2_Gram Positive Bacteria of Medical Importance
advertisement

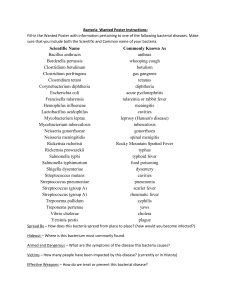
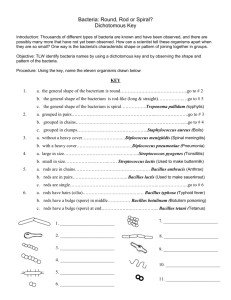
ZaidKhalid MBBS220 Gram Positive Bacteria of Medical Importance Intro on Gram Positive Bacteria 1. Has thick, multilayered cell wall composed of peptidoglycan 2. Peptidoglycan is important for a. Maintaining the structure of cell b. Replication c. Survival of bacteria at hostile environments 3. Other components of cell wall a. Techoic acid i. Water soluble ii. Covalently linked to peptidoglycan iii. Essential for cell viability iv. Important factors in virulence b. Lipotechoic acid i. Have fatty acid ii. Anchored to the plasma membrane iii. Common surface antigens to distinguish bacterial serotypes iv. Promote attachment to other bacteria or mammalian cell receptors c. Complex polysaccharides i. Also called as C polysaccharides ZaidKhalid MBBS220 COCCUS 2. Chains a. Streptococcus These two type can be differentiated thru CATALASE TEST 1. POSITIVE=STAPHYLOCOCCUS 2. NEGATIVE=STREPTOCOCCUS Aerobes/Facultative Anaerobes Categorized based on the arrangement 1. Cluster a. Staphylococcus aureus b. Staphylococcus epidermidis c. Staphylococcus saprophyticus b. Negative = need to be followed by Novobiocin test 2. Novobiocin test a. Sensitive =staphylococcus epidemidis b. Resistant=staphylococcus saprophyticus Staphylococcus (arranged in clusters) Identification of staphylococcus 1. Coagulase test a. Positive = staphylococcus aureus Name of bacteria Staphylococcus aurieus 1. Normal flora a. Skin b. Mucosal layer 2. Presence at anterior nares (50-75% of healthy individuals) Lab Characteristics Virulence factors Clinical diseases Treatment 1. Produces golden colony a. Orange to white 2. Positive in both a. Catalase test b. Coagulase test 3. Selective media a. 7.5% NaCl b. Mannitol salt agar 1. Capsule a. Inhibits i. Chemotaxis ii. Phagocytosis 2. Peptidoglycan a. Provides osmotic stability b. Stimulates the production of endogenous pyrogen/causing fever (like endotoxin) 3. Protein A a. Inhibit antibody mediated clearance b. Binds to IgG Fc receptor 4. Toxins a. Exfoliative toxins i. Splits IC bridges at SG of epidermis b. Enterotoxins i. Superantigens, promotes Toxic mediated diseases 1. Staphylococcus scalded skin syndrome (Ritter’s disease) a. Due to exfoliative toxins 2. Bullous(blister) impertigo (with pus) a. Localised form of SSSS b. Due to specific strains of toxin producing S.aurieus (phage type 71) 3. Staphylococcus food poisoning a. Intoxification by enterotoxin in foods 4. Toxic shock syndrome a. Initiated with the localised growth of toxin producing strains at i. Vagina ii. Wound b. Followed by the release of TSST-1 into the bloodstream 1. Antibiotic of choice a. Cloxacillin 2. MRSA (Methicillin Resistant Staphylococcus Aureus) a. Vancomycin b. Teicoplanin c. Fusidic acid ZaidKhalid MBBS220 Name of bacteria Lab Characteristics Staphylococcus Epidermidis 1. Present as normal flora 1. Negative in coagulase test 2. Sensitive to Novobiocin test proliferation of T cell, release cytokines c. Toxic Shock Syndrome Toxin-1 i. Superantigen 1. Causes the leakage of endothelial cells 5. Enzymes a. Coagulase i. Converts fibrinogen to fibrin b. Catalase i. Catalyzes the removal of hydrogen peroxide c. Hyaluronidase i. Hydrolyses hyaluronic acid in connective tissue d. Fibrinolysin i. Dissolves fibrin clot e. B-lactamase i. Hydrolyses B-lactam antibiotic Suppurative/Pyogenic infection 1. Impetigo 2. Folliculitis 3. Furunculosis 4. Carbuncles 5. Wound infection Virulence factors Clinical diseases Treatment Much lower pathogenicity and rarely causes disease in healthy individuals Slime is the virulence factor 1. Enables the bacteria to adhere to medical instrument especially a. Urinary catheter b. Prosthetic heart valve 1. Catheter-associated infection 2. Prosthetic heart valve endocarditis 3. Infection of orthopaedic prosthesis (implant) 3. Antibiotic of choice a. Cloxacillin 4. MRSE (MultiResistant Staphylococcus Epidermidis) a. Vancomycin b. Fusidic acid Systemic infection 1. Pneumonia 2. Pyemia 3. Septic arthritis 4. Osteomyelitis 5. Endocarditis ZaidKhalid MBBS220 Streptococcus (arranged in chains) 1. Most are facultative anaerobes 2. Some only grow in atmosphere enhanced with CO2 (capnophillic growth) Biochem classification Serologic classification Streptococcus pyogenes A Streptococcus agalactiae B Streptococcus dysgalatiae C,G Streptococcus bovis D Viridians group streptococci Non-groupable Streptococcus pneumonia Non-groupable Name of bacteria Lab Characteristics Streptococcus pyogenes 1. Chains a. Short chains at medical specimens b. Long chain in liquid media 2. Enriched media of blood agar a. Optimal growth b. Large zone of beta haemolysis 3. Catalase negative 4. Sensitive to bacitracin Haemolysis pattern Beta (B) Beta (B), occasionally non-haemolytic Beta Alpha (A), non-haemolytic, occasionally Beta Alpha (A) or non-haemolytic Alpha (A) Virulence factors Clinical diseases Treatment 1. Capsule a. Anti-phagocytosis 2. Lipothecoic acid a. Binds to epithelial cells 3. M protein a. Adhesin b. Antiphagocytic 4. Pyrogenic exotoxins a. Acts as superantigen b. Types i. Spe A ii. Spe B iii. Spe C 5. Streptolysin S a. Lyses i. Leukocytes ii. Platelets iii. Erythrocytes Suppurative/pyogenic streptococcal diseases 1. Pharyngitis a. Sore throat 2. Scarlet fever a. Complication of pharyngitis occurs when infecting strain is lysogenized by temperate bacteriophage i. Stimulates the release of pyrogenic exotoxin 3. Impetigo a. Confined purulent happens only on exposed areas i. Arms ii. Face iii. Legs b. Vesicles develop and turn to pustules; rupture to produce 1. Penicillin 2. Pts with penicillin allergic a. Erythromycin b. Cephalosporin ZaidKhalid MBBS220 b. Stimulates release of lysosomal enzyme i. Non-immunologic 6. Streptolysin O a. Lyses i. Leukocytes ii. Platelets iii. Erythrocytes b. Stimulates release of lysosomal enzyme i. Immunologic 7. Streptokinase a. Lyses blood clot b. Facilitate spread of bacteria in tissue 8. DNAase a. Depolymerizes cell-free DNA in purulent material crust c. Primarily seen in young children 4. Erysipelas (acute cellulitis) a. Acute infection of the skin b. Local pain c. Inflammation d. Lymph node enlargement e. systemic signs i. chills ii. fever iii. leukocytosis 5. Cellulitis a. Involves the skin and deeper subcutaneous tissues 6. Necrotizing fasciitis a. Infection occurs deep in subcutaneous layer b. Spreads along the fascial plane c. Characterized by extensive destruction of muscle and fat 7. Streptococcal toxic shock syndrome a. Involves multiple organs; kidneys, lungs, heart and liver Non-suppurative streptococcal diseases 1. Rheumatic fever a. Inflammatory of heart, joints, blood vessels and SC tissues 2. Acute glomerular nephritis a. Inflammation of renal glomeruli with oedema, HPT, hematuria and proteinuria ZaidKhalid MBBS220 Name of bacteria Streptococcus agalactiae 1. Colonizes a. GIT b. GUT 2. Transient vaginal carriage found in 10-30% of pregnant women Lab Characteristics 1. The only species that has B antigen 2. Produces a narrow zone of Betahaemolysis Virulence factors 1. B antigen 2. Type-specific capsular polysaccharides a. Ia b. Ib c. II d. VII Clinical diseases Most infections in newborns are acquired from mother; pregnancy/delivery Neonates at high risk 1. Premature ruptures of membrane 2. Long labours 3. Preterm delivery 4. Disseminate maternal group B streptococcal disease 5. Mother without type-specific antibody/low compliment levels Early onset neonatal disease 1. Younger than 7 days of age 2. Characterized by a. Bacteremia b. Pneumonia c. Meningitis Late onset neonatal disease 1. 1week-3 months of life 2. Exogenous source a. Mother b. Other infant 3. Bacteremia with meningitis Other group B streptococcus infections 1. Urinary tract infection 2. Wound infection 3. Bacteremia Treatment 1. Penicillin alone 2. Penicillin plus aminoglycosides for serious infection ZaidKhalid MBBS220 Name of bacteria Streptococcus pneumonia 1. Commonly known as pneumococcus 2. Encapsulated coccus arranged in pairs or short chains Lab Characteristics 1. Appear alphahaemolytic on blood agar a. Production of pneumolysin, degrades haemoglobin 2. Can be differentiated from S. Viridans a. Sensitive to Optochin b. Soluble in bile solubility test c. Quellung reaction i. Polyvalent anticapsular antibodies will show swelling of the capsule Virulence factors 1. Capsule a. Antiphagocytic 2. Secretory Ig A protease a. Disrupts secretory IgAmediated clearance 3. Pneumolysin a. Able to destroy ciliated epithelial cells b. Activates classic complement pathway 4. Teichoic acid a. Activates alternative compliment pathway Clinical diseases 1. Pneumonia a. Most common causes of community acquired disease 2. Sinusitis and otitis media a. Most common causes infections at sinuses and ear b. Preceded by viral infection of upper respiratory tract 3. Meningitis a. Most common at any age except neonate 4. Bacteraemia a. Pneumonia i. 25-30% of pts b. Meningitis i. More than 80% of pts Treatment 1. Penicillin is the DOC 2. Penicillin allergic pts a. Cephalospori n b. Vancomycin c. Erythromycin 3. Immunization with 23-valent pneumococcal vaccine can prevent the infection ZaidKhalid MBBS220 Name of bacteria Viridan streptococci Colonizes : 1. Oropharynx 2. GIT 3. GUT Most isolates do not possess a group specific carbohydrate Name of bacteria Enterococcus sp Colonizes GIT Most common to be isolated are 1. Enterococcus faecium 2. Enterococcus faecalis Lab Characteristics Virulence factors Collection of 1. Alpha-haemolytic 2. Non-haemolytic Clinical diseases 1. Dental carries 2. Infective endocarditis 3. Intra-abdominal infections Treatment Ampicillin Resistance to Optochin Some strains are nutritionally deficient, needing presence of exogenous pyridoxal vitB6 Lab Characteristics Arranged in pairs or short chains Often confused with pneumococcal Virulence factors 1. Most infections originate from normal flora 2. Pts who at risk a. Prolonged hospitalization b. Use of broad-spectrum of antibiotic i. Cephalosporin, resistant to this drug Clinical diseases 1. Urinary tract infection 2. Wounds infection a. Intra-abdominal, usually polymicrobial 3. Bacteraemia 4. Endocarditis Treatment Ampicillin ZaidKhalid MBBS220 BACILLUS Aerobes/facultative anaerobes 1. Categorized based on ability to form spore a. Spore forming i. Bacillus Bacillus spp 1. Spore forming gram-positive bacilli 2. Clinically important species Name of bacteria Bacillus anthracis 1. Spore forming 2. Causative agent of anthrax Considered to be one of the most feared biological warfare Bacillus cereus 1. Ubiquitous (found everywhere) 2. Non-fastidious 3. Spore forming bacteria b. i. ii. iii. a. b. Non-sporing Corynebacterium Listeria Nocardia Bacillus anthracis Bacillus cereus Virulence factors Clinical diseases 1. Capsule is present in virulent strains 2. Virulent strains produce 3 exotoxins that combine to form a. Edema toxin i. Protective antigen + edema factor b. Lethal toxin i. Protective antigen + lethal factor 3. Spores can survive in soil for years 1. Cutaneous anthrax a. Most common form b. Starts with painless papules at site of inoculation c. Rapid progress to an ulcer surrounded by vesicles d. Later become necrotic eschar 2. Inhalation anthrax a. Most deadly form b. Progress to shock and death within 3 days of initial symptoms 3. Gastrointestinal anthrax a. Rare case b. Commonly fatal disease i. Mortality of up to 100% 1. Gastroenteritis a. Emetic forms b. Diarrhoea forms 2. Ocular infection following trauma in the eye 3. Other opportunistic infection a. IV catheter-related sepsis 1. Enterotoxins a. Heat-stable i. Causes emetic b. Heat-labile i. Causes diarrhoea 2. Cytotoxic enzymes a. Cereolysin-potent haemolysin b. Phospholipase C Treatment 1. DOC: ciprofloxacin 2. Alternative antibiotics a. Penicillin b. Chloramphenicol c. Doxycycline d. Erythromycin 3. Vaccination can control the spread of the disease 4. Spores are difficult to destroy ZaidKhalid MBBS220 Anaerobes Bacillus 4. Remarkable capacity of clostridia to cause disease is because a. Capable to survive at adverse environment by forming spore b. Rapidly grow at enriched nutrition, deprived oxygen c. Production of numerous i. Histolytic toxins ii. Enterotoxins iii. Neurotoxins Clostridium sp 1. Spore forming 2. Ubiquitous 3. Recognized harmful pathogens a. Clostridium perfringes b. Clostridium tetani c. Clostridium botulinum d. Clostridium deficile Name of bacteria Lab Characteristics Clostridium perfringes 1. Large rectangular 1. Forms spores 2. Produces double zone haemolysis on blood agar a. Alpha toxins b. Delta toxins 3. Nagler’s reaction a. Opalescence is seen when toxins act with egg yolk medium Virulence factors Clinical diseases Treatment 1. α toxins a. Lethal toxin phospholipase C b. Increase vascular permeability c. Haemolysin produces necrotizing activity 2. β toxins a. Lethal toxin-necrotizing activity 3. θ toxins a. heat and oxygen labile haemolysin-cytolytic 4. Enterotoxins a. Alter membrane permeability i. Cytotoxic ii. Enterotoxic 5. Neuramidase a. Alters cell surface ganglioside receptors b. Promotes capillary thrombosis 1. Soft tissue infections a. Cellulitis b. Suppurative myositis c. Myonecrosis d. Gas gangrene 2. Food poisoning a. Short incubation period (824hrs) b. Abdominal cramps c. Watery diarrhoea d. Nausea/emesis e. No fever f. Last less than 24 hrs 3. Necrotizing enteritis a. Abdominal pain b. Bloody diarrhoea c. Shock d. Peritonitis c. Caused by β toxins C.perfringes C 6. Septicaemia 1. Immediate treatment is vital for serious infection 2. Systemic infection requires surgical procedure 3. High dose of penicillin should also be employed ZaidKhalid MBBS220 Name of bacteria Clostridium tetani 1. Ubiquitous 2. Found in most soil 3. GIT humans and animals 4. Obligate anaerobes 5. Spores shape like a drumstick Clostridium botulinum 1. Agent of botulism 2. Spore forming, fastidious organism 3. 7 antigenically distinct botulinum toxins a. A to G b. A,B, E and F are pathogenic to human Virulence factors 1. Spore formation 2. Production of enzymes 3. Production of toxins a. Tetanolysin i. Oxygen labile haemolysin ii. Plasmid encoded b. Tetanospasmin i. Heat labile neurotoxin ii. Responsible for tetanus iii. Block neurotransmitter for inhibitory synapses, thus excitatory synaptic activity is unregulated (spastic paralysis) 1. Spore formation 2. Production of toxins a. Botulinum toxins i. Prevents the release of neurotransmitter acetylcholine b. Binary toxin i. Disrupts vascular permeability Clinical diseases 1. Tetanus 1. Food-borne botulism a. Blurred vision with fixed dilated pupils b. Dry mouth (anti cholinergic activity of the toxins) c. Constipation d. Abdominal pain e. Fever is absent f. Flaccid paralysis g. Death associated with respiratory paralysis 2. Infant botulism a. Caused by neurotoxin 3. Wound botulism Treatment 1. Requires debridement 2. Antibiotic therapy a. Penicillin b. Metronidazole 3. Passive immunization a. Antitoxin globulin 4. Vaccination a. Tetanus toxoid ZaidKhalid MBBS220 Name of bacteria Clostridium difficile 1. Ubiquitous organism 2. Spore forming 3. Strict anaerobes 4. Exposure to antibiotic is associated with overgrowth of C. difficile thus resulting in subsequent disease (endogenous infection) Virulence factors 1. Spore formation a. Permits organism to survive months in the hospital environment 2. Enterotoxin A a. Produces chemotaxis b. Induces cytokine c. Produces hypersecretion of fluid d. Produces haemorrhagic necrosis 3. Cytotoxin B a. Induces depolymerisation of actin with loss of cellular cytoskeleton Clinical diseases 1. Antibiotic-associated diarrhoea 2. Pseudomembranous colitis Treatment 1. Implicated antibiotic should be discontinued 2. Severe disease a. Vancomycin b. Metronidazole ZaidKhalid MBBS220 Aerobes Bacillus/ non-sporing Name of bacteria Corynebacteriu m diptheriae 1. Pleomorphic 2. Causative agent of diphtheria Lab Characteristics Virulence factors 1. Albert satin a. Metachromic granules within cell may be visible 2. Potassium tellurite agar a. Black colonies are seen 3. Elek test a. Toxin and antitoxin combine to form antigenantibody complexes b. Form precipitation on the agar in the form of visible lines 1. Exotoxin a. Tox gene that codes for the toxins is introduced by lysogenic bacteriophage b. Inhibits protein synthesis by inactivating the elongation factor 2 c. Can be detected thru Elek test Clinical diseases 1. Diphtheria a. Onset is sudden b. Malaise c. Sore throat d. Exudative pharyngitis e. Low-grade fever 2. Exudates evolve into thich pseudomembrane which composed of a. Bacteria b. Lymphocytes c. Plasma cells d. Fibrin e. Dead cells Can extend from nasopharynx or down to the larynx Treatment 1. Early use of antitoxin to neutralize the toxin 2. Erythromycin to kill the corynebacterium thus preventing excretion of exotoxin 3. Admin of diphtheria vaccine and booster to susceptible population ZaidKhalid MBBS220 Coccobacilus gram positive Name of bacteria Listeria monocytogenes 1. Facultative anaerobes 2. Motile at room temperature 3. Isolated form soil, veggie and water Lab Characteristics 1. Weak beta haemolytic 2. Capable of growing at 4oc a. Increase number when contaminated food is refrigerated Clinical diseases 1. Associate with consumption of contaminated food a. Soft cheese b. Milk c. Raw veggie 2. Transplacental spread from mother to neonate 3. Neonatal infection a. Bacteraemia b. Meningitis c. Meningoencephalitis 4. Adult infection a. Mild-influenza like illness b. Primary bacteraemia c. Meningitis Treatment 1. Severe infection a. Ampicillin b. Combine with gentamicin