Guidelines for Preventing the Transmission of M. tuberculosis in
advertisement

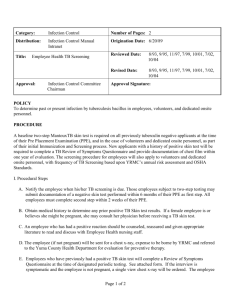
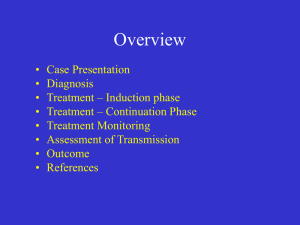
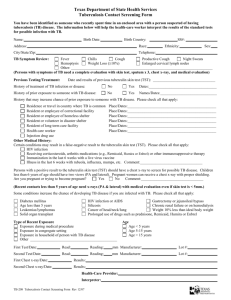
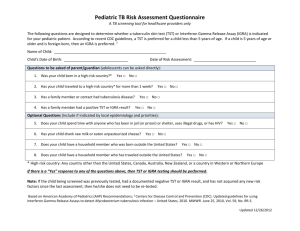
Infection Control: New CDC Guidelines Kevin Fennelly, MD, MPH 2006 Northeast TB Controllers Meeting Relapse? The State of TB Control in the Era of Declining Funds October 24, 2006 New Terminology Guidelines for Preventing the Transmission of M. tuberculosis in Health-Care Settings, 2005 MMWR 2005; 54 (RR-17): 1-147 • health-care-associated outbreaks Guidelines for Preventing the Transmission of M. tuberculosis in Health-Care Facilities, 1994 MMWR 1994; 43 (RR-13): 1-132 • nosocomial outbreaks • tuberculin skin tests • PPD (purified protein derivative) • airborne infection isolation room • respiratory isolation room • airborne precautions • TB infection control • BAMT: Blood assay for M. tuberculosis – IGRA: interferon gamma release assay • QFT-G: QuantiFERON-TB Gold test What’s New (1) • Change of risk classification and tuberculin skin test (TST) frequency • Expanded scope addressing lab, outpatient, and nontraditional settings • Expanded definitions of affected HCWs • “TST” instead of “PPD” Change in Risk Classifications Previous New • • • • • • Low • Medium • Potential ongoing transmission Minimal Very low Low Intermediate High Please refer to excellent presentation by Philip LoBue at Medical Consultants Meeting, September 20, 2006. -KF What’s New (2) • QuantiFERON-TB Gold test (QFT-G) • QFT-G is a type of blood assay for M. tuberculosis (BAMT) – Measures the patient’s immune system reaction to M. tuberculosis – Blood samples must be processed within 12 hours – Interpretation of QFT-G results is influenced by the patient’s risk for infection with M. tuberculosis – An alternative to TST TSTs vs. BAMTs for Surveillance of Exposure to Mtb • • • • • TSTs inexpensive assay Two visits Cost-effective? False+s (NTM & BCG) Allow for historical comparisons • Two products stable • Quantitative • • • • • BAMTs expensive: “NIMB” One visit Cost-effective? Eliminates false+s Uncertainty re: comparing to TST data • Newer versions will compete & confuse • Not quantitative: +/• Lack of technical experience and new problems – Notice regarding indeterminate results with the QuantiFERONTB Gold Test: CDC website, Oct 11, 2006 What’s New (3) • Term “airborne infection isolation” (AII) • Criteria for initiating and discontinuing AII precautions • Respirator fit testing and training; voluntary use of respirators by visitors • Additional information on ultraviolet germicidal irradiation (UVGI) • Frequently asked questions (FAQs) Prompt Triage Think TB! • Primary TB risk to HCWs is patient with undiagnosed or unrecognized infectious TB • Promptly initiate AII precautions and manage or transfer patients with suspected or confirmed TB – – – – Ask about and evaluate for TB Check for signs and symptoms Mask symptomatic patients Separate immunocompromised patients This is the Most Important Slide !!! -KF New Risk Factors for TB: Risk of Transmission ? • Treatment with immune modulators – Well-documented with TNF-alpha inhibitors – For rheumatoid arthritis & other collagen vascular diseases, Crohn’s disease, others • Organ transplantation • Immune reconstitution inflammatory syndrome (IRIS) Frequency of Sputum Collection for Patients with Suspected TB Disease • • • • Three negative sputum smears At least 8 hours apart At least one collected during early morning In most cases, patients with negative sputum smear results may be released from AII in 2 days Use sputum induction with history of no or scant sputum production ! -- KF Criteria for Discontinuing AII Precautions • Infectious TB is unlikely and another diagnosis is made that explains the syndrome Or • Patient has 3 consecutive negative AFB sputum smear results, and • Patient has received standard antituberculosis treatment (minimum of 2 weeks), and • Patient has demonstrated clinical improvement Discharge to Home • Patient can be discharged without 3 negative sputum smears if – Follow-up plan has been made with local TB program – Patient is on standard treatment and directly observed therapy (DOT) is arranged – And clinically improving with microbiological response (e.g., sputa AFB 4+ to 2 +); low suspicion of MDR-KF – No person in home <4 years old or immunocompromised *Recommend home visit!*-KF – All in household previously exposed – Patient willing to stay home until sputum results negative • Do not release if high-risk persons will be exposed IC Observations from a Consultant • Admin: Clinical suspicion for TB among primary care practitioners and specialists is highly variable. • Environ: Nursing staff need training & know who and when to call, esp in low-use settings. • PRP: Annual fit-testing is unsupported by data, onerous, costly & detracts from other efforts. – Need coordination within settings: lack of N95s to which HCWs are fit-tested. – Shortages of N95s due to SARS; expect with influenza. Summary • High index of suspicion remains most important TB IC measure. • Second most important is effective treatment: micro lab is critical part of IC. • Environ and PRP controls only work if infectious patients are identified – And if used properly!! • Key control measure in era of declining funds: EDUCATION! CDC Tuberculosis Guidelines: Highlights and Controversies 2000-2006 (excerpts related the Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Settings, 2005 ) Philip LoBue, MD Centers for Disease Control and Prevention Division of Tuberculosis Elimination September 20, 2006 Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in HealthCare Settings, 2005 • Published in 2005 • Broadening of scope • Revision of risk assessment • Screening of healthcare workers – Allows use of QFT-G in place of TST Broadening of Scope • The scope of settings in which the guidelines apply has been broadened to include laboratories and additional outpatient and nontraditional facilitybased settings • Examples – Dentist’s office – Home-based healthcare – Emergency medical services Health-care Setting Risk Assessment • Classifications: ongoing transmission, medium risk, low risk Ongoing Transmission • Evidence of transmission of M. tuberculosis between patients and/or HCW, occurring in the setting during the preceding year • Evidence of person-to-person transmission includes – Increased rates or clusters of TST or QFT-G conversions – HCW with confirmed TB disease – Unrecognized TB disease in patients or HCWs – Recognition of an identical strain of M. tuberculosis in patients or HCWs with TB disease identified by DNA fingerprinting Medium and Low Risk • Medium risk – Inpatient, at least 200 beds: 6 or more TB patients per year – Inpatient, less than 200 beds; outpatient; outreach; or home-based healthcare : 3 or more TB patients per year • Otherwise low risk TB Screening Procedures for Settings Classified as Potential Ongoing Transmission • Testing for infection with M. tuberculosis might need to be performed every 8–10 weeks until lapses in infection control have been corrected • “Ongoing transmission” should be used as a temporary classification only • Warrants immediate investigation and corrective steps • After a determination that ongoing transmission has ceased, the setting should be reclassified as medium risk for at least 1 year TB Screening Procedures for Settings Classified as Low Risk • All HCWs should receive baseline two-step TST or a single QFT-G upon hire • After baseline testing, additional TB screening is not necessary unless an exposure occurs • HCWs with a baseline positive or newly positive test or documentation of treatment for LTBI or TB disease should receive a CXR to exclude TB disease • Routine repeat CXRs are not needed TB Screening Procedures for Settings Classified as Medium Risk • All HCWs should receive baseline two-step TST or a single QFT-G upon hire • After baseline testing, HCWs should receive TB screening annually – Symptom screen for all HCWs – Single TST or QFT-G for HCWs with baseline negative test results • HCWs with a baseline positive or newly positive test or documentation of treatment for LTBI or TB disease should receive a CXR to exclude TB disease • Routine repeat CXRs are not needed Prevention and Control of Tuberculosis in Correctional and Detention Facilities • Published in 2006 • Risk assessment – different from healthcare settings • Screening Risk Assessment • A facility has minimal TB risk if – No cases of infectious TB have occurred in the facility in the last year – The facility does not house substantial numbers of inmates with risk factors for TB (e.g., HIV infection and injection-drug use) – The facility does not house substantial numbers of new immigrants (i.e., persons arriving in the US within the previous 5 years) from areas of the world with high rates of TB – Employees of the facility are not otherwise at risk for TB • Any facility that does not meet these criteria should be categorized as a nonminimal TB risk facility Screening: Minimal Risk Facilities • All inmates and detainees at intake: screening for symptoms and risk factors for TB • If no symptoms or risk factors, no further screening required • If risk factors present: TST or QFT-G or CXR within 7 days of arrival • If HIV-infected, HIV status unknown with risk factors for HIV, or other severe immunosuppression: CXR Screening: Nonminimal Risk Facilities • All inmates and detainees at intake: screening for symptoms AND TST or QFT-G or CXR within 7 days of arrival • If HIV-infected, HIV status unknown with risk factors for HIV, or other severe immunosuppression: CXR Additional Evaluation • If symptoms or abnormal CXR: evaluate for disease • If TST or QFT-G positive: CXR and evaluate for LTBI treatment once TB disease has been excluded and if completion of treatment is likely