The Skeletal System: Bone Tissue
advertisement

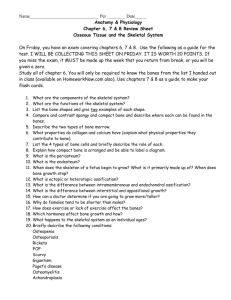
The Skeletal System: Bone Tissue Chapter 6 Functions of Bone and the Skeletal System • • • • • Support Protection Assistance in Movement Mineral Homeostasis Blood Cell Production – Red bone marrow – Hemopoiesis – hemo = blood, poiesis = making • Triglyceride Storage – Yellow bone marrow Parts of a Long Bone • Diaphysis = growing between – shaft • Epiphyses = growing over – distal and proximal ends • Metaphyses – meta = between – region where the diaphysis joins the epiphyeses • Articular cartilage - hyaline cartilage – covers epiphyses Parts of a Long Bone continued… • Periosteum – peri = around – surrounds the remainder of the bone surface • Medullary cavity – medulla = marrow – space within the diaphysis • Endosteum – endo = within – Lines the medullary cavity – Single layer of bone forming cells Bone Matrix • 25% water • 25% collagen fibers – provide tensile strength and flexibility • 50% crystallized mineral salts – provides hardness – Mainly hydroxyapatite (calcium phosphate and calcium carbonate) • A framework is created by the collagen fibers and the mineral salts are deposited into this framework • Osteoblasts initiate calcification Type of Cells in Bone Tissue • Osteogenic cells – Unspecialized cells from the mesenchyme • Osteoblasts – They become trapped in their secretions and become osteocytes • Osteocytes – mature bone cell • Osteoclasts – Resorption Types of Cells in Bone Tissue Compact Vs. Spongy Bone • Bone is not completely solid • There are spaces between cells and the matrix components • The spaces are channels for blood vessels • The size and distribution of the spaces determines whether it is compact bone (80%) or spongy bone (20%). Compact Bone • Contains few spaces • External layer of all bones and the bulk of the diaphysis • Provides protection and support • Resists the stresses produced by weight and movement Histology of Compact Bone • Arranged in units called osteons (Haversian Systems) • Perforating (Volkmann’s canals) – passage of blood vessels, lymph vessels and nerves • Connect with the central (Haversian) canals • Concentric lamallae – rings of hard calcified matrix • Lacunae = little lakes – lie between lamallae – Contain osteocytes • Canaliculi = small channels – Contain processes of osteocytes Bone Deposition • Osteons in compact bone are aligned in the same direction along lines of stress • The lines of stress can change – Fracture and deformity – Weight training – When a person learns to walk • Wolfe’s law Histology of Spongy Bone • Spongy bone does not contain osteons • Contains trabeculae – irregular latticework of thin columns of bone • Red Bone Marrow fills the spaces • Bone tissue in short, flat, or irregular bones • Epiphyses of long bones • Spongy bone is light • The spongy bone of the hip bones, ribs, breastbone, backbones, and the ends of long bones is the only site of red bone marrow in adults Bone Scan • Radioactive tracer is injected intravenously • The degree of uptake depends upon the amount of blood flow • Normal bone appears as gray in color with uniform uptake of the tracer • Darker or lighter areas suggest abnormalities • Dark areas “hot spots” – increased metabolism – Bone cancer, healing fractures, abnormal bone growth • Light areas “cold spots” – decreased metabolism – Degenerative bone disease, decalcified bone, fractures, bone infection, Paget’s, RA Paget’s Disease Paget’s Disease Blood and Nerve Supply • Bone is richly supplied with blood. • Blood vessels are particularly abundant in the portions of bone containing bone marrow. • They enter through the periosteum • Nerves accompany the blood vessels that supply the bones – rich in sensory nerves Blood Supply • • • • Periosteal arteries / veins Nutrient artery / vein Metaphyseal arteries / veins Epiphyseal arteries / veins Bone Formation • Ossification – ossi = bone, fication = making • Osteogenesis • Intramembranous ossification – Bone forms directly on or within loose fibrous CT • Endochondral ossification – Bone forms within hyaline cartilage Intramembranous Ossification • Development of the center of ossification – Mesenchymal cells cluster and differentiate – First forming osteogenic cells, then osteoblasts – Secrete organic matrix • Calcification – Minerals salts are deposited into the matrix • Formation of trabeculae – Forms spongy bone • Development of the periosteum – At the periphery of the bone the mesenchyme condenses – Forms a thin layer of compact bone Endochondral Ossification • Development of the cartilage model – Chondroblasts secrete cartilage matrix (hyaline) • Growth of the cartilage model – Interstitial growth - length – Appositional growth - thickness • Development of the primary ossification center – A region where bone tissue will replace most cartilage • Development of the secondary ossification center • Formation of articular cartilage and the epiphyseal plate – lengthwise growth in the adult Bone Growth • Bones throughout the body grow in thickness by appositional growth. • Long bones lengthen by the addition of material to the epiphyseal plate • Bones stop growing in length at about 25, although they may continue to thicken. Growth in Length • Epiphyseal plate – layer of hyaline cartilage in the metaphysis of a growing bone • 4 zones – Zone of resting cartilage – Zone of proliferating cartilage – Zone of hypertrophic cartilage – Zone of calcified cartilage Epiphyseal Line • The epiphyseal plates close between the ages of 18 and 25. • The cells of the plate stop dividing and bone replaces the cartilage • As the plate fades a bony structure called the epiphyseal line is left behind. • This signifies that the bone has stopped growing Growth in Thickness • Appositional growth – bone grows in thickness and diameter by this method • New bone tissue is being deposited on the outer surface of the bone and the lining of the medullary cavity is being resorbed, thus enlarging the meduallary cavity. Factors Affecting Bone Growth • Vitamins and Minerals – Calcium and Phosphorous – Flouride, magnesium, iron, manganese – Vitamins C, K, B12, and A • Hormones – – – – – Insulinlike growth factors (IGFs) Human Growth Hormone (hGH) Thyroid hormones (T3 and T4) Insulin Sex Steroids • Estrogens (produced by ovaries) • Adrogens (produced by testes) Hormonal Abnormalities • Oversecretion of hGH in childhood produces gigantism • Oversecretion of hGH in adulthood produces acromegaly • Undersecretion of hGH in childhood produces short stature • Men and Women who lack estrogen grow taller than normal (estrogen terminates growth at the epiphyseal plates) Gigantism Acromegaly Bone Remodeling • • • • • • • • Ongoing process Osteoclasts carve out small tunnels Osteoblasts build bone tissue Response to stress Healing of fracture sites 2-4 months Bone Resoprtion – osteoclasts break down matrix Weak bones / bone spurs (homeostasis is disrupted) Types of Fractures • • • • • • • Open (compound) fracture Closed (simple) fracture Comminuted fracture Greenstick fracture Impacted fracture Pott’s fracture Colle’s fracture Stress Fracture • A bone fracture without physically breaking • Due to repeated strenuous activities Repair of Bone • • • • Formation of a fracture hematoma Fibrocartilaginous callus formation Bony callus formation Bone remodeling Treatments for Bone Fractures • Realignment of the bone fragments – Closed – skin remains intact – manual manipulation – Open – surgical procedure • Screws, plates, pins, rods, and wires are used • Immobilization to maintain alignment – Cast, sling, splint, elastic bandage, external fixation device • Restoration of function – rehabilitation Bone and Calcium Homeostasis • Bone serves as a major calcium reservoir • Parathyroid hormone (PTH) regulates Ca2+ exchange between bone and blood • PTH decreases kidney loss of Ca2+ and stimulates the formation of calcitrol which helps the GI tract absorb Ca2+ • Calcitonin inhibits osteoclasts, speeds up blood uptake of Ca2+ by bone, and facilitates Ca2+ deposition Exercise and Bone Tissue • Bone responds to the level of stress placed upon it. • Wolfe’s law – Increased stress leads to increased bone deposition – Decreased stress leads to bone loss • Immobilzed bones can lose up to 1% per week. • Weight bearing exercise – Weight training – Incline 11 degrees or greater • Deposition until age 35 Effects of Aging • Loss of bone mass – demineralization • Brittleness – Decreased rate of protein synthesis Osteoarthritis • Degeneration of articular cartilage such that bony ends touch Osteogenic Sarcoma • Bone cancer that primarily effects teenagers, most often during their growth spurt. • Often metastasizes to the lungs. Osteomyelitis • Infection of the bone. • Fever, sweating, chills, pain, nausea, pus formation, edema, warmth • Bacteria (Staphylococcus aureus) usually causes it Rickets and Osteomalacia • Bones fail to calcify • Bones are “soft and rubbery” • Rickets affects the growth plates of children – Bowed legs, deformities of the skull and rib cage • Osteomalacia is a condition in adults – Brittle bones • Both are due to insufficient Vitamin D intake Rickets Osteopenia • Reduced bone mass • Osteoporosis is an example