ppt - Department of Mathematics
advertisement

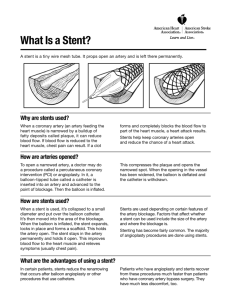
Collaborative Research: Modeling the Growth and Adhesion of Auricular Chondrocytes under Controlled Flow Conditions 1 Houston , Department of Mathematics, University of The Texas Heart Institute and the UT Health 2 3 Science Center at Houston , Baylor College of Medicine and Rice University 1 Canic , 1 Glowinski , 1 Pan , Suncica Roland Tsorng-When Doreen DMS-0443826 (UH), DMS-0443549(THI), DMS-0443563(Baylor) 2 Rosenstrauch , 3 Hartley (PIs) Craig www.math.uh.edu/~canic/NIGMS.html RESULTS: Coronary artery disease causes narrowing or METHODS: To investigate and optimize coating of stents stenosis of coronary arteries which might lead to heart attack. Treatment of coronary artery disease involves inserting a vascular stent into the diseased artery to keep the artery open thereby securing blood supply to the heart muscle. by auricular chondrocytes we have been working on the development of a fluid-structure-cell interaction algorithm. The aim is to mathematically and computationally simulate the growth, adhesion, detachment and long-term behavior of auricular chondrocytes under controlled flow conditions. Two algorithms: a fluid-structure interaction algorithm (Figure 3 top) and an algorithm simulating cell deposition and attachment to artificial surfaces (Figure 3 bottom) have already been developed, and a comparison with experiment showed good agreement. Figure 1. Vascular stent and restenosis. (Click on the picture to run the movie.) Upon implantation, vascular stents have been shown to activate inflammatory responses due to their poor biocompatibility. To improve biocompatibility of implantable cardiovascular devices, our group showed that lining stents with ear cartilage cells called auricular chondrocytes, might produce a long-lasting biocompatible device. Chondrocytes were genetically modified to produce nitric oxide which is known to have an antiinflammatory action. They were shown to exhibit superior adherance to artificial surfaces such as those of stents, shown in Figure 2. Figure 2. Stent struts lined with auricular chondrocytes: before expansion of stent (left), after expansion (right) (Wire filament width is 200 microns). Figure 3 Computational simulation:blood flow-stent interaction (top), cell rolling and detachment (bottom). (Click on the picture to run the movies.) WHY IT MATTERS: Heart attack is the single leading cause of death in the United States. Design of long-lasting biocompatible stents used in the treatment of coronary artery disease might lower the heart attack rates and improve the health of heart patients. Collaborative Research: Modeling the Growth and Adhesion of Auricular Chondrocytes under Controlled Flow Conditions OUTLOOK: Although a first generation fluid-structure PUBLICATIONS (selected): interaction algorithm and a fluid-cell interaction algorithm have been developed by our group, the coupling between the two algorithms is yet to be investigated. Simultaneously, we have been working on the set up of the flow loop, shown in Figure 4, for experimental testing of the vascular stent dynamics and cell slough off under controlled (pulsatile) flow conditions. The flow loop will be used to validate the mathematical and computational algorithm. Once the computational algorithm is experimentally validated, it will be used as a guide to optimal design of coated stents allowing different stent geometries and different artificial surfaces. For a complete list of publications please visit www.math.uh.edu/~canic/NIGMS.html • S. Canic, J. Tambaca, G. Guidoboni, A. Mikelic, C.J. Hartley, D. Rosenstrauch. Modeling viscoelastic behavior of arterial walls and their interaction with pulsatile blood flow. SIAM J Applied Mathematics Vol. 67 (2006). • R. Glowinski, G. Guidoboni, T-W Pan, "Wall-driven incompressible viscous flow in a two-dimensional semi-circular cavity", Journal of Computational Physics. To appear (2006). • S. Canic, C.J. Hartley, D. Rosenstrauch, J. Tambaca, G. Guidoboni, A. Mikelic. Blood Flow in Compliant Arteries: An Effective Viscoelastic Reduced Model, Numerics and Experimental Validation. Annals of Biomedical Engineering. 34 (2006), pp. 575 – 592. • S. Canic, Z. Krajcer, and S. Lapin. Design of Optimal Prostheses Using Mathematical Modeling. Endovascular Today (Cover Story). (2006) 48-50. •T.-W. Pan and R. Glowinski, Numerical Simulation of Pattern Formation in a Rotating Suspension of non-Brownian Settling Particles, in Free and Moving Boundaries: Analysis, Simulation and Control, Glowinski and Zolesio eds., Lecture Notes in Pure and Applied Mathematics, Vol. 252, Taylor & Francis/CRC Press, Boca Raton, FL, 2006 . Figure 4.. Experimental flow-loop set up. •S. Canic, A. Mikelic and J. Tambaca. A two-dimensional effective model describing fluid-structure interaction in blood flow: analysis, simulation and experimental validation Comptes Rendus Mechanique Acad. Sci. Paris 333(12) 867-883. (2005). PIs, Collaborators and Students: S. Canic, T.-W. Pan, R. *Received US Congressional Recognition for The Best Women in Technology Award (Houston 2005) (awarded to PI Canic) *SIAM 2004 von Karman Prize (awarded to Glowinski) *Glowinski elected to the French National Academy of Sciences in 2005 Glowinski (UH), D. Rosenstrauch (UTMCH&THI), C. Hartley (Baylor) PIs; G. Guidoboni (UH), A. Mikelic (France), J. Tambaca (Croatia), D. Mirkovic (MD Anderson Cancer Center), Z. Krajcer (THI), S. Lapin (UH) Collaborators; M. Kosor, T. Kim, J. Hao, T. Wang, B. Stanley (UH), K. Moncivais, T. Joseph, J. Gill (Rice) Students. Thanks: Mia Mirkovic for help with poster.