Diapositiva 1
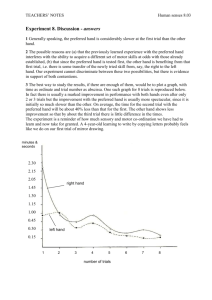
advertisement

National Institute for Infectious Diseases L. Spallanzani Roma, Italy Constrains and common mistakes in TB/MDR TB clinical trials Delia Goletti and Giovanni Sotgiu Borstel, May 28th, 2010 Agenda Trial organization Constraints related to TB-MDR trials Need for novel TB drugs and regimens Need for novel TB drugs and regimens that would: Time, shorten current treatment duration and/or allow more widely spaced intermittent treatment Amount of pills (10 or more at the moment) Avoid parental injection Safety and drug interaction especially in TB-HIV patients concurrently being treated for HIV infection TB drug trials have to be conducted to registration standards compliant with the International Conference on Harmonization (ICH) Good Clinical Practice (GCP) and Good Laboratory Practice (GLP) standards Agenda Trial organization Constraints related to TB-MDR trials Organization of a trial Phases of the clinical trials Phase Subjects enrolled Objective I Healthy donors Safety IIA Disease people Efficacy of the drug IIB Disease people Dosage III Disease people Control group. Ex: disease people under • gold standard therapy • placebo IV Disease people Efficacy of the drug, tolerability, safety Post-marketing Conduct of clinical trials A well conducted clinical trial must follow well defined steps in order to arrive at a valid result. These are : Initial design and protocol development Ethics Committee review Patients recruitment sites Treatment phase Follow-up phase Data analysis Publication of the results Section of the protocol. Initial design. Background and aims Specific objectives Trial design Eligibility criteria (including those ineligible) Trial endpoints (primary and secondary) Randomization procedure [sample, stratified, at cluster, systematic, at presentation] Treatment/intervention details (drug: dose, posology) Assessment of endpoints Follow-up procedures (physical examination, culture tests, blood tests) Statistical considerations including outline of analysis plan (comparative, equivalence; type of the statistical analysis: interim analysis for safety reasons) Procedure for handling adverse events, in particular serious adverse events Committee membership Appendices, including patient information sheet and consent form, tables with outlines of the protocol Site requirements-1 Sites with patients ! A stable population Common protocol Drug supplies Costs (indirect and direct) Site requirements-2 Organizational structure (outpatient service) Standardization Monitoring Mycobacteriology laboratory of high quality Facility for HIV testing and counseling Computing facilities Good Clinical Practice Data management Data entry Data analysis Statistical analysis (The results should not drive the analysis. Objectives are decided before the results are obtained) The rôle of the Central Coordinating Office Overseeing the development of the protocol Recruitment of the participating centres Training of the local staff Despatch of the drugs and study forms to the participating centres Randomisation Monitoring the conduct of the study Data management Site visits Organising the meetings of the Steering Committee Organising the meetings of the Data and Safety Monitoring Committee Dissemination of results Obtaining funds for each trial Agenda Trial organization Constraints related to TB-MDR trials Constraints of clinical trials for MDR-TB compared to trails for TB To generate homogeneous cohorts of patients with similar drug resistance using identical drugs main confounding variables (gender, age, co-morbidities, etc.) Severe clinical conditions Longer duration of treatment Drug toxicity more frequent per se and if concomitant HIV disease Drug-drug interactions (anti-TB and/or anti-HIV drugs) Sample size Common constraints of clinical trials Methodological issues Homogenous clinical management among the different sites Homogenous diagnostic work-up among the different sites Drug shortages Try to plan a clinical trial on a new anti-TB drug………. Trial justification. Ex: TB needs better treatment…. Trial objectives. Ex: shorten time of therapy , i.e. 4 months vs 6 months Treatment schedules. Ex: write the proposed schedule Trial endpoint: culture conversion rate, or other surrogate markers relapse rate (define the period: within a year, 2 years..) , time to death, changes in radiographic extent of disease and cavitation, urine tests for compliance, adverse events (stop the trial, etc.) Try to plan a clinical trial on a new anti-TB drug………. Statistical approach New regimen better than standard therapy New regimen equivalent than standard therapy Other… Publication (agreement on the PI, etc) Critical Path to New TB Regimens (CPTR) In March 2010 was launched Objective: to promote the development of new regulatory approaches that support innovative research into TB therapeutics and evaluate the safety and efficacy of new TB drugs combination Ex: to test regimens that include more than one experimental compound at a time, shifting the unit of development from individual TB drugs to entire regimens They are going to test 9-10 new TB drug regimens starting next year Spigelman et al, IJTLD June 2010 Try to plan a clinical trial on a new anti-TB drug………. Trial justification Trial objectives Treatment schedules Trial endpoint: Statistical approach Publication agrrement And thank you to: