Predicting Pneumonia risk in patients with dysphagia
advertisement

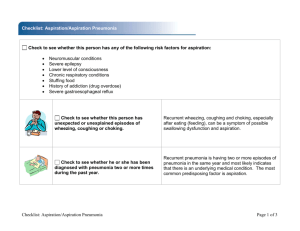
Evaluation and Management of Dysphagia a Team Approach Rebecca L. Gould, MSC, CCC-SLP rebec26050@aol.com (561) 833-2090 www.med-speech.com “More than 15 million Americans have some degree of dysphagia, and with regular treatment 83% recover or significantly improve”. Bello, J. (1994) compiled by Communication Facts. ASHA Research Division RLG Pneumonia occurs in 38% of all stroke victims and is the most common respiratory complication. Pneumonia contributes to about 34% of all stroke deaths and represents the third cause of mortality in the first month following stroke. Stepphens & Addington, 1999 RLG “IS IT SAFE TO FEED THIS PATIENT?” RLG EVALUATION Clinical “bedside” swallow evaluation. Videofluoroscopic Swallowing Study (VFSS) Fiberoptic Endoscopic Evaluation of Swallowing (FEES) (Reflexive cough test) RLG MBSS? or FEES? RLG Two Goals of Swallowing Evaluation: 1. Determine the Safest and Least Restrictive Level of P.O. 2. Determine the physiologic breakdown of the swallow so it can be rehabilitated in treatment. RLG FEES (Fiberoptic Endoscopic Evaluation of Swallowing) RLG RLG RLG RLG RESIDUAL Leftover material in the oral pharynx after swallow has occurred. RLG PENETRATION Entry of material into the laryngeal vestibule to the level of the vocal folds. RLG ASPIRATION Entry of material below the level of true vocal folds. RLG RLG RLG RLG RLG RLG RLG RLG RLG Assess secretions RLG Leder, Sasaki, Burrell (1998) FEES/Fluoro Comparison, n = 56 96% Agreement: 1 silently aspirated during MBS but coughed during FEES 1 did not aspirate during MBSS but did during FEES RLG Will Test ALL Types of Food/Liquid Thin liquid Thick liquid (Nectar) Puree Solid Mixed Consistency Pills Challenging food (i.e. nuts, peanuts, etc.) RLG Will give MULTIPLE trials of each consistency CPG can break down Large bolus size Consistency Fatigue Lack of coordination (COPD) RLG Protocol Saliva – Secretion rating Anatomy screen Laryngeal physiology assessment Swallowing physiology assessment Functional – Patient self-administer bolus Diet recommendations Recommendations for swallowing therapy/follow-up RLG Typically use green food coloring FEES Interpretation 4 Main Parameters: Delay in Swallow Initiation Penetration Aspiration Residue RLG RLG Swallow Initiation Bolus spills to valleculae or pyriform sinuses for greater than one second before the swallow (white-out). RLG RLG RLG RLG Penetration/Aspiration RLG RLG Timing of Penetration/Aspiration Before the Swallow During the Swallow After the Swallow RLG Issues With Residue Residue in Vallecula? Residue in Pyriform Sinuses? Diffuse Pharyngeal Residue? RLG RLG RLG RLG RLG RLG RLG Zenker’s Diverticulum RLG RLG Cervical Osteophytes Cervical Osteophytes RLG Globus RLG In General FEES = better detector of role of anatomy on swallowing physiology, aspiration, and appropriate diet ModBASW = better detector of role of UES and esophagus on pharyngeal function RLG Gurgly vocal quality predictive of who will aspirate on VFSS Linden (1993) RLG Incidence and patient characteristics associated with silent aspiration in the acute care setting 1001 patients underwent videoflurographic evaluation of their swallowing during a 2-year period: 469 aspirated 276 were silent aspirating Coughing is a physiologic response to aspiration in normal healthy individuals. No cough in response to aspiration silent aspiration Smith, C.H. et al (1999) RLG Aspiration risk after acute stroke: Comparison of clinical examination and Fiberoptic Evaluation of Swallowing Conclude: Clinical exam underestimated aspiration risk. FEES accurately assessed. 19 correct identification of aspiration risk 3 incorrect identification of aspiration risk 19 incorrect identification of aspiration risk 8 correct identification of no aspiration risk Leder, S.B. et al (2002) RLG 14% false negative rate – most important 20% false negative rate for VFSS 0% false negative rate for endoscopy “Fallacy to rely on bedside evaluation when instrumentation is possible” Aviv, J.E. (1997) RLG Oropharyngeal secretions and swallowing frequency in predicting aspiration Presence rated with endoscopic view. Scale 0, 1, 2, 3, Strong association between the presence of oropharyngeal secretions in the laryngeal vestibule and the likelihood of aspiration of food or liquid. Patients who demonstrate trouble in clearing oropharyngeal secretions for whatever reason will also demonstrate the same trouble with food or liquid while swallowing. J. Murray et al. (1996) RLG Oropharyngeal secretions and swallowing frequency in predicting aspiration (cont’d) Significant decrease in the frequency of swallowing in the aspirating hospitalized patients. The frequency of spontaneous swallows can be easily sampled at bedside with simple instrumentation or palpation of the larynx to monitor elevation associated with the pharyngeal stage of the swallow. J. Murray et al. (1996) RLG A randomized control study to determine the effects of unlimited oral intake of water in patients with identified aspiration Small number: 20 patients with aspiration pneumonia. 10 with thick water 10 with “free water” Results: “No patient in either group developed pneumonia” Garon, B. et al. (1997) RLG Thick, “crusted” mucous throughout hypopharynx. Mucous appears moist and dispersed following hydration. (tsp. of water). RLG Predictors of Dysphagia Measured radiographically >70 years male gender disabling stroke (Barthel score <60) palatal weakness or assymetry incomplete oral clearance impaired pharyngeal response (cough/gurgle) Mann, G. & Hankey, G.J.(2001) RLG Clinical predictors of aspiration Measured radiographically delayed oral transit incomplete oral clearance Mann, G. & Hankey, G.J.(2001) RLG Tube feeding is associated with a higher rate of pneumonia than with patients who are eating. M.J. Feinberg, MD (1990) RLG Look to correlate frequency of pneumonia with prandial aspiration. Found there is not a simple relation between liquid aspiration and pneumonia. M.J. Feinberg, MD (1996) RLG Studied 152 SNF residents - average age of 86. Followed for 3 years. Begin of study 50 non aspirators 51 minor aspirators 51 major aspirators End of study 37 38 47 30 artificial feeding expired M.J. Feinberg, MD (1996) RLG SNF PATIENT (very elderly and/or frail) - RISK FACTORS Delayed recognition of pneumonia as signs and symptoms are subtle and different from younger individuals. Advanced age Difficult antibiotic treatment: difficult to identify pathogen altered drug metabolism medication side effects M.J. Feinberg, MD (1996) RLG SNF PATIENT - RISK FACTORS (cont’d) Dependency for feeding. Depressed and/or fluctuating levels of consciousness (medication and/or neurological disease). Microaspiration of oropharyngeal secretions that had been pathologically colonized overgrowth gram negative enteric rods associated with functional decline Anaerobic bacteria overgrowth secondary to gum disease or dentures M.J. Feinberg, MD (1996) RLG Pneumonia frequency was higher in months of artificial feeding. Patients with artificial feeding are at risk for aspiration of refluxed material. PEG’s/JEG’s do not help to protect those who are known to aspirate. M.J. Feinberg, MD (1996) RLG “Artificial feeding does not seem to be a satisfactory solution for preventing pneumonia in elderly prandial aspirators”. M.J. Feinberg, MD (1996) RLG Colonization (Altered Oropharyngeal Flora) Dependent for oral care Number of decayed teeth Number of medications Tube feeding Aspiration into lungs Large volume aspiration Microaspiration (liquid, food, GER, saliva) (saliva, plaque, GER) Dependent for feeding Host resistance Pulmonary clearance Now smoking Systemic Immunologic response Multiple Medical Diagnoses Langmore, S. (1997) RLG PNEUMONIA Pneumonia in acute stroke patients fed by nasogastric tube 100 consecutive patients with acute CVA (outcome was assessed at three months) Determine risk given the frequency of pneumonia in acute stroke patients fed by nasogastric tube. Identify variables significantly associated with the ocurrence of pneumonia and those related to a poor outcome. Dziewas R. et al, Jun 2004 RLG Pneumonia in acute stroke patients fed by nasogastric tube (cont’d) Results: Pneumonia was diagnosed in 44% of the tube fed patients. Most patients acquired pneumonia on the second or third day after stroke onset. Patients with pneumonia more often required endotracheal intubation and mechanical ventilation. Dziewas R. et al, Jun 2004 RLG Pneumonia in acute stroke patients fed by nasogastric tube (cont’d) Independent predictors Decreased level of consciousness Severe facial palsy. Conclusion Nasogastric tubes offer only limited protection against aspiration pneumonia in patients with dysphagia from acute stroke. Dziewas R. et al, Jun 2004 RLG 189 male veterans (55 outpatients), 41 or 21.7% developed pneumonia. (Bivariate analysis to determine predictive risk factors). Langmore, et al (1998) RLG “Dysphagia and aspiration are necessary but not sufficient conditions to predict development of aspiration pneumonia… a multifactorial phenomenon”. Langmore,S. (1998) RLG Focus on context of risk factors in given setting. Assess strengths/weaknesses. Langmore,S. et al(2000) RLG Predictors of aspiration pneumonia in nursing homes patients 102,842 patient 3,118 pneumonia = 3% suctioning use COPD CHF presence of feeding tube bedfast delirium weight loss swallowing problems UTI’s mechanically altered diet Langmore, S. et al. (2002) RLG Predictors of aspiration pneumonia in nursing homes patients (cont’d) dependence for feeding bed mobility locomotion number of medications age CVA tracheotomy care 1998 Predictors dependence for oral care smoking multiple medical diagnosis numerous decayed teeth Langmore, S. et al. (2002) RLG Impaired cough reflex in patients with recurrent pneumonia 7 Patients with recurrent pneumonia Capsaicin cough sensitivy 2-6 episodes of pneumonia Cough threshold was significantly higher in patients than in controls Conclusion: Impaired cough reflex may be involved in the pathogenesis of recurrent pneumonia. Niimi A., et al (2003) RLG What is a safe amount of aspiration? What is the long term consequence of chronic aspiration? What factors predict who will get pneumonia? RLG SCALE PREDICTIVENESS OF PNEUMONIA RISK IF FED FACTORS Multiple or progressive disease/one diagnosis Multiple medications (>5)/ <5 medications NPO (PEG)/ oral Oral hygiene fair – poor/ good – excellent Smoker / non-smoker RLG SCALE PREDICTIVENESS OF PNEUMONIA RISK IF FED (cont’d) FACTORS Inpatient / outpatient Physical ability (mobile)/ sedentary Reflexive cough (present) / absent – delayed Cognitive status (fair-poor)/ good – excellent Secretion Pooling (minimal) / copious RLG SCALE PREDICTIVENESS OF PNEUMONIA RISK IF FED (cont’d) Score < 7= 5–6= <3 = Use extreme caution fair – good good – excellent RLG Inpatient “sick” (acute/ exacerbation of chronic condition) + sedentary “bed rest/ bathroom privileges” number of medications multiple medical diagnosis. tube feeding dependent for oral care/ hygiene status dependent for feeding smoking RLG Outpatient may have multiple diagnosis; however, “stable” + mobility number of medications if tube feeding, bolus fed typically are not dependent for feeding smoking RLG Consensus VFSS and FEES/FEEST are good for identifying aspiration. However, identifying aspiration is not sufficient for predicting who will and who won’t develop pneumonia. Some chronic aspirators appear to fair quite well i.e. head and neck CA, hemilaryngectomees, supraglottic laryngectomees. Status of reflexive cough appears important. RLG SWALLOWING TREATMENT “The human body is one of the greatest compensatory mechanisms.” RLG GOAL: TARGET MOST CRITICAL RISK FACTORS. RLG TECHNIQUES OF DYSPHAGIA THERAPY A UNIQUE PATIENT POSTURES & POSITIONING STRENGTHENING - MENDELSOHN MANEUVER - E-STIM - SUPRAGLOTTIC SWALLOW - EMG - MODIFIED VALSALVA - ORAL MOTOR EXERCISES EXPECTORATION MANEUVER - BOLUS WEIGHT MANIPULATION OF CONSISTENCY TIMING PATIENT NUANCES - THICK - THICKER - THICKEST - RESPIRATORY CONTROL - WHEN TO SWALLOW - HOW MANY SWALLOWS - SEQUENCE - COGNITION - GENERAL HX. - COPD - ACTIVITY LEVEL RLG Timing of laryngopharyngeal events during swallow: an EMG perspective RLG Electrode Placement Genioglossus (GG) Superior pharyngeal constrictor (SPC) - Posterior pharyngeal wall below level of the soft palate, lateral to the midline Longitudinal muscles of the pharynx (LP) - Transorally in the midportion of the posterior tonsillar pillar McCulloch, T. (Voice, Swallow & Airway 2005) RLG Electrode Placement (cont’d) Thyroarytenoid (TA) - Local, transcutaneously, subjects phonated, at level to the cricothyroid membrane angle 30 degrees superior and 30 degrees medial to normal plane, verification maneuvers Cricopharyngeus (CP) - Local, transcutaneously at level of the cricothyroid membrane, needle advanced in a posterior and inferior direction, verification maneuvers McCulloch, T. (Voice, Swallow & Airway 2005) RLG Methods Five normal subjects (4 male, 1 female) Human subject approval Simultaneous endoscopy (fiberoptic endoscope, camera and video recorder) multichannel electromyography (hook wire electrodes, amplification, filtration, and on line monitoring) during swallow Time code generator (time lock endoscopic and electromyographic events) McCulloch, T. (Voice, Swallow & Airway 2005) RLG Instructions The supraglottic swallow - “Inhale and hold your breath - Swallow while holding your breath - Cough immediately after your swallow without breathing in” The Mendelsohn Maneuver - “Swallow your saliva several times and pay attention to your neck as you swallow - Now, when you swallow feel your Adam’s apple/voice box lift and lower - Swallow don’t let your Adam’s apple drop - Hold it up with your muscles for several seconds” McCulloch, T. (Voice, Swallow & Airway 2005) RLG Emphasis EMG of the cricopharyngeus (CP) during the Mendelsohn maneuver EMG of the thyroarytenoid (TA) and CP during the supraglottic swallow McCulloch, T. (Voice, Swallow & Airway 2005) RLG Muscle examined Superior pharyngeal constrictor (SPC) Tongue base (GG) Cricopharyngeus (CP) Thyroarytenoid (TA) McCulloch, T. (Voice, Swallow & Airway 2005) RLG Discussion A number of studies have concluded the Mendelsohn maneuver prolonges UES opening, these employed manometric recordings and videofluorgraphic evaluation. None have employed the use of simultaneous Studies have demonstrated that the UES diameter may increase with the use of swallowing maneuvers without increasing the duration of UES opening McCulloch, T. (Voice, Swallow & Airway 2005) RLG Discussion Traction of the anterior wall of the UES during the Mendelsohn may lead to a prolongation of opening of the UES, despite the resumption of tone in the Cricopharyngeus (CP) The study presented was that of normal volunteers, with normal swallowing function. We cannot predict the efficacy of these maneuvers on the head and neck patient who is status post anatomic and physiologic changes from neurologic/ surgical insults. In such patients these maneuvers may improve coordination of swallowing. McCulloch, T. (Voice, Swallow & Airway 2005) RLG Conclusions Swallowing is the result of a series of coordinated neuromuscular events. Certain aspects of swallowing may be superceded by volitional control. The thyroarytenoid (TA) activity in the supraglottic swallow and the Mendelsohn it is prolonged along the “tail” end of the swallow. McCulloch, T. (Voice, Swallow & Airway 2005) RLG Conclusions Cricopharyngeal quiescence is not prolonged by changes in swallowing maneuvers. The basic order of events swallowing is predetermined. The physical ends results may be modified by extraneous biomechanical forces. McCulloch, T. (Voice, Swallow & Airway 2005) RLG Conclusions We are able to eat, talk, breath and swallow like a great orchestra. Timing is everything. There is a delicate balance. The “escalation” neuromuscular patterns add to the efficiently of the system. It is no wander that patients with nearly any head or neck problem are at risk for dysphagia. McCulloch, T. (Voice, Swallow & Airway 2005) RLG IDEAL REALITY Instrumental exam for each patient. Coordinated team. Plenty of time. Medical experts making decisions. Salient/clear data presented. Treatment without exam. Piece meal. Little time. 3rd party payer control. Lengthy reports. Check lists-important information lost “in the trees”. RLG SOLUTIONS Assess your environment. Establish “partnership”/collaborative working relationships with instrumental source. “Trust and understand results”. Streamline reports. Highlight pertinent information. Foster open communication among practitioners. Focus on what you can do. “Prioritize”. Be resourceful. RLG RLG