Pelvic Inflammatory Disease
advertisement

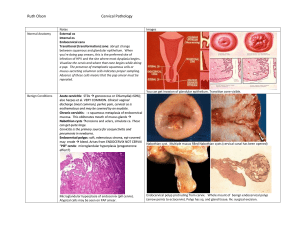
Delese LaCour M.D. Pediatric and Adolescent Gynecology Johns Hopkins Community Physicians January 29, 2010 Cervical Cancer Screening 1943 Papanicolaou and Trout published their monograph on the use of vaginal and cervical cytology as a screening tool for cervical neoplasm The incidence of cervical cancer has been reduced by 50% Cervical cancer has dropped from the #2 female cancer deaths to the 13th Types of Cervical Cancer Squamous cell Approximately 80-90% of cervical cancers Adenocarcinoma 10% Clear cell cervical cancer Mucinous adenocarcinoma Adenosquamous Glassy cell carcinoma Stromal sarcoma Sarcoma botryoides Leiomyosarcoma Lymphoma Small cell cervical cancer Adenoid cystic carcinoma of the cervix Technique for cervical cancer screening Collection Methods for Pap Smear Collection Methods for Pap Smear Bethesda System 2001 SPECIMEN ADEQUACY Satisfactory for evaluation (note presence/absence of endocervical/ transformation zone component) Unsatisfactory for evaluation . . . Specimen rejected/not processed Specimen processed and examined, but unsatisfactory for evaluation of epithelial abnormality because GENERAL CATEGORIZATION (Optional) Negative for intraepithelial lesion or malignancy Epithelial cell abnormality INTERPRETATION/RESULT Negative for Intraepithelial Lesion or Malignancy Organisms Trichomonas vaginalis , Fungal oganisms consistent with Candida species Shift in flora suggestive of bacterial vaginosis Bacteria consistent with Actinomyces species Cellular changes consistent with herpes simplex virus Other non-neoplastic findings Reactive cellular changes associated with inflammation radiation intrauterine contraceptive device Glandular cells status posthysterectomy Atrophy Bethesda System 2001 Epithelial Cell Abnormalities Squamous cell Atypical squamous cells (ASC) of undetermined significance (ASC-US) cannot exclude HSIL (ASC-H) Low-grade squamous intraepithelial lesion (LSIL) encompassing: human papillomavirus/mild dysplasia/cervical intraepithelial neoplasia (CIN) 1 High-grade squamous intraepithelial lesion (HSIL) moderate and severe dysplasia, carcinoma in situ; CIN 2 and CIN 3 Squamous cell carcinoma Glandular cell Atypical glandular cells (AGC) Atypical glandular cells, favor neoplastic Endocervical adenocarcinoma in situ (AIS) Adenocarcinoma Classification Terminology for Cervical Cytology: The 2001 Bethesda System Normal1 ASCUS2 LSIL3 HSIL3 Two types of atypical squamous cells (ASC)4 Atypical squamous cells of undetermined significance (ASCUS) Atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesions (ASC-H) Squamous intraepithelial lesions (SIL)4 Low-grade SIL (LSIL): Mild dysplasia, cervical intraepithelial neoplasia 1 (CIN 1) High-grade SIL (HSIL): Moderate and severe dysplasia, CIN 2/3, carcinoma in situ (CIS) 1. Spitzer M, Johnson C. Philadelphia, Pa: WB Saunders Co; 2002:41–72. Copyright © 2000 by WB Saunders Company. Reprinted with the permission of Elsevier. 2. Apgar BS, Zoschnick L. Am Fam Physician. 2003;68:1992–1998. Reprinted with the permission of the American Academy of Family Physicians. 3. Cannistra SA, Niloff JM. N Engl J Med. 1996;334:1030–1038. Images reproduced courtesy of Dr. Graziella Abu-Jawdeh. 4. Solomon D, Davey D, Kurman R, et al, for the Forum Group Members and the Bethesda 2001 Workshop. JAMA. 2002;287:2114–2119. Classification of Histological Findings: Cervical Intraepithelial Neoplasia Cervical intraepithelial neoplasia (CIN)1 CIN 1: Mild dysplasia; includes condyloma (anogenital warts) CIN 2: Moderate dysplasia CIN 3: Severe dysplasia; includes CIS CIN1 Normal CIN 1 (condyloma) CIN 1 (mild dysplasia) CIN 2 (moderate dysplasia) CIN 3 (severe dysplasia/CIS) Invasive Cancer Histology of squamous cervical epithelium1 Basal cell Basal membrane CIN caused by HPV can clear without treatment; however, rates of regression are dependent on grade of CIN.2 1. Bonnez W. In: Richman DD, Whitley RJ, Hayden FJ, eds. Washington, DC: American Society for Microbiology Press; 2002:557–596. Reprinted with the permission of the American Society for Microbiology Press. 2. Ostor AG. Int J Gynecol Pathol. 1993;12:186–192. Cervical cancer screening Cervical cancer screening should begin at age 21 A) High prevalence of HPV infection in teenagers B) Most dysplasia regresses spontaneously in adolescents C) Invasive cervical cancer is rare in those younger than 21 D) Potential for adverse effects of side effects American College of Obstetrics and Gynecology Practice Bulletin No 109, Dec 2009 High prevalence of HPV infection in teenagers Risk of Acquiring HPV After First Intercourse in Female Adolescents 70 Cumulative risk of cervical HPV infection in female adolescents with only 1 sexual partner Cumulative Risk of HPV (%) 60 50 40 30 20 10 0 0 12 24 36 48 60 Time Since First Intercourse (Months) From Collins S, Mazloomzadeh S, Winter H, et al. High incidence of cervical human papillomavirus infection in women during their first sexual relationship. Br J Obstet Gynaecol. 2002;109:96–98. Reprinted with the permission of the Royal College of Obstetricians and Gynaecologists. Projected Age-Specific Prevalence of HPV (Based on a Mathematical Model) 0.3 HPV LSIL HSIL Prevalence 0.25 0.2 0.15 0.1 0.05 0 15 25 35 45 55 65 75 Age From Myers ER, McCrory DC, Nanda K, Bastian L, Matchar DB. Mathematical model for the natural history of human papillomavirus infection and cervical carcinogenesis. Am J Epidemiol. 2000;151:1158–1171. Reprinted with the permission of Oxford University Press. HPV Infection in Female Adolescents1 81.6% infected with multiple types Mean number of HPV types per HPV-positive subject = 4.9 Of the 60 subjects, Pap smear results were available for 54. 37% had ≥1 abnormal result. Most severe Pap smear result for each individual subject (n=54) 70 63.0 60 Patients (%) Single-center study in 60 female adolescents (14–17 years of age) monitored over 2.2 years 81.7% cumulative prevalence (49/60) 50 40 30 16.7 20 18.5 10 1.9 0 Normal ASCUS 1. Brown DR, Shew ML, Qadadri B, et al. J Infect Dis. 2005;191:182–192. LSIL HSIL Prevalence of HPV Infection in Young Men Study Author, Year Baldwin, 2004*,1 N 393† Selected Age Range (Years) 18–24 HPV Prevalence (%) 34% Weaver, 20042 317 18–25 33% Svare, 2002*,3 44 18–24 48% Kataoka, 19914 108 18–23 29% *Conducted at a sexually transmitted disease clinic † Number includes all patients included in the study (18–70 years of age). 1. Baldwin SB, Wallace DR, Papenfuss MR, Abrahamsen M, Vaught LC, Giuliano AR. Sex Transm Dis. 2004;31:60:601–607. 2. Weaver BA, Feng Q, Holmes KK, et al. J Infect Dis. 2004;189:677–685. 3. Svare EI, Kjaer SK, Worm AM, Østerlind A, Meijer CJLM, van den Brule AJC. Sex Transm Infect. 2002;78:215–218. 4. Kataoka A, Claesson U, Hansson BG, Eriksson M, Lindh E. J Med Virol. 1991;33:159–164. Most dysplasia regresses spontaneously in adolescents A prospective study of 187 women aged 18-22 years old found that LSIL had reverted to negative in 61% after 1 year and 91% after 3 years Only 3% progressed to CIN 3 Two smaller studies of adolescent females with biopsy confirmed CIN 2 showed 65-75% regression after 18 months and 36 months ACOG practice bulletin 2009 Estimated Likelihood of Time to LSIL Regression in Adolescents In a study of women 13–22 years of age, there was a 91% probability of regression of LSIL cases within 36 months. The probability of progression to HSIL within this same time frame was 3%. 12-month regression rate = 61% Estimated Proportion With LSIL* 1.0 0.8 36-month regression rate = 91% 0.6 0.4 0.2 0 0 10 20 30 40 Months After Diagnosis 50 60 *The shaded area indicates point wise 95% CIs. From Moscicki A-B, Shiboski S, Hills NK, et al. Regression of low-grade squamous intra-epithelial lesions in young women. Lancet. 2004;364:1678–1683. Reprinted with the permission of Elsevier Ltd. Incidence and Progression of SIL and CIN 2/3 in Female Adolescents 1 N=602 18–20 years of age 0.9 Cumulative Incidence Cervical SIL Vaginal SIL CIN 2/3 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 0 4 8 12 16 20 24 28 Months 32 36 40 44 48 Time from detection of first incident HPV infection to progression of lesions From Winer RL, Kiviat NB, Hughes JP, et al. Development and duration of human papillomavirus lesions, after initial infection. J Infect Dis. 2005;191:731–738. Reprinted with the permission of the University of Chicago Press. Risk of Cervical Lesions and Cancer in Women Exposed to HPV at a Young Age1 Relative risks for CIN and invasive cancer increase with decreasing age of first sexual intercourse Relative Risk Estimates* 7 6 5 Age at First Intercourse (Years) ≥23 or Never 18–22 ≤17 4 3 2 1 0 CIN (n=206) Invasive Cervical Cancer (n=327) *Mantle-Haenszel estimates adjusted for age only 1. La Vecchia C, Franceschi S, DeCarli A, et al. Cancer. 1986;58:935–941. Invasive cervical cancer is rare in those younger than 21 Only 0.1 % of cervical cancers occur before age 21 National data from 1998 through 2003 identified 14 cases of invasive cancer /year in those ages 15-19 SEER 2002-2006 incidence rate of 1-2 cases per 1,000,000 females aged 15-19 (Surveillance Epidemiology and End Results) Pap Smear Abnormality Rates in Adolescent Versus Adult Women Simsir1 Edelman2 Pap Smear Abnormality Rates (%) 35 30 25 29 Adolescents (n=528) Adolescents (n=271) Adults (n=10,312) Total Population (n=29,295) P<0.0002 20.7 23 20 16 15 15 P=0.04 13 13.2 12.2 9.9 10 7 P=0.001 5 0.2 1.2 P=NR* 0 P<0.00001 7.7 2.5 0.1 0.7 0.6 P=NR* 0 0.2 HSIL Carcinoma 0 All Abnormal Results ASCUS LSIL HSIL SCC † All Abnormal Results ASCUS LSIL *NR = statistically significant but P value not reported †SCC = squamous cell carcinoma 1. Simsir A, Brooks S, Cochran L, Bourquin P, Ioffe OB. Acta Cytol. 2002;46:272–276. 2. Edelman M, Fox AS, Alderman EM, et al. Cancer. 1999;87:184–189. Comparative Incidence of CIN in Adolescent and Adult Women1 Annual Incidence per 1000 Women 6 15–19 years of age (n=6261) 5 20–24 years of age (n=1570) 25–29 years of age (n=2919) 4 3 2 1 0 CIN 1 CIN 2 1. Insinga RP, Glass AG, Rush BB. Am J Obstet Gynecol. 2004;191:105–113. CIN 3 Incidence of HPV Infection and LSIL in Female Adolescents and Young Women1 105 HPV-negative at baseline 496 with prevalent HPV infection 54 incident HPV infections 109 incident LSIL cases in HPV-positive subjects 70 HPV-Negative at Baseline 60 51 (54/105) HPV-Positive at Baseline 50 Incidence (%) Prospective cohort study of female adolescents and young women (13–21 years of age) with median follow-up of 50 months 40 30 19 (10/54) 20 22 (109/496) 10 0 HPV Infection 1. Moscicki A-B, Hills N, Shiboski S, et al. JAMA. 2001;285:2995–2002. LSIL LSIL Potential for adverse effects of side effects Significantly increased risk of : Preterm birth Low birth weight Neonatal intensive care admissions For every 18 LEEPs preformed there will be an additional preterm birth Suh-Burgmann B and Kinney W 2006 ASCCP Vol 10 , Issue 2,2006 Management of LGSIL Abnormal Pap ASCUS-H Management of HGSIL Abnormal Pap CIN1 Abnormal Pap CIN 2-3 How often to screen Frequency of cervical cytology screening Every 2 years for women aged 21-29 Women aged 30 or older with three consecutive negative pap smears can be followed every three years More frequent screening for HIV infected women Immunosuppressed women Women exposed to DES Women with previously treated CIN2, CIN 3 , or cancer How often to screen Frequency Women with HIV should be screened every 6 months in the first year of diagnosis, then every year Women treated in the past for CIN2, CIN3, or cancer are at risk for 20 years for recurrence or persistence, annual screening Special Notes The frequency of those with same sex partners Penetrative sex at an early age Same screening in those who have been vaccinated against HPV ( ACOG press release 11/09) Pelvic Inflammatory disease in pregnancy A 23 year old P2032 at 8 weeks and 6 /7 days presents to ER with complaint of nausea, vomiting, and abdominal pain Past Medical history : NC Past Surgical history : TAB x 3 Social history : positive marijuana use Gyn/OB history: new partner, history of Chlamydia, Trich, PID in past, SVD times two Vitals 37.0 , RR 20, P 65, BP 97/59 PE: moderate distress Abdomen soft, no rebound or guarding, Pelvic: Yellow vaginal discharge, cervical motion tenderness Sonogram: 8 week fetus with fetal HMS Pelvic Inflammatory disease in pregnancy Labs: WBC 4.9, Hct 39.9, Positive culture for chlamydia, Trich on wet prep Hospital course: pt was admitted with diagnosis of PID in pregnancy, Treated 48 hours with IV Gentamycin and Clindamycin , po Azithomycin Discharge Home with Clindamycin for ten days Pelvic Inflammatory Disease Most of the times multi-organism Can range from endometritis to pelvic abcesses 300,000 cases per year 16-20% in Adolescents Clinical diagnosis overestimated and difficult Pelvic Inflammatory Disease •Empiric treatment warranted if suspected because of long term effects if untreated •Begin treatment if sexually active and – Uterine tenderness –Adnexal tenderness – Cervical motion tenderness (CMT) Pelvic Inflammatory Disease Additional Criteria: Temp > 101 F (38.3 C) Mucopurulent cervical discharge WBC on microscopy Increased erythrocyte sedimentation rate Increased C-reactive protein Positive culture for N. gonorrhea or Chlamydia Pelvic Inflammatory Disease Treat in hospital if: Surgical emergency cannot be excluded Pregnancy (rare 1: 1000 to 1:25000) No initial clinical response Does not tolerate PO Severe illness Tubo-Ovarian abscess Pelvic Inflammatory Disease Rx. Outpatient: A: Ofloxacin 400 mg PO BID X 14 days OR Levofloxacin 500 mg PO QD X 14 days +/- Metronidazole 500 mg PO BID X 14 days B: Ceftriaxone 250 mg IM X 1 dose OR Cefoxitin 2 g IM X 1 dose + Probenecid 1 g PO OR Other third generation cephalosporin Plus Doxycycline 100 mg PO BID X 14 days +/- Metronidazole 500 mg PO BID X 14 days CDC STD treatment guidelines 2006 1-94 Pelvic Inflammatory Disease In House A: Cefotetan 2 g IV Q 12 OR Cefoxitin 2 g IV Q 6H Plus Doxycycline 100 mg IV or PO Q12 H B: Clindamycin 900 mg IV q8h Plus Gentamicin 2mg/kg loading f/u 1.5 mg/kg Q8H C: Ofloxacin 400 mg IV Q6h or Levofloxacin 500 mg QD +/- Metronidazole 500 mg IV Q8H or Unasyn 3 g IV Q6H Plus Doxycycline 100 mg PO IV Q12H CDC STD treatment guidelines 2006 1-94 Pelvic Inflammatory Disease Pregnancy: Multiple reports in the literature (1:1000-1:25000) Easily confused with ectopic pregnancy Associated with fetal wastage and poor outcomes Etiology confusing: Sperm carrying bacteria? Infection prior to 12 weeks and membrane apposition? Reactivation of latent disease? Hematogenous or Lymphatic spread? Lara-Torre E et al JRM 2002;47:959-61 Pelvic Inflammatory Disease Pregnancy (cont): Aggressive antibiotic treatment warranted prior to uterine evacuation Conservative treatment may maintain pregnancy to term Delay in diagnosis because of pregnancy may worsen outcomes Decrease immune response in pregnancy may worsen presentation and progression