hot flushes. Notably, there is a significant placebo effect: in most studies, approximately one-third of women will experience relief of hot flushes, even if they do not receive active treatment. In numerous studies, venlafaxine, administered at doses of 37.5 mg/d to 150 mg/d, decreases hot flush severity and frequency in approximately 60% of patients (as compared with 30% who experienced benefit with placebo treatment). Paroxetine is similarly beneficial; in contrast, few studies have shown efficacy with fluoxetine or citalopram. Gabapentin and clonidine are two additional nonhormonal treatments that reduce hot flushes, but attendant side effects may limit their use in some patients. Vaginal estrogen therapy is typically used for the isolated treatment of vaginal dryness, pruritus, and dyspareunia. Treatment with vaginal estrogen tablets will improve local vaginal symptoms, but will not improve menopausal vasomotor symptoms. Menopause Diagnosis When menstruation ceases, an FSH level >30 milliunits/mL is considered diagnostic of menopause, but this finding is not usually needed for diagnosis. Perimenopause is marked by menstrual cycle irregularity, but approximately 30% of women experience the hallmarks of menopause, hot flushes and night sweats, before menstrual changes. Estrogen deficiency can lead to dyspareunia, atrophic vaginitis, dysuria, urgency, and frequency. Menopause is defined as the time following 12 months of amenorrhea. Vaginal epithelial cells contain less glycogen, resulting in increased vaginal pH and increased growth of Escherichia coli. Loss of lactobacilli leaves this pale, thin, friable tissue vulnerable to infection and ulceration. Menopause Therapy Vaginal moisturizers or lubricants are indicated for urogenital atrophy. Exercise and cessation of cigarette smoking may relieve menopausal symptoms. Use short-term hormone replacement therapy (2 to 3 years) only for patients with intolerable vasomotor symptoms. Gabapentin, serotoninnorepinephrine reuptake inhibitors (SNRIs), or SSRIs are alternatives for reducing hot flushes. Local (topical) estrogen helps relieve dyspareunia and vaginal dryness. Don't Be Tricked Do not prescribe hormone replacement therapy for prevention or relief of urinary incontinence, decreased libido, or cardiovascular risk, which could even increase with this therapy. Do not select phytoestrogens and black cohosh for the treatment of menopausal symptoms. They are no more effective than placebo. Question 28 A 42-year-old woman is evaluated for a 6-month history of heavy menstrual bleeding. She has been menstruating for the last 8 days and is still going through 10 pads or more daily with frequent clots. She has fatigue but no dizziness. Previous evaluation for this problem has included normal thyroid function and prolactin testing. She has no other medical problems and takes no medications. Pelvic ultrasonography has demonstrated a large posterior submucosal fibroid. A surgical treatment is planned in 2 weeks. On physical examination, vital signs are normal. Abdominal examination is benign, and the pelvic examination reveals a moderate amount of blood in the vaginal vault. Hemoglobin level is 10.5 g/dL (105 g/L). Pregnancy test is negative. Answer Choice Which of the following is the most appropriate next management step? A B C D Estrogen/progesterone multiphasic oral contraceptive Intravenous estrogen Oral medroxyprogesterone acetate Reevaluation in 1 week Answer Choice Which of the following is the most appropriate next management step? A B C D Estrogen/progesterone multiphasic oral contraceptive Intravenous estrogen Oral medroxyprogesterone acetate Reevaluation in 1 week Key Point and Education Objective Treat heavy menstrual bleeding Medroxyprogesterone acetate for 10 to 21 days is effective treatment for moderate menstrual bleeding. Explanation The most appropriate next management step is oral medroxyprogesterone acetate. In patients who present with menorrhagia (heavy menstrual bleeding) with a known etiology, several therapeutic agents can decrease bleeding. For moderate bleeding that can be managed on an outpatient basis, a progestational agent such as medroxyprogesterone acetate can be given for 10 to 21 days. The progesterone will typically act to stabilize the endometrium and stop uterine blood flow. Estrogen/progesterone-containing oral contraceptives may be useful in decreasing menstrual blood loss, although the doses of both agents in most typical formulations would likely be inadequate to control the degree of bleeding in this patient, particularly with a multiphasic preparation. If a specific progestational agent is not available, a monophasic oral contraceptive may be dosed four times daily for 5 to 7 days, and subsequently reduced to daily dosing until definitive treatment is undertaken. If the patient were orthostatic or dizzy from blood loss, intravenous estrogen would be appropriate. Parenteral conjugated estrogens are approximately 70% effective in stopping the bleeding entirely. Pulmonary embolism and venous thrombosis are complications of intravenous estrogen therapy. Monitoring the patient for an additional week of observation is not appropriate given her significant, ongoing blood loss. Abnormal Uterine Bleeding Question 29 A 19-year-old woman is evaluated for painful menses. She usually misses one or two days of school each month owing to these symptoms, which include cramps and nausea. Menarche occurred at age 12 years. Menses have been regular for the past 2 years, occurring every 29 days. The patient is not sexually active, and her medical history is noncontributory. She takes no medications. Physical examination, including external pelvic examination, is normal. Answer Choice Which of the following is the most appropriate management option for this patient? A B C D E Combined estrogen-progesterone contraceptive Depot medroxyprogesterone acetate Ibuprofen Measurement of follicle-stimulating hormone and luteinizing hormone levels Pelvic ultrasound Answer Choice Which of the following is the most appropriate management option for this patient? A B C D E Combined estrogen-progesterone contraceptive Depot medroxyprogesterone acetate Ibuprofen Measurement of follicle-stimulating hormone and luteinizing hormone levels Pelvic ultrasound Key Point and Education Objective Manage primary dysmenorrhea The first-line treatment for primary dysmenorrhea is NSAID therapy. Explanation The most appropriate management option for this patient is a trial of NSAID therapy, such as ibuprofen. This patient has dysmenorrhea associated with normal menstrual cycles and no pelvic pathology. Initial treatment options for primary dysmenorrhea include NSAIDs and cyclooxygenase-2 inhibitors, which inhibit the inflammation, vasoconstriction, and uterine ischemia that are thought to cause the symptoms. If symptoms are not relieved with NSAID therapy or the patient requests contraception or is sexually active, a combination estrogen-progesterone contraceptive would be appropriate. Extended-cycle formulations are particularly useful for this indication. Explanation Depot medroxyprogesterone acetate (DMPA) is a long-acting progesterone compound, administered intramuscularly or subcutaneously every 12 to 14 weeks. Long-acting progesterone therapy is a treatment option for dysmenorrhea, and also provides contraception. For adolescents and young adults, however, long-term use of progesterone therapy decreases bone mineral density owing to prolonged estrogen deficiency. Therefore, such treatment should be used with caution for dysmenorrhea or for contraception in younger women based on the risks and benefits of treatment in a given patient. In general, NSAIDs should be tried before hormonal therapy. In the absence of worrisome symptoms such as severe pelvic pain or significant bleeding abnormalities, treatment for dysmenorrhea may be initiated without further evaluation, such as pelvic imaging, hormonal testing, or gynecologic referral. Primary Dysmenorrhea Diagnosis Patients with a history of menstrual pain that begins within 1 to 2 years of menarche and sometimes worsens over time usually have primary dysmenorrhea, in which no pathologic cause for the menstrual pain exists. An underlying cause for dysmenorrhea is likely in the setting of noncyclic pain, abnormal discharge, dyspareunia, or heavy or irregular bleeding. Therapy NSAIDs are an effective first-line therapy. For women who are not trying to conceive, oral contraceptive pills are also effective therapy, as are transcutaneous electrical nerve stimulation and vitamin B1. Question 30 A 33-year-old woman is evaluated for chronic lower pelvic pain. It has been persistent for the past year but has worsened in recent months. She describes it as a constant, aching discomfort centered over her lower pelvis that persists during her menstrual cycle and has prevented her from being sexually active with her partner. She also reports a 4-month history of urinary urgency and frequency. She has been empirically treated twice for urinary tract infections, but her urinary symptoms improve for only a few days and then recur. She has no history of pelvic surgeries or pelvic infections and has never been pregnant. She has no associated constipation, diarrhea, abdominal distention, or flank pain. She currently takes ibuprofen as needed for pain. On physical examination, vital signs are normal. BMI is 24. There is mild tenderness to palpation over the pelvic floor muscles with significant tenderness over the anterior vaginal wall. External genitalia are normal in appearance; there is no tenderness to palpation over the vulva. There is no cervical motion tenderness, adnexal tenderness, or discomfort with palpation of the uterus Laboratory studies show normal electrolytes, kidney function, and a complete blood count. Erythrocyte sedimentation rate is 4 mm/h. Urinalysis is without erythrocytes or leukocytes and is negative for nitrite and leukocyte esterase. Urine culture is negative. Tests for chlamydial infection and gonorrhea are negative. Transvaginal/transabdominal ultrasonography is negative for endometrial or ovarian masses and no abnormalities are noted. Answer Choice Which of the following is the most likely diagnosis? A B C D Endometriosis Interstitial cystitis Irritable bowel syndrome Pelvic adhesions Answer Choice Which of the following is the most likely diagnosis? A B C D Endometriosis Interstitial cystitis Irritable bowel syndrome Pelvic adhesions Key Point and Education Objective Diagnose interstitial cystitis as a cause of chronic pelvic pain. Interstitial cystitis is a likely diagnosis in women with chronic pelvic pain associated with unexplained urinary symptoms; most women with interstitial cystitis have been treated empirically several times for urinary tract infections. Explanation This most likely diagnosis in this patient with chronic pelvic pain is interstitial cystitis. Chronic pelvic pain is defined as noncyclic pain of at least 6 months' duration that localizes to the anatomic pelvis, the anterior abdominal wall at or below the umbilicus, the lumbosacral back, or the buttocks, and is of sufficient severity to impair quality of life. Potential causes of chronic pelvic pain include interstitial cystitis, endometriosis, pelvic adhesions, and irritable bowel syndrome. In this patient, the combination of chronic pelvic pain in association with unexplained urinary symptoms is most consistent with a diagnosis of interstitial cystitis. Interstitial cystitis is a chronic inflammatory condition of the bladder that causes symptoms of urinary urgency, frequency, and pelvic discomfort. The pelvic discomfort may be worsened by sexual intercourse, and patients may urinate numerous times per day. Although urinalysis and urine cultures are almost always negative, most women with interstitial cystitis have been treated empirically several times for urinary tract infections. Explanation Endometriosis is a common cause of chronic pelvic pain, and patients typically report severe dysmenorrhea, cyclic pain, and dyspareunia. The absence of severe dysmenorrhea and the noncyclic nature of this patient's pelvic pain make endometriosis a less likely diagnosis. Similarly, irritable bowel syndrome is unlikely to explain her symptoms in the absence of any associated gastrointestinal symptoms. Adhesions are diagnosed in 25% to 50% of women with chronic pelvic pain. Pelvic adhesions typically form in the setting of acute or chronic inflammatory processes, such as infection, or surgery. This patient has no history of pelvic infection and has never had pelvic surgery, making this an unlikely cause of her symptoms. Endometriosis Endometriosis Don't Be Tricked Endometriosis does not cause fever or vaginal discharge. Therapy NSAIDs are first-line therapy, followed by oral contraceptives (if pregnancy is not desired) when NSAIDs are ineffective. Severe symptoms call for gonadotropin-releasing hormone agonists for pain relief. Surgical ablation or resection of endometrial tissue is recommended for patients who do not respond to conservative measures. However, women with noncyclic pain, migratory pain, and normal pelvic examinations are unlikely to benefit from surgery. Counseling syndrome. is important for abused women with chronic pelvic pain Question 31 A 69-year-old woman is evaluated for involuntary leakage of urine with coughing, sneezing, laughing, or when lifting heavy boxes at work. She has no dysuria, frequency, or urgency and she has no mobility problems. She is gravida 4, para 4, and underwent a total abdominal hysterectomy 20 years ago for uterine fibroids. She has type 2 diabetes mellitus. Medications are metformin and lisinopril. She has no known drug allergies. On physical examination, vital signs are normal. BMI is 31. There is bulging of the anterior vaginal wall when the patient is asked to cough, accompanied by leakage of urine. Bimanual examination is unremarkable. The remainder of her examination is normal. Laboratory studies show fasting plasma glucose level of 89 mg/dL (5.0 mmol/L) with hemoglobin A1c of 6.5%. Urinalysis is normal. Answer Choice Which of the following is the most appropriate treatment? A B C D Pelvic floor muscle training Prompted voiding Pubovaginal sling Tolterodine Answer Choice Which of the following is the most appropriate treatment? A B C D Pelvic floor muscle training Prompted voiding Pubovaginal sling Tolterodine Key Point and Education Objective Treat stress urinary incontinence Pelvic floor muscle training is first-line treatment for stress urinary incontinence. Explanation This patient has stress urinary incontinence and should receive pelvic floor muscle training (PFMT). Stress urinary incontinence, defined as loss of urine with physical activity, cough, or sneeze, is caused by sphincter incompetence. Findings on physical examination include weakened anterior or posterior vaginal wall support (cystocele or rectocele, respectively). PFMT is considered first-line therapy for urinary stress incontinence. In PFMT, women learn repetitive exercises (Kegel exercises) to strengthen the voluntary urethral sphincter and levator ani muscles. For PFMT to be effective, it is important that the patient learn to correctly contract her muscles without straining, which increases abdominal pressure. Each contraction is held for approximately 10 seconds, followed by an equal relaxation period. The number of repetitions should be increased weekly until the patient is performing 8 to 12 repetitions three times daily, every day or at least 3 to 4 days per week. In a systematic review of nonsurgical therapy, PFMT improved stress urinary incontinence episodes. Outcomes were even better when PFMT was combined with biofeedback and when skilled therapists directed the treatment. Explanation Prompted voiding is indicated in and is effective in patients with significant mobility or cognitive impairments that may hinder the patient's ability to reach the toilet in time, neither of which this patient has. Sling procedures are effective for moderate to severe stress incontinence, but surgery is usually reserved for patients who do not benefit from more conservative approaches, including behavioral or appropriate pharmacologic therapy. Tolterodine, a selective antimuscarinic anticholinergic medication, is most effective for patients with urge, rather than stress, incontinence. This patient does not experience the classic sense of urinary urgency with her incontinence episodes, and, therefore, tolterodine would not be an appropriate first choice. Urinary Incontinence Urinary Incontinence Therapy Begin nondrug therapy in all patients with urinary incontinence regardless of what other interventions may eventually be needed. Evaluate for other reversible factors contributing to symptoms, such as diuretics or poorly controlled diabetes. Oxybutynin and tolterodine provide minor relief of urge incontinence but are associated with side effects related to anticholinergic properties. Stress incontinence cannot be treated with medications. Topical estrogen helps women with stress incontinence and atrophic vaginitis. Pelvic floor muscle training and biofeedback is also effective for stress incontinence. Imipramine (not FDA approved for this indication) may offer some benefit for combined urge and stress incontinence, although anticholinergic side effects are a factor. Prompted urination (asking about incontinence, reminding patient to use the toilet, positive feedback for continence and toilet use) is effective for functional incontinence (inability to get to the toilet because mental or physical disability). Don't Be Tricked Do not prescribe systemic estrogen-progestin therapy because it can worsen stress and urge incontinence. Do not order urodynamic testing because outcomes are no better than those associated with management based on clinical evaluation alone. Test Yourself A 78-year-old woman has urinary urgency, nocturia, and urine loss with coughing and sneezing. Her medical history includes HF and glaucoma. ANSWER: The diagnosis is combined stress and urge incontinence. Begin pelvic muscle exercises and bladder training techniques. Imipramine is contraindicated because of its anticholinergic effects. Question 32 A 32-year-old woman presents for emergency department follow-up. She was seen 1 week ago for a facial laceration. She tells you she cannot remember the incident. She had a humeral fracture 1 year ago, and has had bruising on her arms and legs on several visits. History is significant for depression and recurrent urinary tract infection. Her only current medication is citalopram. Upon questioning about intimate partner violence, the patient admits that her husband often beats her. Physical examination is significant for normal vital signs; a healing, sutured, 4-cm laceration across the left zygomatic arch; and several 5to 6-cm ecchymoses on her upper extremities. Answer Choice Which of the following is the most appropriate next step in management? A Advise the patient to leave her current living situation immediately B Ask her to bring her husband to her next appointment C Assess her immediate safety and develop a safety plan D Report the husband to the police E Request psychiatry consultation Answer Choice Which of the following is the most appropriate next step in management? A Advise the patient to leave her current living situation immediately B Ask her to bring her husband to her next appointment C Assess her immediate safety and develop a safety plan D Report the husband to the police E Request psychiatry consultation Key Point and Education Objective Manage a patient who is a victim of intimate partner violence. The primary responsibility of the provider for a patient who is a victim of intimate partner violence is to assist with health; assess for safety; and provide validation, support, and empathy. Explanation The primary responsibility of the provider for a patient who is a victim of intimate partner violence is to assist with health; assess for safety; and provide validation, support, and empathy. Leaving the abuser is neither necessary nor recommended without a well thought-out plan unless the patient is in imminent danger, in which case immediate intervention is indicated. Advising victims of intimate partner violence to simply leave the situation, to utilize a shelter, contact an intimate partner violence counseling service, or press criminal charges is generally not helpful as the circumstances surrounding intimate partner abuse relationships are complex, and the abused individual may have significant reasons for not pursuing these actions that need to be understood. An appreciation of the individual circumstances in the context of a supportive relationship will help in developing a plan that may ultimately involve the use of these valuable resources. Explanation It is not recommended that the potential abuser be confronted directly or legal action be undertaken as an initial step in most cases as this may potentially put the victim in greater danger. Psychiatry intervention may be necessary for refractory depression, or when the patient is deemed a risk to harm herself or others. However, this would not be an appropriate next step in management of this patient. A substantial number of patients remain in adverse relationships yet demonstrate improved health and health outcomes after disclosure of their situation with appropriate support and management. Domestic Violence Diagnosis Physical and psychological domestic violence are associated with significant mental and physical health consequences for both male and female victims. Abuse frequently starts or increases during pregnancy. Characteristic findings: exacerbations or poor control of chronic medical conditions seeming nonadherence to medications abdominal pain sleep or appetite disturbances, fatigue, reduced concentration, or chronic pain depression, anxiety, acute or posttraumatic stress, somatization, and eating disorders suicide attempts and substance abuse frequent appointment changes STDs, HIV, unplanned pregnancies visible bruises or injuries Assess the risk of homicide, suicide, or serious injury. Inquire about: escalating threats or abuse and escalating level of fear stalking weapons, especially firearms, in the home sexual assault and abuse during pregnancy recent separation or abuser's awareness of impending separation Therapy Initiate safety planning. Determine if the patient wants to leave home, return home, or have the abuser removed from his or her household. Refer the patient to a domestic violence advocate. Question 33 A 75-year-old woman is evaluated during a follow-up examination for recently diagnosed symptomatic peripheral arterial disease. The patient has hypothyroidism, hypertension, atrial fibrillation, and smokes cigarettes (30-pack-year history). Her current medications are diltiazem, warfarin, hydrochlorothiazide, levothyroxine, calcium, and vitamin D. On physical examination, she is afebrile, blood pressure is 140/82 mm Hg, pulse rate is 66/min, and respiration rate is 12/min. BMI is 21. Posterior tibialis and dorsalis pedis pulses are diminished bilaterally (1+); the skin on the anterior aspect of the lower legs is shiny and hairless. Heart rhythm is irregularly irregular and without murmurs. Neurologic and musculoskeletal examinations are normal. Laboratory studies: Total cholesterol 238 mg/dL (6.16 mmol/L) HDL cholesterol 36 mg/dL (0.93 mmol/L) LDL cholesterol 165 mg/dL (4.27 mmol/L) Triglycerides 205 mg/dL (2.32 mmol/L) Serum creatinine 0.9 mg/dL (79.6 µmol/L) Answer Choice In addition to strongly recommending smoking cessation, which of the following is the safest treatment for this patient? A B C D Atorvastatin Pravastatin Rosuvastatin Simvastatin Answer Choice In addition to strongly recommending smoking cessation, which of the following is the safest treatment for this patient? A B C D Atorvastatin Pravastatin Rosuvastatin Simvastatin Key Point and Education Objective Treat elevated LDL cholesterol level In patients who require lipid-lowering therapy and who are taking multiple medications, a statin that is renally metabolized, such as pravastatin, has a lower risk of drug-drug interactions Explanation Pravastatin is the safest choice for lowering LDL cholesterol level in this patient. She has recently diagnosed peripheral arterial disease, which is associated with atherosclerosis; her goal LDL cholesterol level is, therefore, less than 100 mg/dL (2.59 mmol/L) . Pravastatin is one of the preferred statins in patients who are being treated with multiple medications. Statins should be considered first-line therapy for lowering LDL cholesterol levels in this patient, as studies have shown that older patients (ages 65-80 years) derive similar benefit as younger patients for secondary prevention of cardiovascular disease. However, advanced age is also a risk factor for statin-related myopathy, and therapy should be chosen carefully to minimize this risk. Female sex, small body frame, hypothyroidism, statin dosage, and treatment with multiple medications also influence the likelihood of developing statin-related myopathy. Pravastatin is metabolized by the kidneys; therefore, its concentration will be unaffected by cytochrome isoenzymes that affect the metabolism of other statins or warfarin. Explanation In contrast, atorvastatin, lovastatin, and simvastatin are primarily metabolized through the cytochrome P-450 3A4 isoenzyme, and treatment with these medications in combination with diltiazem can increase serum statin levels, placing the patient at higher risk for statin myopathy. These statins should not be combined with diltiazem in a patient who is at already high risk for statin-induced myopathy based on her age, small body frame, hypothyroidism, and multiple medications. Rosuvastatin and fluvastatin are metabolized through the cytochrome P-450 CYP2C9 isoenzyme, and would effectively lower this patient's LDL cholesterol level. However, rosuvastatin may affect the metabolism of warfarin, leading to an increased INR. Caution is therefore necessary when combining these medications, and this is not the safest choice for this patient. Question 34 A 30-year-old woman is evaluated for hyperlipidemia. Medical history is significant for type 1 diabetes mellitus, hypothyroidism, and hypertension. She is planning pregnancy. Her father was diagnosed with coronary artery disease at the age of 47 years. Her current medications are levothyroxine, hydrochlorothiazide, insulin glargine, and insulin aspart. On physical examination, vital signs and the remainder of the physical examination are normal. Laboratory studies: Hemoglobin A1c 8.1% Total cholesterol 223 mg/dL (5.78 mmol/L) HDL cholesterol 67 mg/dL (1.74 mmol/L) LDL cholesterol 140 mg/dL (3.63 mmol/L) Triglycerides 90 mg/dL (1.02 mmol/L) Answer Choice In addition to recommending therapeutic lifestyle changes, which of the following is the most appropriate management of this patient's lipid levels? A B C D Colesevelam Ezetimibe Gemfibrozil Simvastatin Answer Choice In addition to recommending therapeutic lifestyle changes, which of the following is the most appropriate management of this patient's lipid levels? A B C D Colesevelam Ezetimibe Gemfibrozil Simvastatin Key Point and Education Objective Treat hyperlipidemia in a woman who desires pregnancy. Bile acid sequestrants are an option for reducing LDL cholesterol levels in women with hyperlipidemia who wish to become pregnant. Explanation This patient should be started on colesevelam. She has several risk factors for cardiovascular disease, including poorly controlled diabetes mellitus, hypertension, dyslipidemia, and a family history of premature myocardial infarction. Her goal LDL cholesterol level is below 100 mg/dL (2.59 mmol/L).Therapeutic lifestyle changes, which include a low-saturated fat diet and at least 120 minutes of aerobic exercise weekly, will reduce LDL cholesterol levels by 7% to 15%. Thus, this patient needs additional therapy to achieve her LDL cholesterol goal. Ezetimibe is a cholesterol absorption inhibitor that can reduce LDL cholesterol levels by up to 19%. Treatment with ezetimibe has not been shown to have beneficial effects on cardiovascular morbidity or mortality. Moreover, ezetimibe is FDA pregnancy class X, and should be avoided in women who may become pregnant. Gemfibrozil is a fibric acid that is typically used for the treatment of hypertriglyceridemia. It reduces LDL cholesterol levels by 10% or less; in addition, gemfibrozil monotherapy in patients with hypertriglyceridemia can actually raise LDL cholesterol levels. Gemfibrozil is not contraindicated in pregnancy (FDA pregnancy class C) but would not be effective for achieving this patient's LDL cholesterol goal. Explanation Although statins (such as simvastatin) are typically the first-line treatment for lowering LDL cholesterol levels, statins are teratogenic (FDA pregnancy class X) and should be avoided in women who may be or wish to become pregnant. Colesevelam, which is a bile acid sequestrant that lowers LDL cholesterol levels by up to 18%, is the best initial treatment option for this patient. Colesevelam is FDA pregnancy class B and so is safe to use in premenopausal women who are sexually active. Bile acid sequestrants have been shown to reduce the risk of coronary heart disease in primary prevention trials. The most common side effects associated with bile acid sequestrants include constipation, abdominal pain and bloating, and flatulence. Bile acid sequestrants can bind to and reduce the absorption of other drugs; this effect can be minimized by administering the other drugs 1 hour before or 4 hours after taking a bile acid sequestrant. Question 24 A physician is asked to advise the Pharmacy and Therapeutics Committee of the hospital regarding a new drug to prevent deep venous thrombosis (DVT), drug “Z.” The physician reviews a recent randomized controlled trial of 5000 patients that compared drug Z with drug C, which is commonly used and is on the hospital's formulary.The following data are abstracted from the trial: Study results: Drug Drug Z (n = 2500) Drug C (n = 2500) DVT Cases 25 50 Answer Choice Based on these data, how many patients need to be treated (number needed to treat, NNT) with drug Z, compared with drug C, to prevent one extra case of DVT? A B C D E 1 2 25 100 167 Answer Choice Based on these data, how many patients need to be treated (number needed to treat, NNT) with drug Z, compared with drug C, to prevent one extra case of DVT? A B C D E 1 2 25 100 167 Explanation The number needed to treat (NNT) with drug Z compared with drug C to prevent one additional case of deep venous thrombosis (DVT) is 100. Absolute risk (AR) is the risk of a specific disease based on its actual occurrence, or its event rate (ER), in a group of patients being studied, and is expressed as: AR = (patients with event in group) / (total patients in group) As seen in the table, in this study, the AR for DVT in the group treated with drug Z is 25/2500, or 1%, and the AR for the group treated with drug C is 50/2500, or 2%. Often, the event rate of a disease in an experimental group (EER) is compared with the event rate in a control group (CER). When the risk between groups is reduced, this difference is termed the absolute risk reduction (ARR), or if the outcome is of benefit, the difference is called the absolute benefit index (ABI). In this case, patients treated with drug Z (EER) appear to benefit from treatment with a lower risk of DVT than patients in the group treated with drug C (CER). This is expressed as: ABI = | EER − CER | ABI = |1% − 2% | = 1% or 0.01 This means that treatment with drug Z benefits patients compared with drug C by lowering the risk of DVT from 2% to 1%, or an absolute difference of 1%. Explanation Assessing treatment studies using absolute measures also allows determination of “numbers needed,” which are estimates of the clinical magnitude of the differences between treatments. In this case, the NNT indicates the number of patients needed to be treated with drug Z, compared with drug C, to obtain one additional beneficial outcome. The NNT is calculated as: NNT = 1/ABI NNT = 1 ÷ 0.01 = 100 This means that 100 patients would need to be treated with drug Z compared with drug C in order to prevent one additional case of DVT. Treatment study results may also be reported as relative measures; these measures compare the ratio of two outcomes without regard to the actual frequency of the outcome in a given study population. In this case, treatment with drug Z leads to a 50% reduction in risk of DVT compared with treatment with drug C (25 compared with 50 events), even though the actual frequency of DVT in the study populations does not exceed 2%. Therefore, outcomes expressed in relative terms usually appear of greater magnitude than when expressed in absolute terms; they also do not allow calculations of number needed to estimate clinical impact. Biostatistics Sensitivity, Specificity, Predictive Values, and ROC Curves Sensitivity = (all true-positive test results) / (true-positive and false-negative test results). Remember SNout: Sensitive test that is Negative rules OUT disease. Specificity = (all true-negative results) / (true-negative and false-positive results). Remember SPin: Specific test that is Positive rules IN disease. PPV = (true-positive test results) / (all positive test results). PPV answers the question, “Given a positive test result, what is the probability the patient has the disease?” NPV = (true-negative test results) / (all negative test results). NPV answers the question, “Given a negative test result, what is the probability the patient does not have the disease?” A ROC curve is a graph of the sensitivity vs. (1 − specificity). In medicine, a ROC analysis provides tools to select tests with optimal performance characteristics. The cut-point with the best combined sensitivity and specificity will be closest to the upper left corner. The test with the greatest overall accuracy will have the largest area under the ROC graph. Don't Be Tricked As the prevalence of a condition increases, the PPV increases and the NPV decreases. Changes in prevalence do not alter the sensitivity or specificity. Likelihood Ratios The LR is a measurement of the odds of having a disease independent of the disease prevalence. You must first assess the patient's pretest probability of having a disease before applying the LR of the test/finding to calculate the posttest probability. Positive LR = (sensitivity) / (1 − specificity); negative LR = (1 − sensitivity) / (specificity). Positive LR answers the question, “How much more likely is a person to have the disease given a positive test result?” LRs of 2, 5, and 10 increase the probability of disease by approximately 15%, 30%, and 45%, respectively. LRs of 0.5, 0.2, and 0.1 decrease the probability of disease by approximately 15%, 30%, and 45%, respectively.