embryo ch 2 and 3 [10-26
advertisement

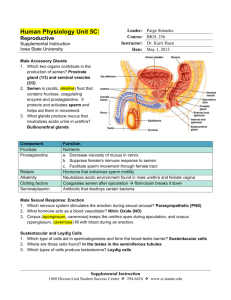
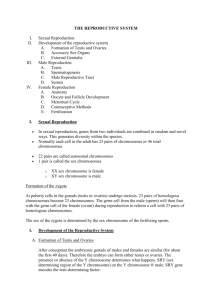
embryo ch 2 and 3 GENE EXPRESSION AND DIFFERENTIATION Gene expression regulated by o Different genes transcribed o DNA transcribed from gene selectively processed to regulate which RNAs become mRNA o mRNAs may be selectively translated o proteins made from mRNAs differently modified linker DNA – part of DNA linking that looped around histones – joins two nucleosomes promoter region binds RNA polymerase for initiation of transcription 3’ end has poly-A tail – 5’ end has TATA box Enhancers – regulatory elements of DNA that activate utilization of promoters to control efficiency and rate of transcription Nuclear RNA – nRNA – mRNA before introns come out Spliceosomes – snRNA that recognize and splice nRNA Splicing isoforms – proteins derived from same gene due to different splicing Competence – ability of responding tissue to respond to induction Paracrine interactions – proteins synthesized by one cell diffuse over short distances to interact with next cell Juxtacrine signaling – neighbor cells signal by touch, ligands in extracellular matrix secreted by one cell interact with another cell on matrix, or signals travel via gap junctions Paracrine signaling factors – also called growth and differentiation factors (GDFs) o Fibroblast growth factors (FGFs) – used for angiogenesis, axon growth, and mesoderm differentiation o Hedgehog proteins – desert, Indian, or sonic Sonic hedgehog is involved in limb patterning, somite differentiation, and gut regionalization o WNT proteins – frizzled family of proteins – limb patterning, midbrain development, some aspects of somite and urogenital differentiation GAMETOGENESIS Gametes derived from primordial germ cells (PGCs) formed in epiblast during 2nd week Germ cells undergo gametogenesis in preparation for fertilization – cytodifferentiation finishes it Teratoma – tumor in fetus or created by fetus that contains random parts of random tissue (hair, teeth, skin, gut, etc.) Linked genes – genes on the same chromosome Synapsis – metaphase I of meiosis Chiasma – structure of crossed chromosomes formed by crossing over 35 years of age and up in woman increases nondisjunction GENETIC DISORDERS Down Syndrome – trisomy 21 Trisomy 18 – intellectual disability, congenital heart defects, low-set ears, malformations of skeletal system – die very early (85% aborted spontaneously) Trisomy 13 – intellectual disability, eye and ear defects, cleft lip and palate, heart defects (90% die in first month after birth) Klinefelter syndrome – XXY Turner syndrome – only monosomy compatible with life – XO – 98% of these fetuses are spontaneously aborted – mostly caused by nondisjunction in male – no gonads at all Tripe X Syndrome – XXX – often go undiagnosed – often have speech problems – two Barr bodies Cri-du-chat Syndrome – deletion of short arm of chromosome 5 – small head, heart problems, intellectual disability, and cat-like cry Angelman’s syndrome – microdeletion on long arm of chromosome 15 – intellectual disability, cannot speak, poor motor movement, laugh for no reason – DELETION ON MATERNAL GAMETE Prader-Willi syndrome – microdeletion on long arm of chromosome 15 in PATERNAL GAMETE – obesity, intellectual disability, hypogonadism, hypotonia Miller-Dieker syndrome – deletion at 17p13 (first number is chromosome number, p for short arm or q for long arm, second number is gene number) – cardiac and facial abnormalities, developmental delay, seizures, lissencephaly (no cerebral folds) Fragile sites – regions of chromosomes with propensity to break or separate Fragile X syndrome – repeats of promoter region in Xq27 – intellectual disability, large ears, prominent jaw, large testes – second to Down syndrome as cause of intellectual disability OOGENESIS Oogenesis – once PGCs arrive in gonad of genetic female, they differentiate into oogonia Several mitotic divisions make oogonia become cluster of primary oocytes surrounded by epithelial cells (follicular cells) that originate from surface epithelium covering ovary Primary oocytes are arrested in prophase I and don’t continue until puberty Diplotene stage – resting stage during prophase characterized by lacy network of chromatin – held here by oocyte maturation inhibitor (OMI) Fewer than 500 oocytes are actually ovulated Each month, 15-20 follicles mature – some die before full maturity o These follicles accumulate fluid in the antrum o Essentially a race to the first to reach maturity Graafian follicle – mature vesicular follicle LH induces preovulatory growth phase when secondary follicle matures Polar bodies accumulate between zona pellucida and PM of secondary oocyte Oocyte arrested in metaphase II during ovulation and only completes if cell fertilized – degenerates about 24 hours after ovulation if not fertilized SPERMATOGENESIS Begins at puberty Type A spermatogonia Type B spermatogonia primary spermatocytes secondary spermatocytes spermatids spermatozoa Epithelium surrounds forming sperm – sustentacular cells (Sertoli cells) FSH – binds to Sertoli cells and stimulate testicular fluid production and synthesis of intracellular androgen receptors Spermiogenesis – process of spermatid becoming spermatozoa o Formation of acrosome o Condensation of nucleus o Formation of neck, middle piece, and tail o Shedding of most of cytoplasm as residual bodies About 300 million sperm produced daily Sperm obtain full motility in epididymis Spermatocytogenesis is process from spermatogonia to primary spermatocyte OVULATION TO IMPLANTION Gonadotropin-releasing hormone (GnRH) – produced by hypothalamus and signals anterior pituitary to release gonadotropins (FSH and LH) Corpus atreticum – connective tissue comprised of degenerating follicle and oocyte FSH stimulates follicles to grow and leave “egg nest” of primordial follicles o These become primary follicles o FSH also stimulates maturation of granulosa cells surrounding oocyte Theca interna cells produce androstenedione and testosterone – granular cells convert these to estrone and 17β-estradiol Estrogens produced by granular cell conversion cause o Uterine endometrium to enter follicular (proliferative) phase o Thinning of cervical mucus to allow sperm passage o Anterior lobe of pituitary gland stimulated to secrete LH Midcycle, an LH surge o Elevates concentrations of maturation-promoting factor, causing oocytes to complete meiosis I o Stimulates production of progesterone by follicular stromal cells (luteinization) o Causes follicular rupture and ovulation Mittelschmerz – pain felt during ovulation Ovulation generally accompanied by a rise in basal temperature Drugs can stimulate gonadotropin release to cause ovulation, but is 10x more likely to cause multiple pregnancy FSH and LH influence vesicular follicle to grow rapidly to become mature vesicular follicle (Graafian) – oocyte arrested in metaphase II about 3-12 hrs before ovulation Surface of ovary begins to bulge locally and at apex, avascular spot (stigma) appears High concentrations of LH increase collagenase activity, digesting collagen fibers surrounding follicle LH surge also increases prostaglandin levels, which cause local muscular contractions in ovarian wall to cause ovulation Corona radiata – formed from cumulus oophorous cells that come along for the ride during ovulation After ovulation, granulosa cells remaining in wall of ruptured follicle and cells from theca interna vascularized by surrounding vessels o Under influence of LH, these cells develop yellowish pigment and change to lutein cells, which form corpus luteum and secrete estrogens and progesterone Progesterone – along with some estrogen, causes uterine mucosa to enter progestational (secretory) stage Fimbriae of uterine tube sweep over surface of ovary while uterine tube undergoes peristalsis Once in uterine tube, cumulus cells withdraw cytoplasmic processes from zona pellucida and lose contact with oocyte Cilia in tubal mucosa help push oocyte along with peristalsis If fertilization does not occur, corpus luteum reaches max development about 9 days after ovulation o Yellowish projection on surface of ovary shrinks because of luteolysis and forms mass of fibrotic scar tissue (corpus albicans) o Progesterone production decreases, precipitating menstrual bleeding If fertilized, degeneration of corpus luteum prevented by human chorionic gonadotropin, secreted by syncytiotrophoblast of developing embryo Corpus luteum continues to grow and forms corpus luteum of pregnancy (corpus luteum graviditatis) o Continues to secrete progesterone until end of 4th month, then regress slowly as progesterone produced by trophoblastic component of placenta takes over o If corpus luteum removed before fourth month, fetus will most likely die Fertilization usually occurs in ampullary region of uterine tube, close to ovary Spermatozoa may remain viable in female reproductive tract for up to six days Only 1% of sperm deposited in vagina reach cervix – muscular contractions of uterus and uterine tube help them along – range in speed from 30 min to 6 days Once at isthmus, sperm become less motile and cease migration – at ovulation, sperm become motile again and swim to ampulla In order to fertilize oocyte, spermatozoa must undergo: o Capacitation – period of conditioning in female reproductive tract that take about 7 hours – involves epithelial interactions between sperm and mucosal surface of tube – glycoprotein coat and seminal plasma removed from acrosomal region o Acrosome reaction – induced by zona pellucida proteins culminating in release of enzymes needed to penetrate zona pellucida (acrosin and tripsin-like substances) Zona pellucida maintains sperm binding while inducing acrosome reaction – release of acrosin by acrosome allows penetration of zona pellucida Permeability of zona pellucida changes when head of sperm contacts oocyte PM because contact results in release of lysosomal enzymes from cortical granules lining PM of oocyte Zona reaction – zona pellucida going impenetrable and inactivating receptor sites on zona surface Initial adhesion of sperm to oocyte mediated by integrins on oocyte interacting with disintegrins on sperm Fusion accomplished between oocyte PM and PM covering posterior region of sperm head – head and tail enter oocyte leaving only PM behind, causing o Cortical and zona reactions – release of cortical oocyte granules that contain lysosomal enzymes o Resumption of meiosis – definitive oocyte arranges its chromosomes into female pronucleus o Metabolic activation of egg to initiate early embryogenesis Male pronucleus becomes prominent and tail disintegrates Pronuclei replicate DNA then undergo mitosis formation of morula CONTRACEPTIVE METHODS Hormonal – provide estrogen and/or progestin, inhibiting release of FSH and LH and thus preventing ovulation, changing lining of uterus and thickening cervical mucus Male “pill” – contains synthetic androgen that prevents LH and FSH secretion that stops sperm production or reduces it to level of infertility Intrauterine devices (IUDs) – T-shaped unit o Hormonal IUD – releases progestin that causes thickening of cervical mucus – may make sperm less active and egg and sperm less viable o Copper IUD – releases copper into uterus to prevent fertilization or attachment of fertilized egg to uterine wall – prevents sperm from entering uterine tubes Emergency contraceptive pills (ECPs) – taken within 120 hours of sex o High dose of progestin (with or without estrogen – combination with estrogen commonly called Plan B) o Antihormonal ECPs – i.e., mifepristone can act as abortifacient if egg already implanted INFERTILITY Problem for 15%-30% of couples Assisted reproductive technology (ART) – methods to help infertility o In vitro fertilization (IVF) – most common method to help infertility – gonadotropins used to bring follicle growth just shy of ovulation, then oocytes recovered via laproscopy and put in culture medium with sperm – zygote monitored to 8 cell stage and then placed in uterus to develop o Chances that these work drops with age of mother o End up in premature births and multiple pregnancies o Often can have birth defects Therapeutic cloning – take differentiated adult cell and introduce it to enucleated oocyte, which is then stimulated to form blastocyst, but is completely unviable – used for more ethical stem cell production Oligozoospermia – very few live sperm per ejaculation Azoospermia – no live sperm per ejaculation Intracytoplasmic sperm injection – sperm injected into egg to cause fertilization o Risk for Y chromosome deletions but no other chromosomal abnormalities IMPLANTATION L selectin on trophoblast cells and carbohydrate receptors on uterine epithelium mediate initial attachment Uterus wall o Endometrium – mucosa lining inside wall – place where fertilized egg attaches o Myometrium – thick layer of smooth muscle o Perimetrium – peritoneal covering lining outside wall Endometrium undergoes follicular phase until ovulation secretory (progestational phase) mensus (or implantation) o Endometrium shed during menstruation (compact and spongy layers) o Venules and sinusoidal spaces become packed with blood cells and extensive diapedesis of blood into tissue occurs o When menstruation begins, blood escapes from superficial arteries and small pieces of stroma and glands break away o Basal layer of endometrium remains – has its own arteries and functions as regenerative layer to rebuild compact and spongy layers Normally blastocyst implants in anterior or posterior wall Day 11-12 – new cells appear between inner surface of cytotrophoblast and outer surface of exocoelomic cavitiy – derived from yolk sac cells and form loose, fine connective tissue (extraembryonic mesoderm) – eventually fills all space between trophoblast and amnion and exocoelomic membrane o Extraembryonic somatic mesoderm – side lining cytotrophoblast and amnion o Extraembryonic splanchnic mesoderm – side covering yolk sac Sometimes around day 13, bleeding occurs around implantation site as a result of increased blood flow into lacunar spaces – can be confused for menses since around that time Extraembryonic mesoderm lining inside cytotrophoblast called chorionic plate when chorionic cavity forms Genomic imprinting – differential modification and/or expression of homologous alleles or chromosome regions depending on parent they got it from