1 Micro TA Review
advertisement

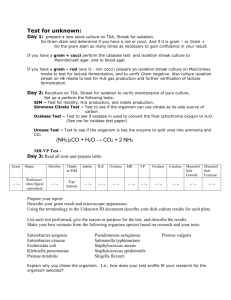
Micro TA Review 1 April 4, 2013 • Tips & hints • Memorization… this is the time! • Flashcards, stories, whatever it takes. • You really do need to know this. • Pathogen clinical presentation & vice versa • Questions: know all the answers • It goes fast – try to keep up as best you can! • Resources • Clinical Micro Made Ridiculously Simple • Lippincott Micro Cards • TA PPTs • Firecracker Bacterial Cell Walls Bacterial Genetics TRANSFORMATION: Ability to take up naked DNA of RELATED bacteria from environment (especially S. pneumo, H. influenzae, and Neisseria -- SHiN) TRANSPOSITION: Segments of DNA that can “jump” from one chromosomal location to another via excision and reincorporation. Can also jump from chromosome to plasmid and vice versa. TRANSDUCTION: Bacteriophage (virus that infects bacteria) transfers bacterial DNA from one bacteria to another. Can be generalized (lytic phage) or specialized (lysogenic phage). Bacterial Genetics CONJUGATION: “Bacterial Sex”– may involve UNRELATED bacteria, requires direct contact and transfer is UNIDIRECTIONAL. Two options: 1. F+ x F-: F plasmid contains genes for conjugation and it is transferred via pilus (no transfer of chromosomal genes). 2. Hfr x F-: F plasmid can become incorporated into DNA -- now called an Hfr cell and now may transfer plasmid + some flanking chromosomal genes. Normal Bacterial Flora • Skin: – Normal: Staphylococcus epidermidis – Transient: S. aureus • Upper Respiratory tract – Normal: Anaerobic cocci, Viridans Streptococci – Transient: Neisseria spp., Streptococcus pneumoniae, Haemophilus influenzae • Gastrointestinal Tract – Anaerobic GNR (Bacteroides), Enterobacteriaceae (E. coli), Enterococci • Genitourinary tract – Normal: Lactobacillus – Transient: GBS Virulence Factors • Ability to block arms of immune system (phagocytosis, antibodies, complement) (Staph aureus- Protein A; Strep pyogenes- M protein) • Slime and biofilms (Staph epi, Strep viridans) • Toxins (endotoxin vs. exotoxin) (Endotoxin: gram negatives; Exotoxin: Staph aureus, Strep pyogenes) • Adhesion (Staph sapro) • Flagella • Ability to survive phagocytosis (Strep pyogenes, hyaluronic acid capsule) • Ability to survive in hostile environments Exotoxin v. Endotoxin Superantigens Definition: • Superantigen toxins allow the non-specific binding of MHC II with T cell receptors, resulting in polyclonal T cell activation (versus other toxins, which are just monoclonal activation so not as intense). • Polyclonal T-cell population cytokine storm multisystem disease and shock. Examples: • S. aureus: TSST-1 • S. pyogenes: Exotoxin A Antibiotic Targets Antibiotic Classes Cell Wall Synthesis Inhibitors: Peptidoglycan Cross-Linking Penicillins, Cephalosporins, Carbapenems (Beta-Lactams) • Mechanism: bind to transpeptidases (aka PBP) → inhibit cross-linking of peptidoglycan no cell wall death by osmolysis • Resistance via beta lactamases, altered penicillin binding protein, altered porins. Cell Wall Synthesis Inhibitors: Peptidoglycan Synthesis Vancomycin • Mechanism: binds D-ala D-ala portion of cell wall precursors inhibits peptidoglycan synthesis. • Resistance via amino acid change from D-ala D-ala to D-ala D-lac; gramnegatives are intrinsically resistant because vanco can’t cross outer membrane. Protein Synthesis Inhibitors Macrolides, Tetracyclines, Aminoglycosides Inhibitors of DNA Polymerase Activity Fluoroquinolones, Metronidazole Folic Acid Synthesis Inhibitors Sulfonamides and Trimethoprim (TMP/SMX) OVERVIEW! Do not be overwhelmed. this week’s focus: gram+ cocci Gram Positive Cocci Also see the table in your lab manual! Types of Hemolysis Also: Staph aureus, GBS Also: Strep viridans Enterococci have variable hemolysis Staphylococcus aureus IN THE LAB • Gram + cocci in clusters • Coagulase +, catalase + • Beta-hemolytic cluster of grapes EPIDEMIOLOGY • Nosocomial and community, all ages CLINICAL • Pyogenic skin infxn (impetigo, cellulitis, abscesses) • Acute endocarditis (v. S. viridans subacute) • Osteomyelitis • Septic arthritis • Toxin-related syndromes (see below) scalded skin impetigo VIRULENCE FACTORS • Protein A, biofilm, capsule, coagulase, catalase, hemolysins, penicillinase • Toxins: TSST-1 (superantigen, causes Toxic Shock Syndrome); enterotoxin (preformed superantigen, causes gastroenteritis); exfoliative toxin (causes scalded skin syndrome) TREATMENT • Most strains secrete penicillinase MSSA, treat with nafcillin • Some strains alter the PBP MRSA, treat with vancomycin Staphylococcus epidermidis IN THE LAB Gram + cocci in clusters Coagulase - (vs S. aureus), catalase +, novobiocin sensitive (vs S. sapro) Gamma-hemolytic • • • EPIDEMIOLOGY Nl. flora of the skin; nosocomial & iatrogenic • CLINICAL Foreign body or device infxns (think prosthetics, IV lines, Foley catheters) Common contaminant in blood cultures • • VIRULENCE FACTORS Biofilm: extracellular scaffold that mediates attachment to foreign devices • TREATMENT Vancomycin & remove the infectious source (i.e., remove the device) • Staphylococcus saprophyticus IN THE LAB Gram + cocci in clusters Coagulase - (vs S. aureus), catalase +, novobiocin resistant (vs S. epi) Gamma-hemolytic • • • EPIDEMIOLOGY Sexually active women 2nd most common cause of UTI (1st is E. coli) • CLINICAL UTI (burning, urgency, frequency) • VIRULENCE FACTORS Specialized mucosal receptors • TREATMENT Folic acid synthesis inhibitors (TMP/SMX) • Streptococcus pyogenes (GAS) IN THE LAB • Gram + cocci in chains • Catalase – (vs Staphs), bacitracin sensitive (vs GBS) • Beta-hemolytic EPIDEMIOLOGY • All ages strep throat w/oropharyngeal petechiae CLINICAL • Suppurative (bc of host neutrophil response): pharyngitis (“strep throat”), cellulitis (inc. erysipelas), impetigo, necrotizing fasciitis • Non-suppurative (toxigenic): scarlet fever, Streptococcal Toxic Shock Syndrome • Delayed (immunologic): rheumatic fever, poststreptococcal glomerulonephritis VIRULENCE FACTORS • M protein, superantigen, streptolysin S & O, streptokinase, SpeA, B, C, anti-C5a peptidase, hyaluronidase (in capsule), T antigen, DNAase • Diagnose recent infxn with ASO titers (antistreptolysin O) TREATMENT • Penicillin Streptococcus agalactiae Streptococcus agalactiae (GBS) IN THE LAB • Gram + cocci in chains • Catalase – (vs Staphs), bacitracin resistant (vs S. pyogenes) • Beta-hemolytic EPIDEMIOLOGY • Neonates, peripartum women, diabetics CLINICAL • Neonatal sepsis, pneumonia, meningitis • Maternal sepsis • Less commonly: UTI, endocarditis VIRULENCE FACTORS • Not important TREATMENT/PROPHYLAXIS • Beta-lactams (penicillin) Group B is Bad for Babies! Enterococcus Enterococcus (E. faecalis, E. faecium) IN THE LAB • Gram + cocci in pairs or chains • Catalase – (vs Staphs) • Variable hemolysis (alpha or gamma) • Subdivided into Lancefield Group D and non-Lancefield Group D depending on carbs in cell wall EPIDEMIOLOGY • Nl GI flora; nosocomial infxn (esp VRE) CLINICAL • UTI, subacute endocarditis, biliary tract infxn • Peritonitis • Nosociomal superinfxn bacteremia VIRULENCE FACTORS • Dextran (glycocalyx) helps bind to heart valves TREATMENT • Inherent antibiotic resistance to cephalosporins • Now have vancomycin resistance as well (VRE) treat with daptomycin or ampicillin + aminoglycoside Strep viridans (S. mutans, S. sanguis) IN THE LAB • Gram + cocci in chains • Catalase – (vs Staphs), optochin resistant (versus S. pneumo) • Alpha-hemolytic EPIDEMIOLOGY • Nl oropharynx flora CLINICAL • S. mutans dental caries (cavities) • S. sanguis subacute bacterial endocarditis (heart valve damage) VIRULENCE FACTORS • Dextran (glycocalyx) helps bind to heart valves TREATMENT • Penicillin (usually sensitive to lotsa antibiotics) foliage growing on mitral valve from oral cavity Streptococcus pneumoniae IN THE LAB • Gram + lancet-shaped cocci in pairs (“diplococci”) • Catalase – (vs Staphs), optochin sensitive (versus S. viridans) • Alpha-hemolytic EPIDEMIOLOGY • See later lectures CLINICAL • Most common cause of MOPS: bacterial Meningitis in kids & elderly, Otitis media in kids, community-acquired Pneumonia, Sinusitis. • Also, sepsis. VIRULENCE FACTORS • Polysaccharide capsule prevents phagocytosis. • Diagnose with Quellung reaction (capsular “swellung”) TREATMENT • Penicillin • Some resistance high dose penicillin & cephalosporins • Lotsa resistance vancomycin