Unit 4a * Almost done!
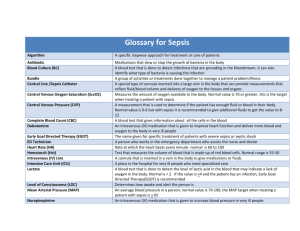
advertisement

Unit 4a – Almost done! Chapter 15: Microbial Mechanisms of Pathogenicity • How microbes cause disease (figure 15.9) Remember? • Pathogenicity: The ability to cause disease. • Virulence: The extent of pathogenicity. • Most pathogens have a preferred portal of entry • Salmonella typhi swallowed vs. rubbed • Strep pneumonia inhaled vs. swallowed Numbers of Invading Microbes • _____: Infectious dose for 50% of a sample population. • _____: Lethal dose (toxin) for 50% of a sample population. • actual number depends on: – virulence of pathogen – strength of host defenses • for same pathogen and same person, infective dosage varies from day to day with strength of body defenses Clickers… • What is the LD50 for the bacterial toxin tested in the experiment below? • Dilution mg/kg a. 6 b. 12.5 c. 25 d. 50 e. 100 # of animals that died 0 0 3 4 6 # of animals that survived 6 6 3 2 0 Adherence factors • for attachment to host cells attachment by capsule • Remember Unit 1 discussion of Biofilms? attachment by filaments attachment by hook attachment by viral spikes Virulence factors: how pathogens cause disease • Many pathogens have multiple virulence factors • Virulence factors have 5 general effects – adherence to host cells – entering into host cells – destruction of host cells – avoiding phagocytosis – evading immune responses Good Essay Question! Some exoenzymes of virulence • 1. collagenase: dissolves collagen (protein fibers in connective tissue); softens up a tissue so infection can spread – Clostridium’s spread of gas gangrene • 2. IgA proteases – Destroy our IgA antibodies – Gonorrhoea and meningococcal meningitis can do • 3. hyaluronidase: dissolves hyaluronic acid (gluelike substance that holds cells together); helps infection to spread – Streptococcus sp. hyaluronidase dissolving hyaluronic acid • 4. lecithinase: dissolves cell membranes; pathogen can digest cell contents enzymes of virulence • 5. coagulases: clot blood; fibrin fibers coat pathogen, prevent phagocytosis – Staph (to wall off boils) • 6. leukocidins: kill white blood cells – Staph aureus • 7. kinases: dissolve clots (e.g. streptokinase) • 8. hemolysins: cause hemolysis (lysis of red blood cells) – test for hemolysis on blood agar – alpha hemolysis: partial hemolysis, causes greenish zone around colony on blood agar – beta hemolysis: complete hemolysis, causes clear, colorless zone around colony – gamma hemolysis: NO hemolysis Other virulence factors • _________: prevents phagocytosis, helps pathogen attach to host cell Toxins • • • • Toxin: Substances that contribute to pathogenicity. Toxigenicity: Ability to produce a toxin. Toxemia: Presence of toxin in the host's blood. Antitoxin: Antibodies our body produces against a specific toxin. • Toxoid: Inactivated toxin used in a vaccine. – When toxoids are injected as a vaccine, they stimulate antitoxin production so that immunity is produced • Diphtheria and tetanus toxoid vaccination Exotoxins • Fig. 15.4 Endotoxins: Fig. 15.4 Endotoxins and the pyrogenic response figure 15.6 Sepsis and Septic Shock: pp. 639-641 (10th ed) • • • Although blood is normally sterile, if the defenses of the cardiovascular and lymphatic systems fail, microbes could enter blood/lymph Septicemia: proliferation of pathogens in the blood – Fever – Sometimes causes organ damage Sepsis: systemic inflammatory response syndrome (SIRS) – Mediators of inflammation into the blood stream – Fever – rapid heart or respiratory rates – High count of white blood cells – Lymphangitis: inflamed lymph vessels Fig. 23.2 Relationship between the cardiovascular and lymphatic systems Sepsis and Septic Shock continued • life-threatening systemic response to a bacterial infection • First stage is sepsis – Fever, chills and accelerated breathing & heart rate • Overwhelming infection leads to low blood pressure and low blood flow. – Shock • Vital organs, such as the brain, heart, kidneys, and liver may not function properly or may fail. Decreased urine output from kidney failure may be one symptom. – Severe sepsis to septic shock • Types – Gram-Negative Sepsis • Endotoxic shock • 750,000 cases/ yr in US; at least 225,000 are fatal (textbook pg. 640) – Gram-Positive Sepsis • Staph, Strep & Enterococcus – Puerperal Sepsis • Childbirth fever • Nosocomial infection • Strep. pyogenes most frequent cause • high risk patients: – Burns – Age >60 or the very young – post-surgery (especially intestinal) – abdominal trauma – advanced cancer – diabetes septic shock • mechanism: pathogens release endotoxins, exotoxins: • these products stimulate release of chemicals from various host cells that produce the symptoms: – – – – – low blood pressure, especially when standing rapid, weak pulse fever (hypothermia in burn patients) Low urine output Agitation, confusion septic shock • symptoms: – sudden high fever – disorientation, confusion, irritability, somnolence – edema (swelling): face, hands, feet – dyspnea • edema may constrict pharynx • bronchioles contract • death by asphyxiation may result – circulatory stagnation • inadequate blood volume causes low blood pressure, rapid weak pulse, possible total stagnation of bloodflow septic shock • treatment (not necessarily in this order) – – – – – inject epinephrine open airway (intubation or tracheostomy) oxygen if needed restore blood volume: rapid IV draw blood for blood gases and to culture pathogen – broad spectrum drug (until pathogen is known) – monoclonal antibodies against endotoxin Back to figure 15.9 In summary: Damage to host cells • 1. By using the host’s nutrients – Siderophores: proteins pathogens produce to get the iron they need from the host • 2. By causing direct damage in the immediate vicinity of the invasion • 3. By producing toxins Portals of Exit Respiratory tract Coughing and sneezing Gastrointestinal tract Feces and saliva Genitourinary tract Urine and vaginal secretions Skin Blood Biting arthropods and needles or syringes